Phase I Pharmacokinetic Study of Belinostat for Solid Tumors and Lymphomas in Patients with Varying Degrees of Hepatic Dysfunction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Company Coverage Report
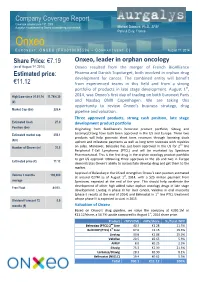
Company Coverage Report th Coverage initiated June 19 , 2009 Aurgalys is contracted by Onxeo to provide equity research Mickael Dubourd, Ph.D., SFAF Paris & Evry, France Onxeo E URONEXT : ONXEO [FR0010095596 – C OMPARTMENT C] August 1st, 2014 Share Price: €7.19 Onxeo, leader in orphan oncology (as of August 1st, 2014) Onxeo resulted from the merger of French BioAlliance Estimated price: Pharma and Danish Topotarget, both involved in orphan drug development for cancer. The combined entity will benefit €11.12 from experienced teams in this field and from a strong portfolio of products in late stage development. August 1st, High/Low since 01.01.14 11.74/4.30 2014, was Onxeo’s first day of trading on both Euronext Paris (€) and Nasdaq OMX Copenhagen. We are taking this opportunity to review Onxeo’s business strategy, drug Market Cap (€m) 226.4 pipeline and valuation. Three approved products, strong cash position, late stage Estimated Cash 27.0 development product portfolio Position (€m) Originating from BioAlliance's historical product portfolio, Sitavig and Estimated market cap. 350.1 Loramyc/Oravig have both been approved in the US and Europe. These two products will help generate short term revenues through licensing deals (€m) upfront and milestone payments as well as long term revenues with royalties nd Number of Shares (m) 31.5 on sales. Moreover, Beleodaq has just been approved in the US for 2 line Peripheral T-Cell Lymphoma (PTCL) and will be marketed by Spectrum Pharmaceutical. This is the first drug in the orphan oncology product portfolio to get US approval. -

Vorinostat—An Overview Aditya Kumar Bubna
E-IJD RESIDENTS' PAGE Vorinostat—An Overview Aditya Kumar Bubna Abstract From the Consultant Vorinostat is a new drug used in the management of cutaneous T cell lymphoma when the Dermatologist, Kedar Hospital, disease persists, gets worse or comes back during or after treatment with other medicines. It is Chennai, Tamil Nadu, India an efficacious and well tolerated drug and has been considered a novel drug in the treatment of this condition. Currently apart from cutaneous T cell lymphoma the role of Vorinostat for Address for correspondence: other types of cancers is being investigated both as mono-therapy and combination therapy. Dr. Aditya Kumar Bubna, Kedar Hospital, Mugalivakkam Key Words: Cutaneous T cell lymphoma, histone deacytelase inhibitor, Vorinostat Main Road, Porur, Chennai - 600 125, Tamil Nadu, India. E-mail: [email protected] What was known? • Vorinostat is a histone deacetylase inhibitor. • It is an FDA approved drug for the treatment of cutaneous T cell lymphoma. Introduction of Vorinostat is approximately 9. Vorinostat is slightly Vorinostat is a histone deacetylase (HDAC) inhibitor, soluble in water, alcohol, isopropanol and acetone and is structurally belonging to the hydroxymate group. Other completely soluble in dimethyl sulfoxide. drugs in this group include Givinostat, Abexinostat, Mechanism of action Panobinostat, Belinostat and Trichostatin A. These Vorinostat is a broad inhibitor of HDAC activity and inhibits are an emergency class of drugs with potential anti- class I and class II HDAC enzymes.[2,3] However, Vorinostat neoplastic activity. These drugs were developed with the does not inhibit HDACs belonging to class III. Based on realization that apart from genetic mutation, alteration crystallographic studies, it has been seen that Vorinostat of HDAC enzymes affected the phenotypic and genotypic binds to the zinc atom of the catalytic site of the HDAC expression in cells, which in turn lead to disturbed enzyme with the phenyl ring of Vorinostat projecting out of homeostasis and neoplastic growth. -

National Cancer Institute Cancer National
DIVISION OF CANCER TREATMENT AND DIAGNOSIS National Cancer Institute Cancer National PROGRAM ACCOMPLISHMENTS 2006 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health TABLE OF CONTENTS Foreword . iii Division of Cancer Treatment and Diagnosis Overview . .1 Major Ongoing Initiatives and Accomplishments . .7 Biometric Research Branch Overview . 11 Partnerships and Collaborations . 12 Scientific Advances . 17 Other Biostatistical Research . 24 Tools, Products, and Resources . 27 Cancer Diagnosis Program Overview . 29 Major Ongoing Initiatives . 30 Current Funding Opportunities . 34 Partnerships and Collaborations . 36 Scientific Advances . 39 Tools, Products, and Resources . 41 Cancer Imaging Program Overview . 45 Major Ongoing Initiatives . 47 Current Funding Opportunities . 54 Partnerships and Collaborations . 57 Scientific Advances . 61 Tools, Products, and Resources . 63 Cancer Therapy Evaluation Program Overview . 65 Major Ongoing Initiatives . 67 Significant Ongoing Clinical Trials . 71 Current Funding Opportunities . 73 Partnerships and Collaborations . 75 Scientific Advances . 79 Tools, Products, and Resources . 92 TABLE OF CONTENTS ■ i Developmental Therapeutics Program Overview . 95 New Initiatives . 97 Major Ongoing Initiatives . .100 Current Funding Opportunities . .104 Tools, Products, and Resources . .105 History-Marking Event . .114 Scientific Advances . .115 Radiation Research Program Overview . .119 Partnerships and Collaborations . .121 Scientific Advances . .127 Tools, Products, and Resources . .129 -

Peripheral T-Cell Lymphomas
Critical Reviews in Oncology/Hematology 99 (2016) 214–227 CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Contents lists available at ScienceDirect Critical Reviews in Oncology/Hematology jo urnal homepage: www.elsevier.com/locate/critrevonc Panoptic clinical review of the current and future treatment of relapsed/refractory T-cell lymphomas: Peripheral T-cell lymphomas a,∗ b c c d Pier Luigi Zinzani , Vijayveer Bonthapally , Dirk Huebner , Richard Lutes , Andy Chi , e,f Stefano Pileri a Institute of Hematology ‘L. e A. Seràgnoli’, Policlinico Sant’Orsola-Malpighi, University of Bologna, Via Massarenti 9, 40138 Bologna, Italy b 1 Global Outcomes and Epidemiology Research (GOER), Millennium Pharmaceuticals Inc., 40 Lansdowne Street, Cambridge, MA 02139, USA c 1 Oncology Clinical Research, Millennium Pharmaceuticals Inc., 35 Lansdowne Street, Cambridge, MA 02139, USA d 1 Department of Biostatistics, Millennium Pharmaceuticals Inc., 40 Lansdowne Street, Cambridge, MA 02139, USA e Department of Experimental, Diagnostic, and Specialty Medicine, Bologna University School of Medicine, Via Massarenti 8, 40138 Bologna, Italy f Unit of Hematopathology, European Institute of Oncology, Via Ripamonti 435, 20141 Milan, Italy Contents 1. Introduction . 214 2. Methodology. .215 3. Treatment of relapsed/refractory PTCL . 215 3.1. Conventional chemotherapy in relapsed/refractory PTCL. .215 3.2. Approved therapies in relapsed/refractory PTCL . 216 3.3. Investigational and off-label therapies in relapsed/refractory PTCL . 222 4. Concluding remarks . 224 Conflict of interest . 224 Funding . 224 Acknowledgments. .224 References . 224 Biography . 227 a r t i c l e i n f o a b s t r a c t Article history: Peripheral T-cell lymphomas (PTCLs) tend to be aggressive and chemorefractory, with about 70% of Received 29 June 2015 patients developing relapsed/refractory disease. -

Belinostat Phase II Trial Initiated in Platinum-Resistant Ovarian Cancer by the Gynecologic Oncology Group (GOG) Supported by the National Cancer Institute (US)
To NASDAQ OMX Copenhagen A/S TopoTarget A/S Announcement No. 01-10 / Copenhagen, January 6 2010 Symbion Fruebjergvej 3 DK 2100 Copenhagen Denmark Tel: +45 39 17 83 92 Fax: +45 39 17 94 92 CVR-nr: 25695771 www.topotarget.com Belinostat phase II trial initiated in platinum-resistant ovarian cancer by the Gynecologic Oncology Group (GOG) supported by the National Cancer Institute (US) Copenhagen, Denmark – January 6, 2010 – TopoTarget A/S (OMX: TOPO) announced today that GOG (The Gynecologic Oncology Group, US) has initiated a phase II trial evaluating efficacy and safety of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube or peritoneal cancer. GOG receives support for this trial from the National Cancer Institute (NCI) of the National Institutes of Health (NIH). “Positive efficacy and safety data with belinostat and carboplatin and paclitaxel (BelCaP) in patients with platinum resistant ovarian cancer have previously been announced by TopoTarget. We are very pleased that GOG now initiates this phase II study with belinostat and carboplatin (BelCar) in this difficult to treat patient population. Platin-resistance is a huge unsolved clinical problem in relapsing ovarian cancer and hopefully GOG will be able to show that BelCar, without additional paclitaxel is active in the platinum resistant setting.” said MD., Professor Peter Buhl Jensen, CEO of TopoTarget “ if GOG is able to repeat our initial positive results in platinum resistant patients we hope to advance into pivotal trials.” The study A Phase II evaluation of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal cancer. -

Belinostat (Beleodaq®)
Belinostat (Beleodaq®) Belinostat (Beleodaq®) Pronounced: be-lin-oh-stat Classification: Histone Deacetylase Inhibitor About Belinostat (Beleodaq®) Belinostat is in a class of anti-cancer therapies called histone deacetylase (HDAC) inhibitors. Histone deacetylation is a biochemical process that is thought to play a role in promoting tumor growth. It does this by silencing some tumor suppressor genes, as well as other genes that are responsible for cell cycle progression, cell proliferation, programmed cell death (apoptosis), and differentiation (transformation of young cells into specialized cells). Therefore, blocking histone deacetylation may allow the body to block tumor growth and prevent progression. How to Take Belinostat Belinostat is given by intravenous (IV, into a vein) infusion. The dose and how often you receive this medication is based on your weight and will be decided by your provider. Your dose may be reduced if you are having severe side effects. Possible Side Effects of Belinostat There are a number of things you can do to manage the side effects of belinostat. Talk to your care team about these recommendations. They can help you decide what will work best for you. These are some of the most common or important side effects: Nausea and/or Vomiting Talk to your oncology care team so they can prescribe medications to help you manage nausea and vomiting. In addition, dietary changes may help. Avoid things that may worsen the symptoms, such as heavy or greasy/fatty, spicy or acidic foods (lemons, tomatoes, oranges). Try saltines, or ginger ale to lessen symptoms. Call your oncology care team if you are unable to keep fluids down for more than 12 hours or if you feel lightheaded or dizzy at any time. -

Histone Deacetylase Inhibitors
ANTICANCER RESEARCH 36 : 5019-5024 (2016) doi:10.21873/anticanres.11070 Review Histone Deacetylase Inhibitors: A Novel Therapeutic Weapon Αgainst Medullary Thyroid Cancer? CHRISTOS DAMASKOS 1,2* , SERENA VALSAMI 3* , ELEFTHERIOS SPARTALIS 2, EFSTATHIOS A. ANTONIOU 1, PERIKLIS TOMOS 4, STEFANOS KARAMAROUDIS 5, THEOFANO ZOUMPOU 5, VASILIOS PERGIALIOTIS 2, KONSTANTINOS STERGIOS 2,6 , CONSTANTINOS MICHAELIDES 7, KONSTANTINOS KONTZOGLOU 1, DESPINA PERREA 2, NIKOLAOS NIKITEAS 2 and DIMITRIOS DIMITROULIS 1 1Second Department of Propedeutic Surgery, “Laiko” General Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 2Laboratory of Experimental Surgery and Surgical Research N.S. Christeas, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 3Blood Transfusion Department, Aretaieion Hospital, Medical School, National and Kapodistrian Athens University, Athens, Greece; 4Department of Thoracic Surgery, “Attikon” General Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 5Medical School, National and Kapodistrian University of Athens, Athens, Greece; 6Colorectal Department, General Surgery, The Princess Alexandra Hospital NHS Trust, Harlow, U.K.; 71st Department of Pathology, School of Medicine, University of Athens, Athens, Greece Abstract. Background/ Aim : Medullary thyroid cancer (MTC) is and histone deacetylase (HDAC) seems to play a potential role highly malignant, metastatic and recurrent, remaining generally to gene transcription. On the -

Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU
Topotarget A/S - Spectrum Pharmaceuticals, Inc. Module 5 Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU 2 SYNOPSIS NAME OF COMPANY: Individual Study Table (FOR NATIONAL AUTHORITY Topotarget A/S, CuraGen, and Spectrum Referring to Part of the USE ONLY) Pharmaceuticals, Inc. Dossier: NAME OF FINISHED PRODUCT: Belinostat Injection 50 mg/mL Volume: NAME OF ACTIVE INGREDIENT: Belinostat (PXD101) Page: TITLE OF STUDY: A Phase 1/2 Safety, Pharmacodynamic, and Pharmacokinetic Study of Intravenously Administered PXD101 Plus Carboplatin or Paclitaxel or Both in Patients with Advanced Solid Tumors INVESTIGATORS: Coordinating Investigator (Site 001): Dr. Ulrik Lassen, Department of Oncology, The Finsen Center, Copenhagen University Hospital, Copenhagen, DK. Principal Investigators: Site 002: Dr, Johann de Bono. Site 003: Dr. Robert John Jones. Site 004: Dr. Lisa Sengeløv. Site 101: Dr. Richard Penson. Site 102: Dr Don Dizon. Site 105: Dr. James Hoffman. Site 106: Dr. John Micha. Site 108: Dr. Neil Finkler. Site 109 Dr. Patricia Braly. Site 111: Dr. Paul Celano. STUDY CENTERS: Part A: The Phase 1 part (advanced tumor) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer Research, UK • Site 101: Massachusetts General Hospital Cancer center, Boston, US Part B: The Phase 2 part, MTD expansion phase (ovarian cancer) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer -

Pricing of Cancer Medicines and Its Impacts
ACCESS TO MEDICINES, VACCINES AND PHARMACEUTICALS TECHNICAL REPORT Pricing of cancer medicines and its impacts A comprehensive technical report for the World Health Assembly Resolution 70.12 Operative paragraph 2.9 on pricing approaches and their impacts on availability and affordability of medicines for the prevention and treatment of cancer TECHNICAL REPORT Pricing of cancer medicines and its impacts Pricing of cancer medicines and its impacts ISBN 978-92-4-151511-5 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. -

140703EN NDA Belinostat
FDA approval of Beleodaq™ (belinostat) Accelerated Approval of Topotarget’s Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma Early Action follows Priority Review 5 weeks before PDUFA Date Trigger milestone payment of USD 25 million to Topotarget Beleodaq™ is expected to be available to patients in July 2014 and will be launched through Spectrum Pharmaceutical's existing oncology sales force The Orphan Oncology Innovator BioAlliance Pharma and Topotarget are merging to create Onxeo, following approval of both companies shareholders end of June 2014 Paris, July 3, 2014 – BioAlliance Pharma SA (Euronext Paris - BIO), an innovative Company specialized in the development of drugs in orphan oncology diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted Topotarget Accelerated Approval of Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (R/R PTCL). This follows a Priority Review of the Beleodaq™ New Drug Application (NDA) and was an Early Approval action prior to the August 9, 2014 PDUFA (Prescription Drug User Fee Act) date. Beleodaq™ was granted marketing authorization under the FDA’s accelerated approval program, which allows conditional approval of a medicine for a life-threatening disease based on early evidence suggesting clinical benefit. The approval is based on results from the BELIEF study, which enrolled 129 PTCL patients refractory to or who had failed at least one prior systemic therapy. A milestone cash payment of USD 25 million from Spectrum Pharmaceuticals is triggered by the NDA approval. A double-digit royalties as well as sales milestones of the aggregated net sales will be received by the company. -

151109EN ASH Abstract
Onxeo Reports Initial Results of Phase 1 Trial Evaluating Belinostat in Combination with CHOP in Peripheral T-cell Lymphoma (PTCL) Full results to be reported in Oral Presentation at 2015 ASH (American Society of Hematology) Annual Meeting Data demonstrate 89% objective response rate, 72% complete response rate, and good safety profile of belinostat in combination with CHOP Study supports the interest of belinostat in combination with CHOP as first-line treatment for PTCL Paris (France), Copenhagen (Denmark), November 9, 2015 – Onxeo S.A. (Euronext Paris, NASDAQ Copenhagen: ONXEO), an innovative company specializing in the development of orphan oncology drugs, announced the initial results from its Phase 1 trial of belinostat, its potent, pan-HDAC (histone deacetylase) inhibitor, in combination with CHOP chemotherapy regimen as first-line treatment in patients with peripheral T-cell lymphoma (PTCL). The Bel-CHOP combination has demonstrated to be well-tolerated with all components of belinostat and CHOP given at their approved therapeutic doses. Furthermore, the efficacy data indicate that the combination is a promising new regimen in PTCL that Onxeo together with its partner Spectrum Pharmaceuticals will further evaluate in a Phase 3 randomized trial, planned to begin in 2016. The abstract has been accepted for oral presentation at the 57th American Society of Hematology (ASH) Annual Meeting & Exposition, being held December 5-8 in Orlando, FL, USA. The open-label, randomized, two-part trial enrolled a total of 23 patients, of which 11 were enrolled in the dose-escalation Part A to determine the study’s primary endpoint, the maximum tolerated dose (MTD), followed by 12 patients treated in Part B at this dose level. -

Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe Harbor Statement
Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe harbor statement This announcement may contain forward-looking statements, including statements about Topotarget A/S’ expectations to the progression of Topotarget A/S’ clinical pipeline and with respect to cash burn guidance. Such statements are subject to risks and uncertainties of which many are outside the control of Topotarget A/S, and which could cause actual results to differ materially from those described. Topotarget A/S disclaims any intention or obligation to update or revise any forward-looking statements, whether as a result of new information, future events, or otherwise, unless required by Danish law. 2 Topotarget at a glance A Scandinavian-based biopharmaceutical company dedicated to develop and market cancer therapies • Situated in Copenhagen, Denmark with ~14 employees and a lean cost structure • Focused on the development and commercialization of belinostat, a molecular targeted cancer therapy NASDAQ OMX Listing Copenhagen 22% Symbol TOPO Denmark Switzerland 45% Market UK capitalization EUR 48 million Sweden (as of Aug 28, 2013) 20% ROW No. of shares 143,317,114 8% 4% 3 Building a strong commercial profile for belinostat Large sales potential in solid First registration filing tumors (CRC, bladder, expected Q4 2013 ovarian, NSCLC) Partnership with Spectrum Outstanding safety profile. Pharmaceuticals, Inc. Belinostat tested in more Pursuing partnerships in EU than 1,100 patients and Asia-Pac Belinostat – a pan-HDACi - Orphan indications (PTCL,