Pilot Study of the Multicentre Randomised Trial of H. Pylori Eradication and Pepsinogen Testing for Prevention of Gastric Cancer Mortality (The GISTAR Pilot Study)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
All Latvia Cemetery List-Final-By First Name#2
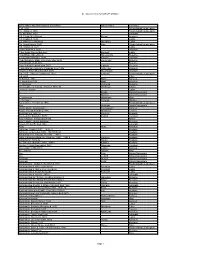
All Latvia Cemetery List by First Name Given Name and Grave Marker Information Family Name Cemetery ? d. 1904 Friedrichstadt/Jaunjelgava ? b. Itshak d. 1863 Friedrichstadt/Jaunjelgava ? b. Abraham 1900 Jekabpils ? B. Chaim Meir Potash Potash Kraslava ? B. Eliazar d. 5632 Ludza ? B. Haim Zev Shuvakov Shuvakov Ludza ? b. Itshak Katz d. 1850 Katz Friedrichstadt/Jaunjelgava ? B. Shalom d. 5634 Ludza ? bar Abraham d. 5662 Varaklani ? Bar David Shmuel Bombart Bombart Ludza ? bar Efraim Shmethovits Shmethovits Rezekne ? Bar Haim Kafman d. 5680 Kafman Varaklani ? bar Menahem Mane Zomerman died 5693 Zomerman Rezekne ? bar Menahem Mendel Rezekne ? bar Yehuda Lapinski died 5677 Lapinski Rezekne ? Bat Abraham Telts wife of Lipman Liver 1906 Telts Liver Kraslava ? bat ben Tzion Shvarbrand d. 5674 Shvarbrand Varaklani ? d. 1875 Pinchus Judelson d. 1923 Judelson Friedrichstadt/Jaunjelgava ? d. 5608 Pilten ?? Bloch d. 1931 Bloch Karsava ?? Nagli died 5679 Nagli Rezekne ?? Vechman Vechman Rezekne ??? daughter of Yehuda Hirshman 7870-30 Hirshman Saldus ?meret b. Eliazar Ludza A. Broido Dvinsk/Daugavpils A. Blostein Dvinsk/Daugavpils A. Hirschman Hirschman Rīga A. Perlman Perlman Windau Aaron Zev b. Yehiskiel d. 1910 Friedrichstadt/Jaunjelgava Aba Ostrinsky Dvinsk/Daugavpils Aba b. Moshe Skorobogat? Skorobogat? Karsava Aba b. Yehuda Hirshberg 1916 Hirshberg Tukums Aba Koblentz 1891-30 Koblentz Krustpils Aba Leib bar Ziskind d. 5678 Ziskind Varaklani Aba Yehuda b. Shrago died 1880 Riebini Aba Yehuda Leib bar Abraham Rezekne Abarihel?? bar Eli died 1866 Jekabpils Abay Abay Kraslava Abba bar Jehuda 1925? 1890-22 Krustpils Abba bar Jehuda died 1925 film#1890-23 Krustpils Abba Haim ben Yehuda Leib 1885 1886-1 Krustpils Abba Jehuda bar Mordehaj Hakohen 1899? 1890-9 hacohen Krustpils Abba Ravdin 1889-32 Ravdin Krustpils Abe bar Josef Kaitzner 1960 1883-1 Kaitzner Krustpils Abe bat Feivish Shpungin d. -

The Saeima (Parliament) Election
/pub/public/30067.html Legislation / The Saeima Election Law Unofficial translation Modified by amendments adopted till 14 July 2014 As in force on 19 July 2014 The Saeima has adopted and the President of State has proclaimed the following law: The Saeima Election Law Chapter I GENERAL PROVISIONS 1. Citizens of Latvia who have reached the age of 18 by election day have the right to vote. (As amended by the 6 February 2014 Law) 2.(Deleted by the 6 February 2014 Law). 3. A person has the right to vote in any constituency. 4. Any citizen of Latvia who has reached the age of 21 before election day may be elected to the Saeima unless one or more of the restrictions specified in Article 5 of this Law apply. 5. Persons are not to be included in the lists of candidates and are not eligible to be elected to the Saeima if they: 1) have been placed under statutory trusteeship by the court; 2) are serving a court sentence in a penitentiary; 3) have been convicted of an intentionally committed criminal offence except in cases when persons have been rehabilitated or their conviction has been expunged or vacated; 4) have committed a criminal offence set forth in the Criminal Law in a state of mental incapacity or a state of diminished mental capacity or who, after committing a criminal offence, have developed a mental disorder and thus are incapable of taking or controlling a conscious action and as a result have been subjected to compulsory medical measures, or whose cases have been dismissed without applying such compulsory medical measures; 5) belong -

The Family of Indriķis Blankenburgs (1887–1944) and Architectural Projects in the Turn of the Century
HISTORY OF ENGINEERING SCIENCES AND INSTITUTIONS OF HIGHER EDUCATION No. 2, Sept. 2018, p. 76.–91. 2018/2 doi: 10.7250/HESIHE.2018.006 THE FAMILY OF INDRIĶIS TURNBLANKENBURGS OF THE CENTURY (1887–1944) AND ARCHITECTURAL PROJECTS IN THE MĀRIS ZVAIGZNE* ALĪDA ZIGMUNDE, ILZE GUDRO Riga State German Grammar School Riga Technical University Summary. Indriķis Blankenburgs The graduate of the Department of Architecture (1913) of the Riga Polytechnic Institute (RPI), architect (1887–1944) is one of the best-known architects of school buildings in Latvia during the interwar years. Most of his more than 30 projected schools and other buildings are Blankenburgsstill used for the original purpose of the architect. Using I. Blankenburgs the documents of the Latvian State Historical Archives and library collections, the article follows the family and outlines the contribution of to school architectureKeywords: Indriķisand provides Blankenburgs the list of schoolsBlankenburgs designed by the architect. , the family, school building projects. Introduction Indriķis Blankenburg On 7 April 2017, a scholarly-practical conference «School Architect – 130» was held at the Riga State German Grammar School. It was marking the anniversary of the graduate of Riga Polytech- nic Institute andIndriķis reviewing Blankenburgs his performance and life activity. By studying less well-known pages of his life, the authors of the paper referred about the architect at the conference. The research was carried out by analysing the documents of the Latvian State Historical Archive, the Riga State German Grammar School Museum and the Natio- nal Library of Latvia, including articles in the periodicals. [email protected] * Corresponding author. E-mail: Māris Zvaigzne Alīda Zigmunde Ilze Gudro 76 © 2018 , , . -

Traditionele Ambachten in Het Oosten Van Letland 8 Dagen
www.boundlessinspiration.nl TRADITIONELE AMBACHTEN IN HET OOSTEN VAN LETLAND 8 DAGEN 21-28 juli 2019 899 EUR (exclusief vluchten) Highlights: Natuur, cultuur, ambachten, pottenbakken, weven, workshop brood bakken, geneeskrachtige kruiden, verblijf in een landhuis; inclusief bezoek aan de hoofdstad Riga. 1 www.boundlessinspiration.nl ALGEMEEN Houdt u van reizen, maar blijft u liever in Europa? Bent u dan op zoek naar nauwelijks bekende, exotische plekjes maar reist u liever wel in een (kleine) groep? Wilt u zich dan verdiepen in oude ambachten, en het liefst zelf ook creatief bezig zijn? Wilt u daarnaast bezienswaardigheden intenser beleven en reizen met mensen die dat ook leuk vinden? En hoort u deze nieuwe informatie liever van iemand die het land en de streek echt kent? Als u positief heeft geantwoord op de meeste vragen hierboven is deze reis echt iets voor u! Deze reis kijk ik altijd bijzonder naar uit, omdat we naar mijn vaderland Letland gaan. We gaan langs mooie bestemmingen en traditionele ambachtslieden in de onbekende regio Latgale, maar bezoeken ook highlights in de hoofdstad Riga. In Letland worden handwerk en ambachtelijk gemaakte producten en voorwerpen nog echt gewaardeerd, en ook veel beoefend. De verschillende regio’s in Letland kennen ook een veelheid aan ambachten en handwerktechnieken. We beginnen in de hoofdstad Riga, waar we al iets zullen zien en horen van de geschiedenis en culturele rijkdom van dit land. Daarna gaan wij kennis maken met de regio Latgale in het Oosten van het land, een regio die bekend staat om haar vele meren, natuur en pottenbakken. Maar naast deze ambacht gebeurt er hier nog veel meer, en leren wij er iets over weven, houtbewerking en ook over de ambachtelijke bereiding van traditionele gerechten. -

Dobrin Family
Dobrin family Yitskhak Dobrin #27854, b. c.1780, d. before 1859 in Latvia. Recorded as the patronymic of David Dobrin in the 1882 Family List in the village of Osun, near Daugavpils (Dvinsk), Latvia. Assumed to be the primogenitor also of the Dobrin family of Lutzin due to the prevelance of personal names common to both families. I. Yaakov Dobrin #22573, b. c.1800, d. before 1858 in Lutzin (now Ludza), Latvia.1 A. David Dobrin #27839, b. 1824,2 resided 1874 in Lutzin (now Ludza), Latvia,3 d. before 1896 in Lutzin (now Ludza), Latvia. He married Rasya (Riska) #27840, b. 1826, (daughter of Leizer #27846). Rasya: Listed in the 1897 census of Lutzin living with her son Moshe. 1. Yisrael Dobrin #27841, d. 1860.3 2. Moshe Dobrin #27842, b. 1851, occupation cabman. Listed in the 1897 census of Lutzin living at 44 Dokrorskaya Streer number 44, a wooden house covered with wood,cabman who owned one horse. He married Riva #27847, b. 1852 in Sebezh, Byelorussia, (daughter of Khaim #27848). a. Khaim Yisrael Dobrin #27849, b. 1877 in Lutzin (now Ludza), Latvia, occupation 1897 Lutzin (now Ludza), Latvia. b. Braina Dobrin #27851, b. 1879 in Lutzin (now Ludza), Latvia. c. Yaakov Dobrin #27853, b. 1885 in Lutzin (now Ludza), Latvia. d. Nakhman Dobrin #27850, b. 1889 in Lutzin (now Ludza), Latvia. e. David Dobrin #27852, b. 1896 in Lutzin (now Ludza), Latvia. 3. Yaakov Dobrin #27843, b. 1858. 4. Avraham Dobrin #27844, b. 1868. B. Avraham Dobrin, #22574, b. 1829 in Lutzin (now Ludza), Latvia,3 d. -

TB Laboratory Network in Latvia Ģirts Šķenders, Head of Bacteriological Laboratory, State Agency of Tuberculosis and Lung Diseases Key Requirements for Good Network
Organization of TB Laboratory Network in Latvia Ģirts Šķenders, Head of Bacteriological Laboratory, State Agency of Tuberculosis and Lung Diseases Key requirements for good network • Algorithm-based selection of high risk patients • Reliable, regular specimen transport • Infrastructure development and maintenance • Staff training and retention plans • Integrated internal QC and external QA • Rapid, effective communication of results (from Karin Wayer’s presentation at The Union world conference in Paris 2006) Key principles • Use existing resources (e.g. Primary Health Care services) • Collaborate with other programs (e.g. AIDS or Malaria) for specimen transport, supervision, EQA. • Accessible for patients, keep low patient costs • Good quality or not at all TB Laboratory Network in Latvia National Reference Laboratory Culture, Drug Susceptibility Tests, Culture Identification, Supervision, Staff training, and Quality control. Jekabpils Rezekne Liepaja Daugavpils Central prison Culture laboratory + Culture laboratory + Culture laboratory + Culture laboratory + Culture laboratory + Microscopy center Microscopy center Microscopy center Microscopy center Microscopy center “Lielberze” “Ceplisi” Culture laboratory + Culture laboratory MDR-TB hospitals Microscopy center +Microscopy center Saldus Talsi Ventspils Ludza Valmiera Aizkraukle Gulbene Microscopy Microscopy Microscopy Microscopy Microscopy Microscopy Microscopy center center center center center center center Tukums Madona Strenci Balvi Kraslava Preili Bauska Microscopy Microscopy Microscopy Microscopy Microscopy Microscopy Microscopy center center center center center center center Limbazi Microscopy center TB Laboratory Network in Latvia Microscopy Centers – integrated in Primary Health structures – Laboratories at policlinics and/or hospitals. All medical laboratories are audited and certified by HEALTH STATISTICS AND MEDICAL TECHNOLOGIES STATE AGENCY. Auditing criteria are based on international standards for testing and medical laboratories (ISO 17025, ISO 15189). -

The Railways of Latvia Toms Altbergs Karīna Augustāne Ieva Pētersone the RAILWAYS of LATVIA
The Railways of Latvia Toms Altbergs Karīna Augustāne Ieva Pētersone THE RAILWAYS OF LATVIA Translated by Daina Grosa UDK 656.2(474.3)(091) Ra 314 Foreword Th is book was published with the support of State Joint Stock Company “Latvijas dzelzceļš” Th e national railway company of Latvia — State Joint Stock Company Latvijas dzelzceļš which recently became a concern, is one of the nation’s largest companies and one of the strongest economically. Th e history of the railways in the territory of Latvia dates back 150 years. Latvian State Railways was founded on 5 August 1919. Th e Railway Central Board took on the task of transforming the railways that had been Design Jānis Jaunarājs devastated by World War I and the chaos that followed and over a 20 year Managing Editor Evija Veide period established one of the most extensive and modern railway networks Copy Editor Marianna Auliciema in Europe. Th e network was founded on the legacy of tsarist Russia, with over 800 km of railways constructed, and so a structurally well-balanced railway system was established. Th is provided domestic and transit trans- The photographs and documents used in this book have been sourced from the collections at the Power Industry Museum, National History Museum of port services to the east and the west. Working on the railways symbolised Latvia, Latvian Railway History Museum, October Railway Central Museum stability and being a railwayman became one of the most prestigious and and the Lithuanian Railway Museum as well as the private archives of Vladimirs Eihenbaums, Dainis Punculs, Arnis Dambis, Dzintra Rupeika, Manfred best-paid professions. -

Download Download
ESUKA – JEFUL 2017, 8–1: 41–59 INSIGHT INTO THE CITY/TOWN NAMES OF LATVIA Laimude Balode University of Helsinki, University of Latvia Abstact. The origin of place names is a research topic for linguists (or onomasticians) and geographers, but since ancient times a wide range of people have also been inter- ested in the subject. As Latvia is the closest neighbour to both Lithuania and Estonia, they share, to a large extent, a common history, as well as – because of this fact – a number of borrowed common words and names. This article is based on the toponym- ical material included in the short dictionary of Latvian geographical names entitled “No Abavas līdz Zilupei” (“From Abava to Zilupe. The origin of Latvian geographical names”), which was compiled by Laimute Balode and Ojārs Bušs and published in Rīga in 2015. It offers insights into the contemporary situation of Latvian oikonyms as well as providing comparisons of the names of inhabited places with their historical names. Keywords: onomastics, place names, Latvia DOI: https://doi.org/10.12697/jeful.2017.8.1.03 1. Introduction Today, Latvia has 9 cities and 67 towns (N=76) with town privi- leges. Naturally there are ancient cities, such as Rīga; founded in 1201, it has had town privileges since 1225. Other examples include Valmiera and Cēsis, which were granted town privileges in 1323, and Aizpute, Kuldīga, Ventspils, which were granted town status in 1378. In addition, Ludza was recorded in historical annals as early as in 1173, but town privileges were not granted until 1777. Then we must also consider the newest towns of Latvia: Jūrmala has been recognised as a town since 1956 and several inhabited places – Aknīste, Cesvaine, Ķegums, Pāvilosta, Saulkrasti, Seda, Stende, and Vangaži – were adjudged as towns in the first years of the second independence – from 1991. -

A Programme to Promote the Information Society: The
OVERVIEW ister with special portfolio for E-gov- A Programme to Promote ernance, Jånis Reirs, to discuss the ministry s investment in promoting the recognizability of the certificates. the Information Society: Seminars were organised in September in Prei¬i, Kråslava, Val- miera and Ventspils, allowing people The First Results of the to learn about the launch of training in Latvia’s regions, about the train- ing programme, and about the proce- Latvija@Pasaule Project dure for signing up for the courses. Lilita VÏksna, Data Media Group, Latvia LIKTA RESEARCH ON IT USE AND DIGITAL SKILLS A press conference was held in September of this year at which representatives of The aim was to collect the infor- the Latvian Information and Communications Technology Association (LIKTA) mation that is needed for the success- announced that the first, preparatory phase of the Latvija@Pasaule ful implementation of the project, (Latvia@World) project has been completed successfully. Work is continuing on the drafting and localisation of educational materials. thus learning the gap which exists be- tween the demand for computer and Internet skills on the one hand, and One of the goals in the first phase banka, Dzintars Kalniñß, said at the the knowledge and skills which of the Latvija@Pasaule project was to press conference that his bank, too, would-be employees can offer in the learn about the situation in Latvia’s would be offering financial assistance labour market. Employers at 278 regions. Since January 2005 LIKTA to the Latvija@Pasaule project. companies were studied in the four started the the project “Training in People who complete the training aforementioned regions that were Computer and Internet Use for course will receive a certificate to at- surveyed. -

The Republic of Latvia and the Russian Federation Treaty on the State Border of Latvia and Russia
The Republic of Latvia and the Russian Federation Treaty on the State Border of Latvia and Russia 27 March 2007 The Republic of Latvia and the Russian Federation, hereinafter referred to as "the Parties", having mutual respect for each other's sovereignty and independence, equality of rights and territorial integrity, confirming their loyalty to the principles of the United Nations and the Organization for Security and Co-operation in Europe, recognising the beneficial effect on the further development of good neighbourly relations of legally formulating the State border of the Republic of Latvia and the Russian Federation, based on the goodwill of both Parties, have agreed as follows: Article 1 For the purposes of this Treaty, the expression "Latvia-Russia State border" (hereinafter: State border or border") shall mean the line, and the surface vertically corresponding to such line, which separates the territories of the two sovereign states of the Republic of Latvia and the Russian Federation (the land, waters, subterranean land and airspace). Article 2 In accordance with the standards of international law, and on the basis of the agreement achieved during negotiations, the Parties have determined the State Border between the Republic of Latvia and the Russian Federation. The Latvia-Russia State border shall be that which is set out in the "Republic of Latvia and Russian Federation State Border Description" and which is indicted in red on the "Republic of Latvia and Russian Federation State Border Delimitation Map" on a scale of 1:50,000 (hereinafter: "Delimitation Map"). The Republic of Latvia and Russian Federation State Border Description (Attachment 1), and the 1:50,000 scale Delimitation Map (Attachment 2) shall each be an inseparable part of this Treaty. -

Rural Development Programme for Latvia 2007–2013
RURAL DEVELOPMENT PROGRAMME FOR LATVIA 2007–2013 CONTENTS 1. TITLE OF RURAL DEVELOPMENT PROGRAMME .................................................. 7 2. MEMBER STATE AND ITS ADMINISTRATIVE REGION ......................................... 8 2.1. Geographical area covered by the programme ............................................................................. 8 2.2. Regions classified as ‘Convergence’ Objective ............................................................................. 8 3. ANALYSIS OF THE SITUATION IN TERMS OF STRENGTHS AND WEAKNESSES, THE STRATEGY CHOSEN TO MEET THEM AND EX- ANTE EVALUATION ............................................................................................................. 9 3.1. Analysis of the situation in terms of strengths and weaknesses ................................................... 9 3.1.1. The general socio-economic context of the geographical area ........................................... 9 3.1.1.1 Territory ........................................................................................................................ 9 3.1.1.2 Population ................................................................................................................... 13 3.1.1.3 Macroeconomic situation ............................................................................................ 14 3.1.1.4 Employment................................................................................................................ 16 3.1.2. Description of agriculture, forestry and -
Russian Minority in Latvia
Russian Minority in Latvia EXHIBITON CATHALOG Foundation of MEP Tatjana Ždanoka “For Russian Schools”, Riga-Brussels 2008-2009 Riga-Brussels 2008-2009 The Exhibition “Russian Minority in Latvia” is supported by the Foundation of MEP Tatjana Ždanoka “For Russian Schools”, by European Parliament political group “Greens/EFA” as well as the External Economic and International Relations Department of Moscow City Government and the Moscow House of Fellow Nationals. Author Team: Tatjana Feigman and Miroslav Mitrofanov (project managers) Alexander Gurin, Illarion Ivanov, Svetlana Kovalchuk, Alexander Malnach, Arnold Podmazov, Oleg Puhlyak, Anatoly Rakityansky, Svetlana Vidyakina Design by Victoria Matison © Foundation “For Russian Schools” ISBN 978-9984-39-661-3 The authors express their gratitude for assistance and consultation to the following: Metropolitan of Riga and all Latvia Alexander Kudryashov and priest Oleg Vyacheslav Altuhov, Natalia Bastina, Lev Birman, Valery Blumenkranz, Olga Pelevin, Bramley (UK), Vladimir Buzayev, Valery Buhvalov, Dzheniya Chagina, Yury Chagin, Chairman of the Central Council of Latvian Pomorian Old Orthodox Church Biruta Chasha, Alexey Chekalov, Irina Chernobayeva, Nataliya Chekhova, Elina Aleksiy Zhilko, Chuyanova, Vitaly Drobot, Yevgeny Drobot, Dmitry Dubinsky, Nadezhda Dyomina, Editor in chief of daily newspaper “Vesti Segodnya” Alexander Blinov, the Vladimir Eihenbaum, Xenia Eltazarova, Zhanna Ezit, Lyudmila Flam (USA), vice-editor in chief Natalya Sevidova, journalists Yuliya Alexandrova and Ilya Svetlana