AHIJB 10 January 2018 Combined.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Emergency Department Activity
NHS Scotland - Emergency Department Activity Attendances and Performance against the 4-hour Waiting Time Standard This is an ISD Scotland National Statistics release. The Scottish Government waiting time standard for emergency departments is that 98 % of all attendances should be seen within 4 hours. The figures presented in these tables detail the performance of each individual site and NHS board against the standard. Time Period: Apr-10 to Mar-11 Source: A&E data mart, ISD Scotland Date: 07 May 2012 List of Tables Table 1: Attendances and performance against 4-hour standard, Apr-10 to Mar-11 Total attendances, number of attendances breaching standard and attendances meeting standard (number and percentage). Figures are given at site and NHS Board level. Table 2: Attendances, Apr-10 to Mar-11 Summary table of attendances only. Figures are given at site and NHS Board level. Table 3: Performance against 4-hour standard, Apr-10 to Mar-11 Summary table of percentage of attendances meeting standard. Figures are given at site and NHS Board level. Notes: 1) The waiting time is defined as the time of arrival until the time of discharge, admission or transfer. 2) New presentations only; excludes planned return and recall attendances. 3) There are two types of site that provide emergency care; • ED - Emergency Departments; sites that provide a 24 hour emergency medicine consultant led service • MIU/Other - sites including minor injuries units (MIU), small hospitals and health centres in rural areas that carry out emergency department related activity and are GP or Nurse led. They may or may not be open 24 hours. -

NHS Tayside CONSULTANT PSYCHIATRIST
NHS Tayside CONSULTANT PSYCHIATRIST General Adult Psychiatry VACANCY Consultant in General Adult Psychiatry (x2 posts) Wedderburn House / Carseview Centre: Dundee Community Mental Health Team 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent NHS Tayside is looking for committed, innovative and enthusiastic Consultant Psychiatrists (full or part time) to join our Community Mental Health Team based in Dundee the ‘City of Discovery’. These posts include opportunities to see and treat a wide variety of psychiatric disorders in patients aged from eighteen to sixty-five years old, with the support of our enthusiastic and well staffed multi-disciplinary and multi- agency social work and health Community Mental Health Team with access to our 20 bed inpatient unit. We have local drug and alcohol, forensic, eating disorder, liaison and advanced intervention services as well as psychotherapy and psychology services available for our patients, and enjoy excellent relations with our local General Practitioners and voluntary service colleagues. There are many learning and training opportunities, including the teaching and supervision of 4th year medical students and Specialty Trainees attached to our team. There is a monthly continuing professional development programme and other continuing professional development will also be encouraged. Active involvement in service improvement is available through membership of our Service Improvement Group. We have close links with the University of Dundee division of Neuroscience where academic and research opportunities are available: http://medicine.dundee.ac.uk/medical-research-institute/divisions/division- neuroscience. Dundee is a coastal city on the Firth of Tay estuary in eastern Scotland. Its regenerated waterfront has the new Victoria and Albert Museum which stands on the banks of the Tay and two nautical museums: RRS Discovery, Captain Scott’s Antarctic expedition ship, and 19th-century warship, HM Frigate Unicorn. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

The Angus Care Model
THE ANGUS CARE MODEL Let’s keep the conversation going Thank you for your interest in the development of the Angus Care Model. During week beginning 16 October 2017 people from across Angus attended drop-in information sessions held in Forfar, Carnoustie, Montrose and Arbroath. These events gave locals the chance to talk to health and social care professionals. Our conversations focused on the challenges facing services, the opportunities for change and how we can together build a future Angus Care Model that provides the best possible care to the most people possible. The majority of people (85%) who attended the meetings found them helpful and informative. Whilst a small number of people commented that they would have preferred a formal meeting, people (94%) overwhelmingly felt that they had been given an opportunity to comment and offer their opinion. When arranging future meetings we will take account of people's suggestions and improve the way we raise awareness about the meetings. We were asked to share the information that was on display. In addition to talking to staff and have many of their questions answered, we also invited people to write down questions and leave comments. We have done our best to answer as many of the questions as possible. Please take some time to consider the information contained below and get involved in the conversation by completing a short survey https://www.surveymonkey.co.uk/r/WDFV53D or by contacting us on [email protected] We look forward to continuing our conversation with you in the very near future. -

S Letter, for Information, to the Convenor of the Health and Sport Committee and the Auditor General
Director-General Health & Social Care and Chief Executive NHSScotland Paul Gray T: 0131-244 2790 E: [email protected] Jackie Baillie Acting Convenor Public Audit and Post-legislative Scrutiny Committee Scottish Parliament [email protected] 27 June 2017 Dear Ms Baillie Following my last letter to the Public Audit and Post-legislative Scrutiny Committee on 17 May, please find attached a copy of the Staging Report submitted to me today by the NHS Tayside Assurance and Advisory Group, chaired by Professor Sir Lewis Ritchie. I have considered the findings and I am content with the recommendations. I attach the letter which I am sending today to the Chair of NHS Tayside, setting out my decision to appoint a Transformation Support Team, reporting to me, to work alongside NHS Tayside’s Executive Team to implement the required scale of transformational change across the organisation at pace. The Committee will wish to be aware that the AAG report makes clear that NHS Tayside are delivering well in a number of key areas, and asks the Scottish Government to consider the potential impact of their being required to repay the £33.2m of brokerage outstanding. I am therefore suspending the requirement for NHS Tayside to repay outstanding brokerage meantime, to avoid the prospect of adverse impacts on patient safety, quality and delivery. I will return to this issue once NHS Tayside’s transformation plans are further developed. I am also copying this letter, for information, to the Convenor of the Health and Sport Committee and the Auditor General. Yours sincerely Paul Gray St Andrew’s House, Regent Road, Edinburgh EH1 3DG www.gov.scot Director-General Health & Social Care and Chief Executive NHSScotland Paul Gray T: 0131-244 2790 E: [email protected] John Connell, Chair NHS Tayside 27 June 2017 ___ Dear John Please find attached the final report of the NHS Tayside Assurance and Advisory Group (AAG), chaired by Professor Sir Lewis Ritchie. -

SH-BBV-Training-Programme-2019
1 Dates for 2019 – 2020 April 2019 May 2019 June 2019 26th April : 9.15am-1.00pm 20th May: 9.15am- 4.30pm Addressing 3rd June : 9.15am-1.00pm Condom Distribution Scheme for Young the Sexual Health Needs of LGBT Condom Distribution Scheme for Young People Community People Seminar Room 4, Perth Royal Infirmary, Room C, Improvement Academy, Committee Room 2, Level 10, Ninewells Perth Ninewells Hospital, Dundee 10 th June: 10:00am-3:30pm Introduction to Sexual and Reproductive Health Room D, Improvement Academy, Ninewells July 2019 August 2019 September 2019 5th August : 10am-3:30pm Safe 2nd September : 9:15am-1.00pm Relationships and the law on sex for the Condom Distribution Scheme for Young under 16s People Room A, Improvement Academy, Rescobie Room, Whitehills, Forfar Ninewells, Dundee 5th & 6th September : 9.30am- 4.30pm 15th & 16th August : 9.30 4.30pm Sexual Sexual Health, BBV & Harm Reduction 2 Health, BBV & Harm Reduction 2 Day day training for staff working with Training for Staff Working with Vulnerable Vulnerable Young People Young People Seminar Room 4 and Board Room Perth Room A, Improvement Academy, Royal Infirmary Ninewells, Dundee 12th September : 10.00am-4.00pm Sex, Drugs, & BBVs Board Room, Arbroath Infirmary, Arbroath October 2019 November 2019 December 2019 2nd& 3rd October : 9.30am- 4.30pm Sexual 7th November : 10.00am-4.00pm 5th December : 10.0am-4.00pm Health, BBV & Harm Reduction 2 Day Sex , Drugs & BBV Sex Drugs & BBV Training for Staff Working with Vulnerable Seminar Room 4, Perth Royal Infirmary Room C, Improvement -

Deliverable D6 FAMS Trials Report: Testing and Evaluation
EUROPEAN COMMISSION INFORMATION SOCIETIES TECHNOLOGY (IST) PROGRAMME FAMS IST-2001-34347 FLEXIBLE AGENCY FOR COLLECTIVE, DEMAND RESPONSIVE MOBILITY SERVICES Deliverable D6 FAMS Trials Report: Testing and Evaluation Document Type: Deliverable Deliverable Number: D6 Deliverable Title: FAMS Trials Report: Testing and Evaluation Work Package WP5 Comparative Evaluation & Business Case Assessment Editor Pekka Eloranta, Mobisoft Dissemination Level Public Version 1.2 Circulation FAMS Consortium Commission Services Contractual date 29th July 2003 of Delivery Planned date 12thth November 2003 of Delivery Keywords Validation, Trial, Testing, Evaluation, Take-up Action, Telematics, Demand Responsive Transport Services, Multimodal, Public Transport DOCUMENT HISTORY Version Date Initials Revised Short description sections 0.1 31/07/03 PE, BM, All Structure of the Deliverable and the first draft AF, MB, established. NdV, CB 0.2 21/10/03 PE, BM, All Site inputs added, revised and shortened AF, MB, NdV, CB 1.0 29/10/03 PE All Deliverable shortened 1.1 03/11/03 JFM All UNEW comments 1.2 12/11/03 BM, JFM, 1, 4.1, 7.1 Minor revisions PE 2 Version number 1.2 Date 12th November 2003 Editors Pekka Eloranta Contributors to this report Giorgio Ambrosino, ATAF Claudia Binazzi, ATAF Marco Boero, Softeco Sismat Neri di Volo, ATAF Andrea Ferrari, SITA Jarno Kanninen, Mobisoft Brian Masson, Angus Transport Forum Brendan Finn, ETTS Jenny Mageean, UNEW 3 TABLE OF CONTENTS EXECUTIVE SUMMARY..................................................................................................6 -

West Practice Springfield Medical Centre Freedom of Information
West Practice Springfield Medical Centre Freedom of Information Publication Scheme 2014 Index Section 1 Introduction Section 2 About West practice, Springfield Medical Centre Section 3 Our functions and services Section 4 How we take decisions and what we have decided Section 5 What we spend and how we spend it Section 6 Accessing information under the scheme Section 7 Information that we may withhold Section 8 Our charging policy Section 9 Our copyright policy Section 10 Our records management and disposal policy Section 11 Feedback Section 12 Complaints Section 13 How to access information which is not available under this scheme Section 14 Classes of information Section 1: Introduction The Freedom of Information (Scotland) Act 2002 requires Scottish public authorities to produce and maintain a publication scheme. Authorities are under a legal obligation to: • Publish the classes of information they make routinely available • Tell the public how to access the information and what it might cost West Practice, Springfield Medical Centre has adopted the Model Publication Scheme 2014 produced by the Scottish Information Commissioner. The scheme has the Commissioner’s approval until 31 May 2018. You can see the model publication scheme on the Commissioner’s website at www.itspublicknowledge.info/mps or by contacting us at the address provided below. The purpose of this Guide to Information is to: • allow you to see what information is available (and what is not available) in relation to each class • state what charges may be applied • explain how you can find the information easily. • provide contact details for enquiries and to get help with accessing the information • explain how to request information we hold that has not been published. -
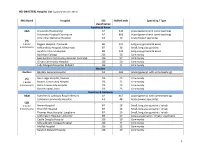
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Trust Name Site Principal Investigator RM / Coordinator Airedale NHS
PAN-COVID project partners (planning funding application, study conduct) Dr Mandish Dhanjal Imperial College Healthcare NHS Trust Professor Tg Teoh Imperial College Healthcare NHS Trust, Imperial College London Dr Alison Wright Royal Free NHS Foundation Trust, London Professor Liona Poon Chinese University of Hong Kong Alison Perry Manager, Women's Health Research Centre, Imperial College London Dr Caroline Shaw Clincial Lecturer, Imperial College London Professor Dirk Timmerman KU Leuven, Belgium Professor Neil Ferguson Imperial College London Professor Neena Modi Imperial College London PAN-COVID Investigators Trust Name Site Principal Investigator RM / Coordinator Airedale NHS Foundation Trust Soum Nallapeta emma dooks Aneurin Bevan University Health Board Royal Gwent Hospital Emma Mills Tracy James Ashford and St Peter's Hospitals NHS Foundation Trust St Peter’s Hospital Beth Peers Hayley Tarft Barnsley Hospital NHS Foundation Trust Sarah Stables Allison Daniels Barts Health NHS Trust Royal London Hospital Dr Stamatina Iliodromiti Megan Parrott Barts Health NHS Trust Newham Hospital Tabitha Newman Barts Health NHS Trust Whipps Cross Hospital Amy Thomas Betsi Cadwaladr University Health Board Wrexham Maelor Maggie Armstrong SARAH DAVIES Betsi Cadwaladr University Health Board Ysbyty Gwynedd Hilary Owen Betsi Cadwaladr University Health Board Glan Clwyd MEL HOLLINS Birmingham Women's and Children's NHS Foundation Birmingham Women’s Hospital Shanteela Mccooty Amy Woodhead Black Country Healthcare NHS Foundation trust Dorothy Pattison -

NHS Tayside CONSULTANT PSYCHIATRIST
NHS Tayside CONSULTANT PSYCHIATRIST General Adult Psychiatry VACANCY Consultant in General Adult Psychiatry Perth Community Mental Health Team 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent NHS Tayside is seeking a Consultant Psychiatrist (full or part time) to join our Community Mental Health Team based in Perth Scotland. This post will include opportunities to see and treat a wide variety of psychiatric disorders in patients aged from eighteen to sixty-five years old, with the support of our enthusiastic and well staffed multi-disciplinary and multi-agency social work and health Community Mental Health Team with access to our 24 bed inpatient unit. Our staff work passionately towards achieving NHS Tayside's vision, aim and values: http://www.nhstayside.scot.nhs.uk/WorkingWithUs/WhyWorkforNHSTayside/PROD_ 204621/index.htm We have local drug and alcohol, forensic, eating disorder, liaison and advanced intervention services as well as psychotherapy and psychology services available for our patients, and enjoy excellent relations with our local General Practitioners and voluntary service colleagues. There are many learning and training opportunities, including the teaching and supervision of 4th year medical students and Specialty Trainees attached to our team. There is a monthly continuing professional development programme and other continuing professional development will also be encouraged. Active involvement in service improvement is available through membership of our Service Improvement Group. We have close links with the University of Dundee division of Neuroscience where academic and research opportunities are available: http://medicine.dundee.ac.uk/medical-research-institute/divisions/division- neuroscience Applicants must have full GMC registration, a licence to practise and be eligible for inclusion in the GMC Specialist Register. -

Angus Health &SCIJB 9 Decmeber
AGENDA ITEM NO 10 REPORT NO IJB 84/20 ANGUS HEALTH AND SOCIAL CARE INTEGRATION JOINT BOARD – 9 DECEMBER 2020 COVID-19 UPDATE REPORT BY GAIL SMITH, INTERIM CHIEF OFFICER ABSTRACT This report provides an update to the IJB on the Angus Health and Social Care Partnership response to the COVID-19 pandemic, focusing on the activity undertaken and challenges faced since the last IJB on 28 October 2020 (Report No 64/20). 1. RECOMMENDATION (s) It is recommended that the Integration Joint Board: - (i) note the actions that have been advanced by the Angus Health and Social Care Partnership and key partners, in response to the COVID-19 pandemic, since the last COVID-19 update provided to the IJB on 28 October 2020. (ii) note and commends staff and key partners for their sustained effort and commitment as we continue to provide care to the people in Angus who rely on our care and support, despite a number of challenges. 2. BACKGROUND As COVID-19 restrictions eased over the summer months, this has been followed by an expected increase in the daily COVID-19 infection numbers, resulting in targeted lockdowns across the country to address infection clusters where they arise. Some of the key decisions made by the Scottish Government since the last update to the IJB include: • 2 November: The new five-tier system of COVID-19 restrictions was introduced in Scotland and will be reviewed each week by Scottish Parliament. Angus placed in Tier 2. • 13 November: Angus moved to Tier 3 COVID-19 restriction level due to the escalating numbers of positive cases of COVID-19.