3 Timetable for Development of the Proposed Phd Program, Including Enrollment Projections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SAN FRANCISCO 2Nd Quarter 2014 Office Market Report
SAN FRANCISCO 2nd Quarter 2014 Office Market Report Historical Asking Rental Rates (Direct, FSG) SF MARKET OVERVIEW $60.00 $57.00 $55.00 $53.50 $52.50 $53.00 $52.00 $50.50 $52.00 Prepared by Kathryn Driver, Market Researcher $49.00 $49.00 $50.00 $50.00 $47.50 $48.50 $48.50 $47.00 $46.00 $44.50 $43.00 Approaching the second half of 2014, the job market in San Francisco is $40.00 continuing to grow. With over 465,000 city residents employed, the San $30.00 Francisco unemployment rate dropped to 4.4%, the lowest the county has witnessed since 2008 and the third-lowest in California. The two counties with $20.00 lower unemployment rates are neighboring San Mateo and Marin counties, $10.00 a mark of the success of the region. The technology sector has been and continues to be a large contributor to this success, accounting for 30% of job $0.00 growth since 2010 and accounting for over 1.5 million sf of leased office space Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 2012 2012 2012 2013 2013 2013 2013 2014 2014 this quarter. Class A Class B Pre-leasing large blocks of space remains a prime option for large tech Historical Vacancy Rates companies looking to grow within the city. Three of the top 5 deals involved 16.0% pre-leasing, including Salesforce who took over half of the Transbay Tower 14.0% (delivering Q1 2017) with a 713,727 sf lease. Other pre-leases included two 12.0% full buildings: LinkedIn signed a deal for all 450,000 sf at 222 2nd Street as well 10.0% as Splunk, who grabbed all 182,000 sf at 270 Brannan Street. -

Appendix 3-‐1 Historic Resources Evaluation
Appendix 3-1 Historic Resources Evaluation HISTORIC RESOURCE EVALUATION SEAWALL LOT 337 & Pier 48 Mixed-Use Development Project San Francisco, California April 11, 2016 Prepared by San Francisco, California Historic Resource Evaluation Seawall Lot 337 & Pier 48 Mixed-Use Project, San Francisco, CA TABLE OF CONTENTS I. Introduction .............................................................................................................................. 1 II. Methods ................................................................................................................................... 1 III. Regulatory Framework ....................................................................................................... 3 IV. Property Description ................................................................................................... ….....6 V. Historical Context ....................................................................................................... ….....24 VI. Determination of Eligibility.................................................................................... ……....44 VII. Evaluation of the Project for Compliance with the Standards ............................. 45 VIII. Conclusion ........................................................................................................................ 58 IX. Bibliography ........................................................................................................................ 59 April 11, 2016 Historic Resource Evaluation Seawall -

Mbtma 2017 Annual Report
Mission Bay Annual Report 2017 Executive Summary Mission Bay is will be largely completed by the end of 2019. As of December 2017, all residential units originally entitled are completed and occupied. Over a third of those units are affordable housing which prioritizes seniors living on fixed incomes, formerly homeless, and low-income families with children. Mission Bay’s residential population now tops 14,000. The Mission Bay project area is also entitled for 4.6 million square feet of commercial office and retail space. Approximately 2 million square feet is completed and occupied and the remainder is under construction. One 600,000 SF commercial property, The Exchange, will open in mid-2018. The 18,000 seat Chase Event Center started construction in 2017 and is on a fast track to open by Fall, 2019. A 200+ room hotel, and the remaining commercial properties (UCSF on Illinois Street, Uber headquarters on Third Street, and the Chase Center office towers) all have similar 18-to-24-month construction schedules. Over 15,000 people now work in Mission Bay. Approximately one third work in commercial buildings which are associated with the Mission Bay TMA and are located along Mission Bay Boulevard, Terry Francois Boulevard, Illinois Street and Owens Street. Two-thirds of workers at Mission Bay are employed by UCSF. Mission Bay’s diverse employment base includes everything from high tech office to medical research and corporate headquarters to non-profit organizations and government offices. The neighborhood’s growing ‘ground floor retail’, restaurants, and the new hotel will also bring hundreds of low income service workers to the community. -

RFP Appendix F.Pdf
REQUEST FOR PROPOSALS SEAWALL LOT 337 DEVELOPMENT OPPORTUNITY Appendix F Transportation Demand Management Program Submittal Requirements Introduction The Seawall Lot 337 Mixed Use Project offers great opportunity to develop thoughtful, effective, and integrated strategies for managing transportation demand, which should serve as a model for Mission Bay and other major mixed use development areas. There has been and continues to be major planned public investment to expand public transit service, and bicycle and pedestrian access to AT&T Park, Mission Bay and along the waterfront, with numerous nearby connections to the regional transit network. As expressed in the RFP Objectives, Respondents are required to include a Transportation Demand Management Plan (TDMP), that presents a comprehensive and integrated approach to planning and managing transportation demands associated with this Mixed Use Project, and addresses transportation and parking needs associated with AT&T Ballpark. This document provides direction on the issues and elements that must be addressed in the TDMP submittal. A TDMP alone cannot result in transit-oriented development. The land use plan must incorporate smart land use measures such as clustering residential development around neighborhood-serving retail and transit stops. The design and placement of these uses should make alternative transportation a convenient and efficient way to travel to and within the SWL 337 and Pier 48 area, with attractive and comfortable amenities. Fortunately, SWL 337 is a large development site which affords many ways to configure land uses, and design buildings, public spaces and streets to prioritize access and use of public transit, walking and non-motorized circulation as a means of everyday transportation. -

STRATEGIC ANALYSIS REPORT the Role of Shuttle Services in San F Rancisco’S Transportation System
FINALAR S 08/09–2 • JUNE 28, 2011 • PAGE 1 SAN FRANCISCO COUNTY TRANSPORTATION AUTHORITY 100 Van Ness Avenue, 26th Floor, San Francisco, CA 94102 TEL 415.522.4800 FAX 415.522.4829 EMAIL [email protected] WEB www.sfcta.org FINAL SAR 08/09–2 STRATEGIC ANALYSIS REPORT The Role of Shuttle Services in San F rancisco’s Transportation System Initiated by Commissioner Dufty APPROVED BY THE AUTHORITY BOARD JUNE 28, 2011 TABLE OF CONTENTS ABOUT SARS: PURPOSE OF DOCUMENT Strategic Analysis Reports (SARs) are carried out at the re- ABOUT SARS: PURPOSE OF DOCUMENT 1 quest of the Authority Board, to frame current issues of concern and to inform policy development regarding spe- INTRODUCTION 2 cific transportation issues which may not be adequately ad- dressed by existing regulations or policy. This SAR, initiated I. BACKGROUND 2 at the request of Commissioner Dufty, analyzes the topic of shuttle services in San Francisco, and seeks to determine II. EXISTING CONDITIONS 4 how best to integrate the growth of shuttles into the overall transportation system, and to manage their operations, in a III. POLICY ANALYSIS 10 way that continues to realize their benefits while address- ing their impacts. Data for this SAR was gathered through IV. RECOMMENDATIONS AND NEXT STEPS 14 literature review, field observations, and extensive outreach to various stakeholders involved in the shuttle landscape BIBLIOGRAPHY, CITY DEPARTMENT STAFF including providers, operators, users, public agencies, and CONSULTED, STAKEHOLDERS CONSULTED 15 the general public. The study finds that, while shuttles play a valuable role in the overall San Francisco transportation ACKNOWLEDGEMENTS 16 system, policy guidance and improved management are needed and warranted in order to improve operations and APPENDICES 17 minimize impacts. -
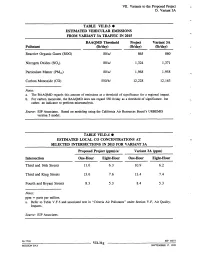
VII. Variants to the Proposed Project D
VII. Variants to the Proposed Project D. Variant 3A TABLE VII.D.3 ¯ ESTIMATED VEHICULAR EMISSIONS FROM VARIANT 3A TRAFFIC IN 2015 BAAQMD Threshold Project Variant 3A Pollutant Ob/day) (lb/day) (lb/day) Reactive Organic Gases (ROG) 80/a/ 865 860 Nitrogen Oxides (NOx) 80/a/ 1,324 1,371 Particulate Matter (PM~0) 80/a/ 1,968 1,958 Carbon Monoxide (CO) 550/b/ 12,228 12,163 Notes: a. The BAAQMD regards this amount of emissions as a threshold of significance for a regional impact. b. For carbon monoxide, the BAAQMD does not regard 550 lb/day as a threshold of significance, but rather, an indicator to perform microanalysis. Source: EIP Associates. Based on modeling using the California Air Resources Board’s URBEMIS version 5 model. TABLE VII.D.4 ¯ ESTIMATED LOCAL CO CONCENTRATIONS AT SELECTED INTERSECTIONS IN 2015 FOR VARIANT 3A Proposed Project (ppm)/a/ Variant 3A (ppm) Intersection One-Hour Eight-Hour One-Hour Eight-Hour Third and 16th Streets 11.0 6.3 10.9 6.2 Third and King Streets 13.6 7.6 13.4 7.4 Fourth and Bryant Streets 8.3 5.3 8.4 5.3 Notes: ppm = parts per million. a. Refer to Table V.F.5 and associated text in "Criteria Air Pollutants" under Section V.F, Air Quality: Impacts. Source: EIP Associates. 96.771E VII.31g El!’ 10073 MISSION BAY SEPTEMBER 17, 1998 VII. Variants to the Proposed Project D. Variant 3A In this variant, the decrease in overall traffic would slightly reduce toxic air contaminant emissions from mobile sources. -

V. Environmental Setting and Impacts E. Transportation Impacts Passenger Trips
V. Environmental Setting and Impacts E. Transportation Impacts passenger trips. Following the BART strike in September, 1997, AC Transit transbay ridership increased substantially, and has stabilized in recent months at a higher level than before the strike. The expected growth in passenger trips, however, has not been reassessed, and the 9,000 to 12,000 additional trips represent a smaller proportion of the revised current ridership. Therefore, expected growth between 1997 and 2010 yields a growth rate of 80% to 110%./82/ AC Transit’s growth estimate assumes that the additional capacity BART will gain with smaller headways will consist primarily of trains traveling on the Dublin/Pleasanton Line. This would mean that a large portion of transbay travel demand growth to the northern part of AC Transit’s service area could not be directly accommodated by BART. However, BART’s Short Range Transit Plan suggests that it will be able to accommodate more transbay demand growth than AC Transit predicts. Therefore, a total cumulative growth rate of 80% was assumed over the next 13 years for AC Transit rather than the larger rate. This corresponds to an annual growth of approximately 4.6%. Currently, there are no plans to increase the number of buses or transbay bus runs in the future. Continued growth in demand may prompt a reevaluation of the service provided. An 80% increase in cumulative passenger trips during the p.m. peak hour would increase the current 83% average load factor to 150%. If all eastbound transbay buses were equally loaded, a load factor of 150% would translate to approximately 23 s’tandees per bus. -

Board of Appeals, City & County of San Francisco
BOARD OF APPEALS, CITY & COUNTY OF SAN FRANCISCO Appeal No. 1S..187 Appellant(s) vs. Respondent NOTICE OF APPEAL NOTICE IS HEREBY GIVEN THAT on November 19, 2015, the above named appellant(s) filed an appeal with the Board of Appeals of the City and County of San Francisco from the decision or order of the above named department(s), commission, or officer. The substance or effect of the decision or order appealed from is the ISSUANCE on November 10, 2015 to GSW Arena, LLC , of a Place of Entertainment Permit (for a mixed use event center open seven days a week from 7:00 AM to 2:00 AM, with proposed entertainment to include family shows, professional basketball games, collegiate athletic events, and concerts, and with food and beverages served on-site, including alcoholic beverages) at Mission Bay South Blocks 29 & 31. PERMIT NO. EC-1352 FOR HEARING ON December 09, 2015 Address of Appellant(s): Address of Other Parties: Mission Bay Alliance , Appellant GSW Arena, LLC, Permit Holder c/o Thomas Lippe, Attorney for Appellant c/o Mary Murphy, Attorney for Permit Holder Law Offices of Thomas Lippe Gibson Dunn 201 Mission Street, 12th Floor 555 Mission Street, Suite 3000 San Francisco, CA 94105 San Francisco, CA 94105 BOARD ()F A.PPEALS Date Filed: OV 1 9 'ut:J CITY & COUNTY OF SAN FRANCISCO APPEAL# / ~~t n BOARD OF APPEALS PRELIMINARY STATEMENT OF APPEAL I I We, Mission Bay Alliance, hereby appeal the following departmental action: CONDITIONAL GRANT of a Place of Entertainment Permit by the Entertainment Commission which was issued or became effective on : November 10, 2015, to: GSW Arena, LLC , for the property located at: Mission Bay South Blocks 29 & 31. -
Open PDF Brochure
Presented by the Division of Clinical Epidemiology of the Department of Epidemiology and Biostatistics, University of California, San Francisco, School of Medicine University of California San Francisco EVIDENCE-BASED Advanced Workshop on DIAGNOSIS: Evaluating and Using Medical Tests for Clinicians, Educators, Editors, and Policy Makers 3 1 0 2 , 1 2 - 0 2 Y A D I R F e - Y A n D S R u U H T J China Basin Landing COURSE CHAIR 185 Berry Street Michael A. Kohn, MD, MPP Lobby 3, Room 6702 Associate Professor of Epidemiology & Biostatistics, San Francisco, CA University of California, San Francisco; Attending Emergency Physician, Mills-Peninsula Medical Center COURSE CO-CHAIRS Thomas B. Newman, MD, MPH Chief, Division of Clinical Epidemiology, Professor, Departments of Epidemiology & Biostatistics and Pediatrics; Attending Physician, Department of Pediatrics, University of California, San Francisco Christopher R. Carpenter, MD Associate Professor of Emergency Medicine, Director, Evidence-Based Medicine, Washington University School of Medicine, St. Louis; Evidence-Based Diagnostics Section Editor, Academic Emergency Medicine China Basin Landing EVIDENCE-BASED DIAGNOSIS: 185 Berry Street Advanced Workshop on Evaluating Lobby 3, Room 6702 San Francisco, CA and Using Medical Tests for Clinicians, Educators, Editors, and Policy Makers June 20-21, 2013 Medicine today relies increasingly on diagnostic, prognostic, and ACCREDITATION screening tests. We spend vast resources on testing, and new The University of tests are being developed and marketed -

Fred Blackwell, Executive Director
102-011.12-002 Meeting of July 5, 2011 INFORMATIONAL MEMORANDUM TO: Agency Commissioners FROM: Fred Blackwell, Executive Director SUBJECT: Media Clippings from 06.16.11 to 06.30.11 Enclosed is a collection of supportive and positive newspaper/media clippings that refer to the Redevelopment Agency or an Agency-related project or program. (Originated by Gia Casteel-Brown, Executive Assistant) Fred Blackwell Executive Director MISSION BAY / TRANSBAY / SOMA / BVHSP: Attachment 1: SAN FRANCISCO Business Times: "Last Mission Bay commercial site hits block," June 22, 2011 Attachment 2: SAN FRANCISCO Business Times: "Salesforce CEO: approve our HQ plan, or else...," June 23, 2011 Attachment 3: SAN FRANCISCO Business Times: "Salesforce campus to transform blight into bright," June 24, 2011 Attachment 4: SAN FRANCISCO Business Times: "Will Alexandria be a buyer again in Mission Bay," June 30, 2011 Attachment 5: Cbe examiner/sfexaminer.com: "Checkout time is near for San Francisco's Hugo Hotel," June 16, 2011 Attachment 6: SFGate.com: "S.F. police brass in way of 6 th Street substation," June 23, 2011 Attachment 7: SAN FRANCISCO Business Times: "Update: Transit center foundation work begins," June 24, 2011 Attachment 8: Email from Linda Green, SFRA Staff: Mighty Men of Valor at South Beach Harbor," June 16, 2011 102-011.12-002 Meeting of July 5, 2011 Media Clippings Page 2 Attachment 9: SFGate.com: "Bayview Third Street revitalization has way to go," June 20, 2011 Attachment 10: Zbe Qxaminer/sfexaminer.com: "San Francisco supervisors to hold -

Oc2()1.1 .. Calendar Item No
MINUWM This Calendar ~em. No. was approved as Minute It.em No.~ by t~ California State Lands __ ~ion by a vote of~ to:::Q-at its 'l meeting. CALENDAR ITEM 65 A 13 08/26/97 G11-01 s 3 D. Plummer B. Stevenson CONSIDER APPROVAL OF DETERMINATIONS PURSUANT TO PUBLIC RESOURCES CODE SECTION 6702 (b) REGARDING A GROUND LEASE AND LEASE DISPOSITION AND DEVELOPMENT AGREEMENT BETWEEN THE CITY AND COUNTY OF SAN FRANCISCO, THROUGH ITS PORT COMMISSION, AND THE CHINA BASIN BALLPARK COMPANY LLC BACKGROUND~ The San Francisco Port Commission (Port) has requested the California State Lands ".Commission to find that the lease for a new San Francisco Giants ballpark is consistent ..- with the public trust, and to make the determinations described in Public Resources Code Section 6702 (b). The lease property, shown in Exhibits A and B (attached to this calendar item and incorporated by reference), is comprised of filled tide and submerged lands and other lands which, following their purchase by the Port, will become subject to the Burton Act. The Burton Act is the legislation through which the Port administers tide and submerged lands granted to the City and County of San Francisco by the State (Chapter 1333, Statutes of 1968, as amended). The parties to the Lease Disposition and Development Agreement (the "Lease ODA") and the Ground Lease are the Port and the developer of the ballpark, the China Basin Ballpark Company LLC ("CBBC"). The CBBC supports the request made by the Port to the State Lands Commission. Further discussion of the Port's request is includ_ed below under the heading "Section 24 of the Burton Act." " - The Port has submitted all significant transactional documents to the Commission to support its request. -

Collection Highlights,” San Jose Museum of Art, CA, Nov.-Dec
NAME: Richard Shaw (415) 456-8767 Activity from academic years 02/03, 03/04, 04/05 have been bolded. EDUCATION: B.F.A., San Francisco Art Institute, 1965 M.F.A., University of California at Davis, 1968 POSITIONS HELD: 1987- Professor, University of California at Berkeley 1978 Lecturer, University of California at Davis 1977 Lecturer, College of Marin, Kentfield, California 1971 Lecturer, University of Wisconsin at Madison 1970 Lecturer, University of California at Berkeley 1966-87 Instructor, San Francisco Art Institute HONORS AND AWARDS: 2002 Marin Arts Council Board Award, San Rafael, CA, Dec. 5 1998 Fellow of the American Crafts Council, New York, NY 1996 Falkirk Annual Life Member Award, Falkirk Cultural Center, San Rafael, CA 1988 Honorary Doctor of Fine Arts Degree, San Francisco Art Institute 1987 Visiting Artist Grant, Atelier Experimental de Researche et de Creation, Manufacture Nationale de Sevres, Paris, France 1974 Visual Artist Fellowship for Crafts, National Endowment for the Arts 1973 Research Grant, Union of Independent Colleges of Art 1971 Visual Artist Fellowship, National Endowment for the Arts RESIDENCIES: (Selected) 2004 Starr Residency, University of Wisconsin, Madison, WI, March 2003 Anderson Ranch, Aspen, CO, Aug. 18-29 2002 Public Glass, San Francisco, CA 2001 Magnolia Editions, Oakland, CA 1998 Shigaraki Cultural Ceramic Park, Shigaraki, Japan 1997 Artist in Residence, Phillips Academy, Andover, MA 1996 Collaboration, Magnolia Editions, Oakland, CA 1995 University of Hawaii, Honolulu. “East Meets West” Ceramic Symposium Anderson Ranch, Aspen, CO 1977 Visiting Artist Grant, Clayworks, New York, NY 1978 SOLO EXIBITIONS AND TWO PERSON COLLABORATIONS: 2005Richard and Martha Shaw, Sataka Garo, Sacarmento, CASept 6-Oct.