05/05/14 Agenda Attachment 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SAN FRANCISCO 2Nd Quarter 2014 Office Market Report
SAN FRANCISCO 2nd Quarter 2014 Office Market Report Historical Asking Rental Rates (Direct, FSG) SF MARKET OVERVIEW $60.00 $57.00 $55.00 $53.50 $52.50 $53.00 $52.00 $50.50 $52.00 Prepared by Kathryn Driver, Market Researcher $49.00 $49.00 $50.00 $50.00 $47.50 $48.50 $48.50 $47.00 $46.00 $44.50 $43.00 Approaching the second half of 2014, the job market in San Francisco is $40.00 continuing to grow. With over 465,000 city residents employed, the San $30.00 Francisco unemployment rate dropped to 4.4%, the lowest the county has witnessed since 2008 and the third-lowest in California. The two counties with $20.00 lower unemployment rates are neighboring San Mateo and Marin counties, $10.00 a mark of the success of the region. The technology sector has been and continues to be a large contributor to this success, accounting for 30% of job $0.00 growth since 2010 and accounting for over 1.5 million sf of leased office space Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 2012 2012 2012 2013 2013 2013 2013 2014 2014 this quarter. Class A Class B Pre-leasing large blocks of space remains a prime option for large tech Historical Vacancy Rates companies looking to grow within the city. Three of the top 5 deals involved 16.0% pre-leasing, including Salesforce who took over half of the Transbay Tower 14.0% (delivering Q1 2017) with a 713,727 sf lease. Other pre-leases included two 12.0% full buildings: LinkedIn signed a deal for all 450,000 sf at 222 2nd Street as well 10.0% as Splunk, who grabbed all 182,000 sf at 270 Brannan Street. -

Locating Critical Care Nurses in Mouth Care: an Institutional Ethnography
Locating Critical Care Nurses in Mouth Care: An Institutional Ethnography by Craig M. Dale A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Lawrence S. Bloomberg Faculty of Nursing University of Toronto © Copyright by Craig M. Dale 2013 Locating Critical Care Nurses in Mouth Care: An Institutional Ethnography Craig M. Dale Doctor of Philosophy Lawrence S. Bloomberg Faculty of Nursing University of Toronto 2013 Abstract Intubated and mechanically ventilated patients are vulnerable to respiratory tract infections. In response, the Ontario government has recently mandated surveillance and reporting of ventilator-associated pneumonia (VAP). Serious respiratory infections – and the related costs of additional care – can be reduced, in part, through oral hygiene. However, the literature asserts that oral care is neglected in busy, high-tech settings. Despite these concerns, little research has examined how mouth care happens in the critical care unit. The purpose of this institutional ethnography (IE) was to explore the social organization of mouth care in one critical care unit in Ontario, Canada. As a reflexive and critical method of inquiry, IE focuses on features of everyday life that often go unnoticed. In paying special attention to texts, the ethnographer traces how institutional forces that arrive from outside the practice setting coordinate experiences and activities. Inquiry began in the field with day/night participant observation to better understand the particularities of nursing care for orally intubated patients. Other data sources included reflexive fieldnotes, stakeholder interviews, and transcripts as well as work documents and artifacts. Over time, the analysis shifted from the critical care unit to the larger social context of Ontario’s Critical Care Transformation Strategy (OCCTS). -

Appendix 3-‐1 Historic Resources Evaluation
Appendix 3-1 Historic Resources Evaluation HISTORIC RESOURCE EVALUATION SEAWALL LOT 337 & Pier 48 Mixed-Use Development Project San Francisco, California April 11, 2016 Prepared by San Francisco, California Historic Resource Evaluation Seawall Lot 337 & Pier 48 Mixed-Use Project, San Francisco, CA TABLE OF CONTENTS I. Introduction .............................................................................................................................. 1 II. Methods ................................................................................................................................... 1 III. Regulatory Framework ....................................................................................................... 3 IV. Property Description ................................................................................................... ….....6 V. Historical Context ....................................................................................................... ….....24 VI. Determination of Eligibility.................................................................................... ……....44 VII. Evaluation of the Project for Compliance with the Standards ............................. 45 VIII. Conclusion ........................................................................................................................ 58 IX. Bibliography ........................................................................................................................ 59 April 11, 2016 Historic Resource Evaluation Seawall -

Mbtma 2017 Annual Report
Mission Bay Annual Report 2017 Executive Summary Mission Bay is will be largely completed by the end of 2019. As of December 2017, all residential units originally entitled are completed and occupied. Over a third of those units are affordable housing which prioritizes seniors living on fixed incomes, formerly homeless, and low-income families with children. Mission Bay’s residential population now tops 14,000. The Mission Bay project area is also entitled for 4.6 million square feet of commercial office and retail space. Approximately 2 million square feet is completed and occupied and the remainder is under construction. One 600,000 SF commercial property, The Exchange, will open in mid-2018. The 18,000 seat Chase Event Center started construction in 2017 and is on a fast track to open by Fall, 2019. A 200+ room hotel, and the remaining commercial properties (UCSF on Illinois Street, Uber headquarters on Third Street, and the Chase Center office towers) all have similar 18-to-24-month construction schedules. Over 15,000 people now work in Mission Bay. Approximately one third work in commercial buildings which are associated with the Mission Bay TMA and are located along Mission Bay Boulevard, Terry Francois Boulevard, Illinois Street and Owens Street. Two-thirds of workers at Mission Bay are employed by UCSF. Mission Bay’s diverse employment base includes everything from high tech office to medical research and corporate headquarters to non-profit organizations and government offices. The neighborhood’s growing ‘ground floor retail’, restaurants, and the new hotel will also bring hundreds of low income service workers to the community. -
NIH Conflict of Interest Regs Revised
OCTOBEROCTOBER 2005 www.asbmb.org Constituent Society of FASEB AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY NIH Conflict of Interest Regs Revised SEE PAGE 30 FOR NEW CLARA BENSON TRAVEL FELLOWSHIP AWARD Held in conjunction with EB2006 Custom Antibodies Your Way! Choose the protocol that is right for you! QwikScreen ™: 65 day, 2 rabbit protocol - 4 immunizations, 3 bleeds/rabbit (~100ml serum), customer supplied peptide/protein - Options: Peptide synthesis, immunograde Conjugation to carrier u ELISA u u Animal extensionsMS analysis $685 Standard: 80 day, 2 rabbit protocol - 5 immunizations, 5 bleeds/rabbit (~ 200ml ser Options: um), ELISA, customer supplied peptide/pr Peptide synthesis MS Check™ peptide sequence confirmation u HPLC purified peptide Affinity purification otein - Pinnacle: $975 u HPLC and MS analysis u Complete Affinity Purified Protocol- Animal extensions 2 rabbit pr 5 bleeds/rabbitotocol, (~ 200mlepitope serum), design, peptide PhD technical synthesis support, (up to 20mer),5 immunizations, HPLC purified to ~85%, 5+mg peptide to customer, ELISA, evaluation period, affinity purification, and morMS Check™ peptide sequence confirmationNo Hidden Charges! e… - Discounts for Multiple Protocols$1795 , Includes peptide sequencing by CID MS/MS– u Guaranteed Peptide Let our enthusiasm for scienceExpert workTechnical for SupportFidelity! P: 508.303.8222 www.21stcenturybio.com Toll-free: 877.217.8238 F: 508.303.8333 you! E: [email protected] www.asbmb.org AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY OCTOBER -

Sugar Coated Sugar Has Become Notorious, with Countless Claims of Its Ill Effects on Health
HHMI BULLETIN N OV . ’11 VOL.24 • NO.04 • 4000 Jones Bridge Road Chevy Chase, Maryland 20815-6789 Hughes Medical Institute Howard www.hhmi.org Address Service Requested Sugar Coated Sugar has become notorious, with countless claims of its ill effects on health. But not all sugars are bad for you. Consider fucose, an essential sugar the body needs. Without it, neurons can’t communicate, kidneys can’t filter blood, and skin can’t stay hydrated. Chemical biologist Carolyn • Bertozzi and her group are trying to learn more about the role of fucose in www.hhmi.org development. To do this, they injected modified versions of fucose into live, single-celled zebrafish embryos. As the embryos developed, the altered fucose molecules were incorporated into the sugars that coat cell surfaces. Using a simple chemical reaction, the team attached a labeled probe molecule to the altered fucose so they could visualize its location in the developing embryo. In this image of a 19-hour-old zebrafish embryo, labeled fucose (red) glows in the peripheral cells. Just one of many ways chemistry is helping answer biological questions (see “Living Chemistry,” page 12). YEAR OF CHEMISTRY Chemists fascinated by the complexity of biology are solving problems in neuroscience, immunology, and cell signaling. v ol. 24 / no. no. / Karen Dehnert and Scott Laughlin / Bertozzi lab In This Issue: Traveling Microscope / Lemur vs Mouse / Spotlight on Science Teacher Training 04 ObservatiOns ThE GIvInG TREE The history of science overflows with captivating stories of break- Johann Kraut in 1869 and Hermann Kolbe in 1874, but then, unfortunately, throughs that led to innovative disease treatments. -

RFP Appendix F.Pdf
REQUEST FOR PROPOSALS SEAWALL LOT 337 DEVELOPMENT OPPORTUNITY Appendix F Transportation Demand Management Program Submittal Requirements Introduction The Seawall Lot 337 Mixed Use Project offers great opportunity to develop thoughtful, effective, and integrated strategies for managing transportation demand, which should serve as a model for Mission Bay and other major mixed use development areas. There has been and continues to be major planned public investment to expand public transit service, and bicycle and pedestrian access to AT&T Park, Mission Bay and along the waterfront, with numerous nearby connections to the regional transit network. As expressed in the RFP Objectives, Respondents are required to include a Transportation Demand Management Plan (TDMP), that presents a comprehensive and integrated approach to planning and managing transportation demands associated with this Mixed Use Project, and addresses transportation and parking needs associated with AT&T Ballpark. This document provides direction on the issues and elements that must be addressed in the TDMP submittal. A TDMP alone cannot result in transit-oriented development. The land use plan must incorporate smart land use measures such as clustering residential development around neighborhood-serving retail and transit stops. The design and placement of these uses should make alternative transportation a convenient and efficient way to travel to and within the SWL 337 and Pier 48 area, with attractive and comfortable amenities. Fortunately, SWL 337 is a large development site which affords many ways to configure land uses, and design buildings, public spaces and streets to prioritize access and use of public transit, walking and non-motorized circulation as a means of everyday transportation. -

Stockholm 2010 Programs and Abstracts
Welcome to Stockholm and Advances in Neuroblastoma Research! Dear all, We are so happy that you all finally made it here, to ANR 2010, to Scandinavia, and most of all, to our beautiful capital of Sweden, Stockholm! We are excited to have received more than 400 abstracts which is the basis of our scientific programme. We are therefore confident that this year’s programme will satisfy every single participant, being a researcher, a clinician, a nurse, a student or a parent. Numerous sessions are prepared, spanning all aspects of neuroblastoma from bench to bedside. We are thrilled to have such excellent invited lecturers including four Nobel laureates visiting us, together with several future ones, we are sure! We are grateful to our sponsors and all others who have contributed to make the meeting possible. Please enjoy the multitude of oral and poster presentations. Discuss and interact! Enjoy the social programme, explore the light summer in the beautiful city of Stockholm. After the meeting you should go home exhausted with important experiences, new ideas and friends. On behalf of the local organising committee, Per Kogner CONTENTS General Information 2Abstract Book Contents Abstract Book 77 Programme Author Index 218 Monday June 21st 7 Keyword Index 233 Tuesday June 22nd 14 Poster session 29 Wednesday June 23rd 53 Poster session 29 Thursday June 24th 70 Committees* ANRA, Advances in Neuroblastoma Research Association ANRA President: Susan L. Cohn ANRA Past President: Frank Berthold ANRA Incoming President: Michelle Haber ANRA Steering Committee ANRA Advisory Board (North/South America) Frank Berthold Rochelle Bagatell Garrett M. Brodeur Sylvain Baruchel General Information General Susan L. -

STRATEGIC ANALYSIS REPORT the Role of Shuttle Services in San F Rancisco’S Transportation System
FINALAR S 08/09–2 • JUNE 28, 2011 • PAGE 1 SAN FRANCISCO COUNTY TRANSPORTATION AUTHORITY 100 Van Ness Avenue, 26th Floor, San Francisco, CA 94102 TEL 415.522.4800 FAX 415.522.4829 EMAIL [email protected] WEB www.sfcta.org FINAL SAR 08/09–2 STRATEGIC ANALYSIS REPORT The Role of Shuttle Services in San F rancisco’s Transportation System Initiated by Commissioner Dufty APPROVED BY THE AUTHORITY BOARD JUNE 28, 2011 TABLE OF CONTENTS ABOUT SARS: PURPOSE OF DOCUMENT Strategic Analysis Reports (SARs) are carried out at the re- ABOUT SARS: PURPOSE OF DOCUMENT 1 quest of the Authority Board, to frame current issues of concern and to inform policy development regarding spe- INTRODUCTION 2 cific transportation issues which may not be adequately ad- dressed by existing regulations or policy. This SAR, initiated I. BACKGROUND 2 at the request of Commissioner Dufty, analyzes the topic of shuttle services in San Francisco, and seeks to determine II. EXISTING CONDITIONS 4 how best to integrate the growth of shuttles into the overall transportation system, and to manage their operations, in a III. POLICY ANALYSIS 10 way that continues to realize their benefits while address- ing their impacts. Data for this SAR was gathered through IV. RECOMMENDATIONS AND NEXT STEPS 14 literature review, field observations, and extensive outreach to various stakeholders involved in the shuttle landscape BIBLIOGRAPHY, CITY DEPARTMENT STAFF including providers, operators, users, public agencies, and CONSULTED, STAKEHOLDERS CONSULTED 15 the general public. The study finds that, while shuttles play a valuable role in the overall San Francisco transportation ACKNOWLEDGEMENTS 16 system, policy guidance and improved management are needed and warranted in order to improve operations and APPENDICES 17 minimize impacts. -
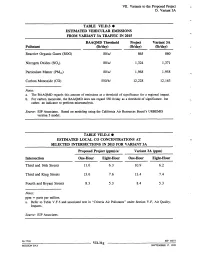
VII. Variants to the Proposed Project D
VII. Variants to the Proposed Project D. Variant 3A TABLE VII.D.3 ¯ ESTIMATED VEHICULAR EMISSIONS FROM VARIANT 3A TRAFFIC IN 2015 BAAQMD Threshold Project Variant 3A Pollutant Ob/day) (lb/day) (lb/day) Reactive Organic Gases (ROG) 80/a/ 865 860 Nitrogen Oxides (NOx) 80/a/ 1,324 1,371 Particulate Matter (PM~0) 80/a/ 1,968 1,958 Carbon Monoxide (CO) 550/b/ 12,228 12,163 Notes: a. The BAAQMD regards this amount of emissions as a threshold of significance for a regional impact. b. For carbon monoxide, the BAAQMD does not regard 550 lb/day as a threshold of significance, but rather, an indicator to perform microanalysis. Source: EIP Associates. Based on modeling using the California Air Resources Board’s URBEMIS version 5 model. TABLE VII.D.4 ¯ ESTIMATED LOCAL CO CONCENTRATIONS AT SELECTED INTERSECTIONS IN 2015 FOR VARIANT 3A Proposed Project (ppm)/a/ Variant 3A (ppm) Intersection One-Hour Eight-Hour One-Hour Eight-Hour Third and 16th Streets 11.0 6.3 10.9 6.2 Third and King Streets 13.6 7.6 13.4 7.4 Fourth and Bryant Streets 8.3 5.3 8.4 5.3 Notes: ppm = parts per million. a. Refer to Table V.F.5 and associated text in "Criteria Air Pollutants" under Section V.F, Air Quality: Impacts. Source: EIP Associates. 96.771E VII.31g El!’ 10073 MISSION BAY SEPTEMBER 17, 1998 VII. Variants to the Proposed Project D. Variant 3A In this variant, the decrease in overall traffic would slightly reduce toxic air contaminant emissions from mobile sources. -

V. Environmental Setting and Impacts E. Transportation Impacts Passenger Trips
V. Environmental Setting and Impacts E. Transportation Impacts passenger trips. Following the BART strike in September, 1997, AC Transit transbay ridership increased substantially, and has stabilized in recent months at a higher level than before the strike. The expected growth in passenger trips, however, has not been reassessed, and the 9,000 to 12,000 additional trips represent a smaller proportion of the revised current ridership. Therefore, expected growth between 1997 and 2010 yields a growth rate of 80% to 110%./82/ AC Transit’s growth estimate assumes that the additional capacity BART will gain with smaller headways will consist primarily of trains traveling on the Dublin/Pleasanton Line. This would mean that a large portion of transbay travel demand growth to the northern part of AC Transit’s service area could not be directly accommodated by BART. However, BART’s Short Range Transit Plan suggests that it will be able to accommodate more transbay demand growth than AC Transit predicts. Therefore, a total cumulative growth rate of 80% was assumed over the next 13 years for AC Transit rather than the larger rate. This corresponds to an annual growth of approximately 4.6%. Currently, there are no plans to increase the number of buses or transbay bus runs in the future. Continued growth in demand may prompt a reevaluation of the service provided. An 80% increase in cumulative passenger trips during the p.m. peak hour would increase the current 83% average load factor to 150%. If all eastbound transbay buses were equally loaded, a load factor of 150% would translate to approximately 23 s’tandees per bus. -

Johnson.Speakers to 2017.17
Johnson Symposia 1986-2018 1986 ALEXANDER KLIBANOV KONRAD BLOCH STEPHEN FODOR ALBERT ESCHENMOSER GEORGE OLAH SIR DEREK BARTON CHI-HUEY WONG JOHN D. ROBERTS REINHARD HOFFMANN GILBERT STORK BRUCE AMES WILLIAM S. JOHNSON 1995 1987 DEREK BARTON DUILIO ARIGONI RON BRESLOW STEPHEN BENKOVIC ALBERT ESCHENMOSER RONALD BRESLOW ROBERT GRUBBS E. J. COREY RALPH HIRSCHMANN GILBERT STORK GEORGE OLAH PETER DERVAN RYOJI NOYORI E. THOMAS KAISER BARRY SHARPLESS JEAN-MARIE LEHN GILBERT STORK 1988 JOHN ROBERTS SAMUEL DANISHEFSKY 1996 DUDLEY WILLIAMS MARYE ANNE FOX PAUL BARTLETT JOEL HUFF KOJI NAKANISHI ERIC JACOBSEN DUILIO ARIGONI LARRY OVERMAN JEREMY KNOWLES GEORGE PETTIT K. BARRY SHARPLESS PETER SCHULTZ DONALD CRAM GREGORY VERDINE 1989 MAXINE SINGER JACK BALDWIN 1997 A. R. BATTERSBY STEPHEN BUCHWALD DAVID EVANS CHARLES CASEY ROBERT GRUBBS STEPHEN FESIK CLAYTON HEATHCOCK M. REZA GHADIRI KOJI NAKANISHI STEPHEN HANESSIAN R. NOYORI DANIEL KAHNE CHARLES SIH MARY LOWE GOOD 1990 JOANNE STUBBE ROBERT BERGMAN 1998 THOMAS CECH KEN HOUK ROALD HOFFMANN NED PORTER STUART SCHREIBER ANDREAS PFALTZ HERBERT BROWN MAURICE BROOKHART HENRY ERLICH SEAN LANCE K. C. NICOLAOU WILLIAM FENICAL E. VOGEL SIDNEY ALTMAN 1991 DUILIO ARIGONI HARRY ALLCOCK 1999 JEROME BERSON STEVEN BOXER DALE BOGER JOHN BRAUMAN WILLIAM JORGENSEN JAMES COLLMAN RALPH RAPHAEL CARL DJERASSI PETER SCHULTZ CHAITAN KHOSLA DIETER SEEBACH BARRY TROST CHRISTOPER WALSH ROBERT WAYMOUTH 1992 THOMAS WANDLESS JACQUELINE BARTON PAUL WENDER KLAUS BIEMANN 2000 RICHARD LERNER SCOTT DENMARK MANFRED REETZ JANINE COSSY ALEJANDRO ZAFFARONI DENNIS DOUGHERTY CLARK STILL JONATHAN ELLMAN J. FRASER STODDART JERROLD MEINWALD HISASHI YAMAMOTO EI-ICHI NEGISHI 1993 MASAKATSU SHIBASAKI PAUL EHRLICH BERND GIESE LOUIS HEGEDUS 2001 STEVEN LEY ROB ARMSTRONG JULIUS REBEK JON CLARDY F.