Applications of Ultraviolet Germicidal Irradiation Disinfection in Health Care Facilities: Effective Adjunct, but Not Stand- Alone Technology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
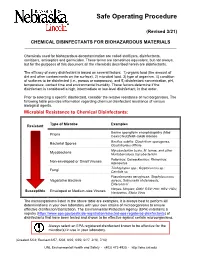
Chemical Disinfectants for Biohazardous Materials (3/21)
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -
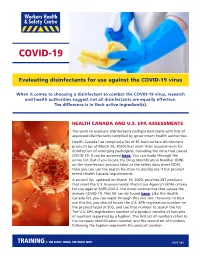
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Effects of Acute and Chronic Gamma Irradiation on the Cell Biology and Physiology of Rice Plants
plants Article Effects of Acute and Chronic Gamma Irradiation on the Cell Biology and Physiology of Rice Plants Hong-Il Choi 1,† , Sung Min Han 2,†, Yeong Deuk Jo 1 , Min Jeong Hong 1 , Sang Hoon Kim 1 and Jin-Baek Kim 1,* 1 Advanced Radiation Technology Institute, Korea Atomic Energy Research Institute, Jeongeup 56212, Korea; [email protected] (H.-I.C.); [email protected] (Y.D.J.); [email protected] (M.J.H.); [email protected] (S.H.K.) 2 Division of Ecological Safety, National Institute of Ecology, Seocheon 33657, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-63-570-3313 † Both authors contributed equally to this work. Abstract: The response to gamma irradiation varies among plant species and is affected by the total irradiation dose and dose rate. In this study, we examined the immediate and ensuing responses to acute and chronic gamma irradiation in rice (Oryza sativa L.). Rice plants at the tillering stage were exposed to gamma rays for 8 h (acute irradiation) or 10 days (chronic irradiation), with a total irradiation dose of 100, 200, or 300 Gy. Plants exposed to gamma irradiation were then analyzed for DNA damage, oxidative stress indicators including free radical content and lipid peroxidation, radical scavenging, and antioxidant activity. The results showed that all stress indices increased immediately after exposure to both acute and chronic irradiation in a dose-dependent manner, and acute irradiation had a greater effect on plants than chronic irradiation. The photosynthetic efficiency and growth of plants measured at 10, 20, and 30 days post-irradiation decreased in irradiated plants, Citation: Choi, H.-I.; Han, S.M.; Jo, Y.D.; Hong, M.J.; Kim, S.H.; Kim, J.-B. -

Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic
Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic Vickie Leonard, PhD Environmental Health in Early Care and Educaon Project, Western States Pediatric Environmental Health Specialty Unit (WSPEHSU) 1 Why Should We Be Concerned about Environmental Health in ECE? 2 Why Should We Be Concerned about Environmental Health in ECE? • There are 8 million children in child care centers in the U.S. A child may spend up to 12,500 hours in an ECE facility. A million child care providers work in these centers in the U.S. Half are child-bearing age. • Many toxicants found in child care facilities are not addressed in state child care health and safety regulations. • No agency at the state or federal level is charged with ensuring children’s health and safety in and around schools and ECE facilities. • No systematic means exists for collecting data on environmental exposures in these buildings. • Teachers have more protection in these buildings (unions, OSHA) than children do 3 Why Should We Be Concerned about Environmental Health in ECE? • Many people think that adults and children are exposed to, and affected by, toxic chemicals in the same way. • This is not the case. • Children • have higher exposures to toxicants in the environment, • are more vulnerable to the effects of those toxicants than adults. 4 Cleaning and Disinfec?ng Products: A Major Source of Exposure in Child Care and Schools • Products used to clean, sanitize and disinfect child care facilities and schools are a good example of the pervasive and unregulated use of toxic chemicals that put the health of our children at risk. -

Effects of Gamma-Irradiation of Seed Potatoes on Numbers of Stems and Tubers
Netherlands Journal of Agricultural Science 39 (1991) 81-90 Effects of gamma-irradiation of seed potatoes on numbers of stems and tubers A. J. HAVERKORT1, D. I. LANGERAK2 & M. VAN DE WAART1 1 Centre for Agrobiological Research (CABO-DLO), P.O. Box 14, NL 6700 AA Wagenin- gen, Netherlands 2 State Institute for Quality Control of Agricultural Products (RIKILT), P.O. Box 230, NL 6700 AE Wageningen, Netherlands Received 28 november 1990; accepted 8 February 1991 Abstract In field trials with the cultivars Bintje, Jaerla and Spunta, whose seed potatoes were treated with gamma-rays from a ^Co source with doses varying from 0.5 to 27 Gy, tuber yield, har vest index, and number of stems and tubers were determined. A dose of 3 Gy increased the number of tubers by 30 % in Spunta in two out of three trials and by 17 % in one trial in Jaer la, but it did not increase number of tubers in Bintje. Doses of 9 or 10 Gy did not influence the number of tubers nor stems, and decreased harvest index. A dose of 27 Gy yielded off-type plants with reduced yield and number of tubers. Gamma-radiation affected the growth of the apex of the sprout allowing lateral buds or divisions of the affected apex to develop into stems. To achieve larger numbers of tuber-bearing stems, tubers should preferably be irra diated at the start of sprout growth, about 5 months before planting. Keywords: harvest index, gamma irradiation, seed potatoes Introduction Effects of different doses of gamma-rays on potato tubers have been studied exten sively, especially in the 1960s. -

Industrial Applications of Electron Accelerators
Industrial applications of electron accelerators M.R. Cleland Ion Beam Applications, Edgewood, NY 11717, USA Abstract This paper addresses the industrial applications of electron accelerators for modifying the physical, chemical or biological properties of materials and commercial products by treatment with ionizing radiation. Many beneficial effects can be obtained with these methods, which are known as radiation processing. The earliest practical applications occurred during the 1950s, and the business of radiation processing has been expanding since that time. The most prevalent applications are the modification of many different plastic and rubber products and the sterilization of single-use medical devices. Emerging applications are the pasteurization and preservation of foods and the treatment of toxic industrial wastes. Industrial accelerators can now provide electron energies greater than 10 MeV and average beam powers as high as 700 kW. The availability of high-energy, high-power electron beams is stimulating interest in the use of X-rays (bremsstrahlung) as an alternative to gamma rays from radioactive nuclides. 1 Introduction Radiation processing can be defined as the treatment of materials and products with radiation or ionizing energy to change their physical, chemical or biological characteristics, to increase their usefulness and value, or to reduce their impact on the environment. Accelerated electrons, X-rays (bremsstrahlung) emitted by energetic electrons, and gamma rays emitted by radioactive nuclides are suitable energy sources. These are all capable of ejecting atomic electrons, which can then ionize other atoms in a cascade of collisions. So they can produce similar molecular effects. The choice of energy source is usually based on practical considerations, such as absorbed dose, dose uniformity (max/min) ratio, material thickness, density and configuration, processing rate, capital and operating costs. -

Bio-9 a Comparison of Y-Irradiation and Microwave Treatments on the Lipids and Microbiological Pattern of Beef Liver
Seventh Conference of Nuclear Sciences & Applications 6-10 February 2000, Cairo, Egypt Bio-9 A comparison of y-irradiation and microwave treatments on the lipids and microbiological pattern of beef liver Farag, R. S .*, Z. Y. Daw2, Farag , S.A 3 and Safaa A. E. ABD El-Wahab3. / Biochemistry Department, Faculty of Agriculture, Cairo University, Giza - Egypt. 2 Microbiology Department. Faculty of Agriculture. Cairo University, Giza - Egypt. 3 Food irradiation Department, National Center for Radiation Research and Technology, Cairo - Egypt. ABSTRACT EG0100123 The effects of y-irradiation treatments (0, 2.5, 5 and, 10 kGy) and microwaves generated from an oven at low and defrost settings for 0.5 , 1 and 2 min on the chemical composition and microbiological aspects of beef liver samples were studied . The chemical and microbiological analyses were performed on the non-treated and treated beef liver immediately after treatments and during frozen storage (-18°C) for 3 months. The chemical analyses of beef liver Hpids showed that acid, peroxide and TBA(Thiobarbituric acid ) values were slightly increased after irradiation treatments and also during frozen storage (-18°C). On the contrary, iodine value of the treated beef liver was decreased. Irradiation treatments remarkably reduced the total bacterial counts in beef liver. The percent reduction of bacterial load for beef liver exposed to microwaves generated from an oven at defrost mode for 2 min and after 3 months at - 18°C was 62% . The bacterial load for beef liver exposed to y-irradiation at 10 kGy after 3 months at - 18°C was decreased by 98%. Hence, y-irradiation treatment was far better than microwave treatment for inhibiting the multiplication of the associated microorganisms with beef liver. -

Silver As a Drinking-Water Disinfectant
Silver as a drinking-water disinfectant Silver as a drinking-water disinfectant Alternative drinking-water disinfectants: silver ISBN 978-92-4-151369-2 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Alternative drinking-water disinfectants: bromine, iodine and silver. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. -

Beam–Material Interactions
Beam–Material Interactions N.V. Mokhov1 and F. Cerutti2 1Fermilab, Batavia, IL 60510, USA 2CERN, Geneva, Switzerland Abstract This paper is motivated by the growing importance of better understanding of the phenomena and consequences of high-intensity energetic particle beam interactions with accelerator, generic target, and detector components. It reviews the principal physical processes of fast-particle interactions with matter, effects in materials under irradiation, materials response, related to component lifetime and performance, simulation techniques, and methods of mitigating the impact of radiation on the components and environment in challenging current and future applications. Keywords Particle physics simulation; material irradiation effects; accelerator design. 1 Introduction The next generation of medium- and high-energy accelerators for megawatt proton, electron, and heavy- ion beams moves us into a completely new domain of extreme energy deposition density up to 0.1 MJ/g and power density up to 1 TW/g in beam interactions with matter [1, 2]. The consequences of controlled and uncontrolled impacts of such high-intensity beams on components of accelerators, beamlines, target stations, beam collimators and absorbers, detectors, shielding, and the environment can range from minor to catastrophic. Challenges also arise from the increasing complexity of accelerators and experimental set-ups, as well as from design, engineering, and performance constraints. All these factors put unprecedented requirements on the accuracy of particle production predictions, the capability and reliability of the codes used in planning new accelerator facilities and experiments, the design of machine, target, and collimation systems, new materials and technologies, detectors, and radiation shielding and the minimization of radiation impact on the environment. -
![Particle Accelerators and Detectors for Medical Diagnostics and Therapy Arxiv:1601.06820V1 [Physics.Med-Ph] 25 Jan 2016](https://docslib.b-cdn.net/cover/8515/particle-accelerators-and-detectors-for-medical-diagnostics-and-therapy-arxiv-1601-06820v1-physics-med-ph-25-jan-2016-558515.webp)
Particle Accelerators and Detectors for Medical Diagnostics and Therapy Arxiv:1601.06820V1 [Physics.Med-Ph] 25 Jan 2016
Particle Accelerators and Detectors for medical Diagnostics and Therapy Habilitationsschrift zur Erlangung der Venia docendi an der Philosophisch-naturwissenschaftlichen Fakult¨at der Universit¨atBern arXiv:1601.06820v1 [physics.med-ph] 25 Jan 2016 vorgelegt von Dr. Saverio Braccini Laboratorium f¨urHochenenergiephysik L'aspetto pi`uentusiasmante della scienza `eche essa incoraggia l'uomo a insistere nei suoi sogni. Guglielmo Marconi Preface This Habilitation is based on selected publications, which represent my major sci- entific contributions as an experimental physicist to the field of particle accelerators and detectors applied to medical diagnostics and therapy. They are reprinted in Part II of this work to be considered for the Habilitation and they cover original achievements and relevant aspects for the present and future of medical applications of particle physics. The text reported in Part I is aimed at putting my scientific work into its con- text and perspective, to comment on recent developments and, in particular, on my contributions to the advances in accelerators and detectors for cancer hadrontherapy and for the production of radioisotopes. Dr. Saverio Braccini Bern, 25.4.2013 i ii Contents Introduction 1 I 5 1 Particle Accelerators and Detectors applied to Medicine 7 2 Particle Accelerators for medical Diagnostics and Therapy 23 2.1 Linacs and Cyclinacs for Hadrontherapy . 23 2.2 The new Bern Cyclotron Laboratory and its Research Beam Line . 39 3 Particle Detectors for medical Applications of Ion Beams 49 3.1 Segmented Ionization Chambers for Beam Monitoring in Hadrontherapy 49 3.2 Proton Radiography with nuclear Emulsion Films . 62 3.3 A Beam Monitor Detector based on doped Silica Fibres . -

Infection Prevention & Control Chlorhexidine
Winnipeg Regional Health Authority Acute Care Infection Prevention & Control Manual INFECTION PREVENTION & CONTROL CHLORHEXIDINE GLUCONATE CONCENTRATION FOR HAND HYGIENE COMMUNICATION FORM PART 1: ISSUE & RECOMMENDATIONS Issue: The WRHA Infection Prevention and Control program (IP&C) was requested to research and recommend acceptable concentrations of chlorhexidine gluconate (CHG) (2% versus 4%) for hand hygiene in all programs within WRHA sites, to ensure appropriate products are being used, and facilitate standardization. Recommendations: Use 2% CHG hand cleansers for hand hygiene when antimicrobial hand soap is indicated. Do NOT use 4% CHG for hand hygiene as the minimal improvement in efficacy (from 2%), does not warrant the increased frequency of skin irritation and breakdown, which ultimately impedes effective hand hygiene practices. PART 2: BACKGROUND: DISCUSSION OF ISSUE, OPTIONS AND ANALYSIS & REFERENCES Discussion of Issue: There are several different hand hygiene products used within and between WRHA sites. All areas should adhere to recommended hand hygiene products, as determined by available evidence. There are differences in when specific hand hygiene products are indicated. It is important to identify the appropriate product to use for the appropriate reason, as supported by evidence. Options and Analysis: 1. CHG has a cumulative effect when applied to the skin. In hand hygiene, this effect remains and is sustained, especially when hand hygiene is repeated. 2% CHG is appropriate for hand antisepsis because of the cumulative effect.1 2. Literature regarding differences between 2% and 4% CHG identifies there is minimal difference in efficacy between 2% and 4% CHG for hand antisepsis and cleansing.2 3. The frequency of skin irritation is concentration dependent, with products containing 4% most likely to cause dermatitis when used frequently for hand antisepsis.