Debunking UVGI Myths
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemical Disinfectants for Biohazardous Materials (3/21)
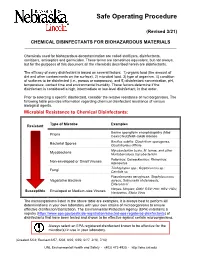
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic
Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic Vickie Leonard, PhD Environmental Health in Early Care and Educaon Project, Western States Pediatric Environmental Health Specialty Unit (WSPEHSU) 1 Why Should We Be Concerned about Environmental Health in ECE? 2 Why Should We Be Concerned about Environmental Health in ECE? • There are 8 million children in child care centers in the U.S. A child may spend up to 12,500 hours in an ECE facility. A million child care providers work in these centers in the U.S. Half are child-bearing age. • Many toxicants found in child care facilities are not addressed in state child care health and safety regulations. • No agency at the state or federal level is charged with ensuring children’s health and safety in and around schools and ECE facilities. • No systematic means exists for collecting data on environmental exposures in these buildings. • Teachers have more protection in these buildings (unions, OSHA) than children do 3 Why Should We Be Concerned about Environmental Health in ECE? • Many people think that adults and children are exposed to, and affected by, toxic chemicals in the same way. • This is not the case. • Children • have higher exposures to toxicants in the environment, • are more vulnerable to the effects of those toxicants than adults. 4 Cleaning and Disinfec?ng Products: A Major Source of Exposure in Child Care and Schools • Products used to clean, sanitize and disinfect child care facilities and schools are a good example of the pervasive and unregulated use of toxic chemicals that put the health of our children at risk. -

Silver As a Drinking-Water Disinfectant
Silver as a drinking-water disinfectant Silver as a drinking-water disinfectant Alternative drinking-water disinfectants: silver ISBN 978-92-4-151369-2 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Alternative drinking-water disinfectants: bromine, iodine and silver. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. -

Infection Prevention & Control Chlorhexidine
Winnipeg Regional Health Authority Acute Care Infection Prevention & Control Manual INFECTION PREVENTION & CONTROL CHLORHEXIDINE GLUCONATE CONCENTRATION FOR HAND HYGIENE COMMUNICATION FORM PART 1: ISSUE & RECOMMENDATIONS Issue: The WRHA Infection Prevention and Control program (IP&C) was requested to research and recommend acceptable concentrations of chlorhexidine gluconate (CHG) (2% versus 4%) for hand hygiene in all programs within WRHA sites, to ensure appropriate products are being used, and facilitate standardization. Recommendations: Use 2% CHG hand cleansers for hand hygiene when antimicrobial hand soap is indicated. Do NOT use 4% CHG for hand hygiene as the minimal improvement in efficacy (from 2%), does not warrant the increased frequency of skin irritation and breakdown, which ultimately impedes effective hand hygiene practices. PART 2: BACKGROUND: DISCUSSION OF ISSUE, OPTIONS AND ANALYSIS & REFERENCES Discussion of Issue: There are several different hand hygiene products used within and between WRHA sites. All areas should adhere to recommended hand hygiene products, as determined by available evidence. There are differences in when specific hand hygiene products are indicated. It is important to identify the appropriate product to use for the appropriate reason, as supported by evidence. Options and Analysis: 1. CHG has a cumulative effect when applied to the skin. In hand hygiene, this effect remains and is sustained, especially when hand hygiene is repeated. 2% CHG is appropriate for hand antisepsis because of the cumulative effect.1 2. Literature regarding differences between 2% and 4% CHG identifies there is minimal difference in efficacy between 2% and 4% CHG for hand antisepsis and cleansing.2 3. The frequency of skin irritation is concentration dependent, with products containing 4% most likely to cause dermatitis when used frequently for hand antisepsis. -

U.S. EPA, Pesticide Product Label, 776 DISINFECTANT VIRUCIDE
, 1-ls-lf9 UNITED ST ATES ENVIRONMENTAL PROTECTION AGENCY Carroll Company 2900 West Kingsley Road Garland, TX 75041 Subject: 776 Disinfectant, Virucide and Cleaner EPA Registration No. 4313-22 Amendment Dated November 9, 1998 Attn: Linda Kirk Kirby Director, Regulatory Compliance The amendment referred to above, submitted in connection with registration under the Federal Insecticide, Fungicide and Rodenticide Act, as amended, is acceptable. A stamped copy of the label is enclosed for your records. Submit one (I) copy ofthe finished printed label before this product is released for shipment. If you have any questions concerning the comments in this letter, you should contact Zenobia Jones at (703) 308-6198. Sincerely, ) JJ~lvJHdL Velma Noble Product Manager 31 Regulatory Management Branch I Antimicrobial Division (751 OW) COHCURRI!HCI!S ::::} ·m·I~ .Q........ ................ - ....................................... -................................ _............................. DATE ) . \-1i.-9l1... ....... ................... ................. .................................................................................... OFFICIAL FILE COpy Primed Oft R~cye/~d Paper ~' '....,-. " DISINFECTANT, UIRUCIDE* AND CLEANER FOR HOSPITAL INSTITUTIONAL ACTIVE INGREDIENT: AND iNDUSTRIAL USE Alkyl (C14 50%, C12 40%, C16 10%) dimelhyl • benzyl ammonium chloride........... 3.3 Yo ·Hum8n immunodeficiency virus, Type 1 (HIV-l) INERT INGR~DIENTS .................. 96.7% KEEP OUT OF REACH OF CHILDREN DANGER See back panel for additional precautionary -

Safer Disinfectant Use During the COVID-19 Pandemic
Safer Disinfectant Use During the COVID-19 Pandemic sing disinfectants on surfaces in your home or workplace can kill disease causing germs (bacteria and viruses), Ubut they may also have health risks. For example, many common disinfectants (like bleach, many disinfectant wipes) have chemicals in them that can cause or worsen asthma. no If someone If in your you can’t one is house If is or access safer sick at sick home: suspected products to be sick: Clean surfaces in your Clean surfaces, then disinfect If you don’t have access to a house with an all-purpose using one of the safer disinfec microfiber cloth, wash sponges or cleaner or soap, and a tants from the EPA’s Design for towels after every surface cleaned: microfiber cloth (available the Environment antimicrobial Clean sponges by online, in grocery stores pesticide list. and at big box stores). This washing in the dishwasher, or will get rid of most of the Look for these safer active soaking for one minute in germs on a surface and ingredients: 1/2 teaspoon of bleach, or avoids excess exposure to Citric Acid microwaving non-metallic, disinfectants. Hydrogen Peroxide soaking wet sponges for one minute. Disinfect after cleaning L-lactic acid surfaces that you touch Ethanol Wash towels in a basin or washing machine. when returning from Isopropanol the outdoors, prior to Peroxyacetic acid If you only have access to washing hands. or quaternary ammonia- Sodium Bisulfate. bleach based disinfectants: Apply to the surface and per the leave glistening wet for the Dilute disinfectants time listed on the product label. -

COVID-19: Guidelines on Disinfection of Common Public Places Including Offices
COVID-19: Guidelines on disinfection of common public places including offices Scope: This document aims to provide interim guidance about the environmental cleaning /decontamination of common public places including offices in areas reporting COVID-19. Coronavirus Disease 2019 (COVID -19) is an acute respiratory disease caused by a novel Coronavirus (SARS-CoV-2), transmitted in most instances through respiratory droplets, direct contact with cases and also through contaminated surfaces/objects. Though the virus survives on environmental surfaces for varied period of time, it gets easily inactivated by chemical disinfectants. In view of the above, the following guidelines are to be followed, especially in areas reporting COVID-19. For ease of implementation the guideline divided these areas into (i) indoor areas, (ii) outdoor areas and (iii) public toilets. 1. Indoor areas including office spaces Office spaces, including conference rooms should be cleaned every evening after office hours or early in the morning before the rooms are occupied. If contact surface is visibly dirty, it should be cleaned with soap and water prior to disinfection. Prior to cleaning, the worker should wear disposable rubber boots, gloves (heavy duty), and a triple layer mask. Start cleaning from cleaner areas and proceed towards dirtier areas. All indoor areas such as entrance lobbies, corridors and staircases, escalators, elevators, security guard booths, office rooms, meeting rooms, cafeteria should be mopped with a disinfectant with 1% sodium hypochlorite -

Hydrogen Peroxide Cleaner Disinfectant Spray 32 Oz
Hydrogen Peroxide Cleaner Disinfectant Spray 32 oz. Spray and 128 oz. Economical Refill Now EPA-registerd to kill microorganisms on hard & soft surfaces Fast kill times on hard and soft surfaces Clorox Healthcare® Hydrogen Peroxide Cleaner Disinfectant Spray is engineered with a patented hydrogen peroxide formula for fast kill times on hard and soft surfaces, cleaning power, broad surface compatibility and no harsh chemical odors or fumes. Hard Surfaces: Powerful cleaning and some of the fastest disinfecting times since bleach* • Fast kill times on 43 bacteria and viruses • Cleans bathroom soil 3x faster than Virex® TB Spray • Ready to use • Cleans bathroom soil 36% faster than Cavicide™ • One-step cleaning and disinfecting Soft Surfaces†: Kills bacteria in just 30 seconds • Simply spray on and let dry. Bacteria will be killed in 30 • Use on high-touch soft surfaces in your facility, such as seconds. chairs, couches, rugs, curtains, cushions and mattresses. Compare Clorox Healthcare® Hydrogen Peroxide to Competitors Clorox Healthcare® Hydrogen Peroxide Virex® TB Spray Cavicide™ Oxivir TB Cleaner Disinfectant Spray Bacteria contact 30 seconds – 1 minute 3 minutes 3 minutes 1 minute time, excluding TB Virus contact times 30 seconds – 1 minute 30 seconds - 10 minutes 2 minutes 1 minute EPA registered to Yes Yes No Yes kill Norvirus? EPA-registered to kill bacteria on soft Yes No No No surfaces? *Based on aggregate 30-second non-TB bacteria and virus contact times for general disinfecting on Federal master labels as of 10/1/11. Use as directed. All claims based on data as of 10/1/11. † 100% polyester and 100% cotton Clorox Healthcare® Hydrogen Peroxide Cleaner Disinfectant Spray Soft Surfaces: EPA-approved to kill Enterobacter aerogenes and Staphylococcus aureus — representing gram-negative and gram-positive bacteria — on soft surfaces in just 30 seconds. -

Antiseptics in the Era of Bacterial Resistance: a Focus on Povidone Iodine
Therapeutic Perspective Antiseptics in the era of bacterial resistance: a focus on povidone iodine Jean-Marie Lachapelle*1, Olivier Castel2, Alejandro Fueyo Casado3, Bernard Leroy1, Giuseppe Micali4, Dominique Tennstedt1 & Julien Lambert5 Practice Points Increasing bacterial resistance to antibiotics makes the management of superficial skin infections a major medical challenge. Antiseptics have broader spectrums of antimicrobial activity and a reduced potential for selection of bacterial resistance, relative to antibiotics. Consequently, antiseptics are appropriate alternatives to antibiotics for the prevention and treatment of superficial skin infections. Of four widely used antiseptics (povidone iodine, polihexanide, chlorhexidine and octenidine), povidone iodine has a particularly broad spectrum of antimicrobial activity that includes Gram-positive and Gram-negative bacteria, bacterial spores, fungi, protozoa and viruses. Widespread and extended use of povidone iodine is not associated with the selection of resistant bacterial strains. In contrast, bacterial resistance to chlorhexidine, quaternary ammonium salts, silver and triclosan has been documented. Regarding duration of effect on healthy skin, chlorhexidine is active for 1–4 h, whereas solutions of povidone iodine are active for 12–14 h. Aqueous and hydroalcoholic formulations of povidone iodine have good skin tolerance. Povidone iodine scrub has better skin tolerance than soap formulations of chlorhexidine and quaternary ammonium compounds (e.g., benzalkonium chloride and -

Disinfectant and Antiseptics Pdf
Disinfectant and antiseptics pdf Continue Antiseptics and disinfectants are very similar in that they are both used to kill microorganisms. They differ from each other, albeit in the composition of them, as well as their use. Antiseptics are used on living organisms, such as human skin, to kill any microorganisms living on the surface of the body. Disinfectants are used on non-living things such as countertops and handrails to kill microorganisms living on this inanimate surface. Antiseptics tend to have a lower concentration of a particular biocide, which is used in this product to clean the surface than that of a disinfectant. Since disinfectants are not intended for use on living tissues, but rather inanimate surfaces, they can use a higher concentration of biocide in the product, since there is no skin or tissue to worry about irritants. Antiseptics require a lower concentration of biocides, as too high concentrations of some biocides can cause a large amount of skin irritation. Some examples of antiseptics are mouthwash or hand sanitizer, both of which are safe for contact with your skin and also capable of being extremely effective in killing large numbers of microorganisms. Alcohol, bleach and formaldehyde are examples of various types of disinfectants used to kill microorganisms on the surface of any non-living objects. It is important that people know the difference between antiseptics and disinfectants, as they are both used for similar things, but in different ways. The use of disinfectant as an antiseptic is likely to irritate this tissue. In addition, the use of antiseptic as a disinfectant may result in less sufficient work to clean this surface due to the lower concentration of the biocide.