FINAL DRAFT Tayside Mental Health and Wellbeing Strategy 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Putting Quality, Into Life
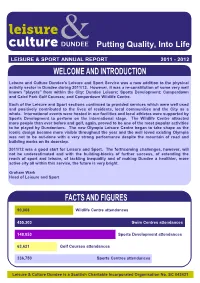
Putting Quality, Into Life LEISURE & SPORT ANNUAL REPORT 2011 - 2012 Leisure and Culture Dundee's Leisure and Sport Service was a new addition to the physical activity sector in Dundee during 2011/12. However, it was a re-constitution of some very well known "players" from within the City: Dundee Leisure; Sports Development; Camperdown and Caird Park Golf Courses; and Camperdown Wildlife Centre. Each of the Leisure and Sport sections continued to provided services which were well used and positively contributed to the lives of residents, local communities and the City as a whole. International events were hosted in our facilities and local athletes were supported by Sports Development to perform on the international stage. The Wildlife Centre attracted more people than ever before and golf, again, proved to be one of the most popular activities to be played by Dundonians. The new Olympia Leisure Centre began to take shape as the iconic design became more visible throughout the year and the well loved existing Olympia was not to be out-done with a very strong performance despite the mountain of road and building works on its doorstep. 2011/12 was a good start for Leisure and Sport. The forthcoming challenges, however, will not be underestimated and with the building-blocks of further success, of extending the reach of sport and leisure, of tackling inequality and of making Dundee a healthier, more active city all within this service, the future is very bright. Graham Wark Head of Leisure and Sport 90,068 Wildlife Centre attendances 455,303 Swim Centres attendances 148,053 Sports Development attendances 63,621 Golf Courses attendances 336,750 Sports Centres attendances Leisure & Culture Dundee is a Scottish Charitable Incorporated Organisation No. -

Spotlight Central and Tayside Residential Market Summer 2016
Savills World Research UK Residential Spotlight Central and Tayside Residential Market Summer 2016 Drumfada (Offers Over £540,000) in Dundee, where overall transactional activity increased annually by 13%. SUMMARY Growing confidence in lower price brackets fuels prime activity across Central and Tayside ■ The market below £400,000 across FIGURE 1 Central and Tayside has outperformed Residential values annual change forecast Scotland and continues to attract second home owners and downsizers Area 2016 2017 2018 2019 2020 from outside the region. Prime GB regional 2.5% 3.5% 6.0% 4.5% 4.0% ■ Strong growth across lower price bands is now leading to improved Prime Scotland 2.0% 3.5% 4.0% 4.0% 4.0% prime activity in the city and town locations of Angus, Dundee, Fife, Prime Central & Tayside 1.0% 2.5% 3.5% 3.5% 3.5% Stirling, and Perth. Mainstream UK 5.0% 3.0% 3.0% 2.5% 2.5% ■ The prime market has adjusted to Mainstream Scotland 3.0% 3.0% 2.5% 2.5% 2.5% taxation changes in the city hotspots of Edinburgh and Glasgow, with Mainstream Central & Tayside 2.5% 2.5% 2.0% 2.0% 2.0% growth spreading into traditional suburbs and commuter areas. Source: Savills Research savills.co.uk/research 01 Spotlight | Central and Tayside Residential Market CENTRAL AND to the city hubs of Edinburgh and Stirling city and the hotspots of Glasgow. As a consequence, there Dollar, Dunblane and Killearn. Tayside MARKET will be opportunities for buyers to take advantage of relative The Fife market was in line with affordability (Figure 1). -

Tayside, Angus and Perthshire Fibromyalgia Support Group Scotland
Tayside, Angus and Perthshire Angus Long Term Conditions Support Fibromyalgia Support Group Scotland Groups Offer help and support to people suffering from fibromyalgia. This help and support also extends to Have 4 groups of friendly people who meet monthly at family and friends of sufferers and people who various locations within Angus and offer support to people would like more information on fibromyalgia. who suffer from any form of Long Term Condition or for ANGUS Directory They meet every first Saturday of every month at carers of someone with a Long Term Condition as well as Ninewells Hospital, Dundee. These meetings are each other, light refreshments are provided. to Local held on Level 7, Promenade Area starting at 11am For more information visit www.altcsg.org.uk or e-mail: Self Help Groups and finish at 1pm. [email protected] For more information contact TAP FM Support Group, PO Box 10183, Dundee DD4 8WT, visit www.tapfm.co.uk or e-mail - [email protected] . Multiple Sclerosis Society Angus Branch For information about, or assistance about the Angus Gatepost Branch please call 0845 900 57 60 between 9am - 8pm or e-mail Brian Robson at mailto:[email protected] GATEPOST is run by Scottish farming charity RSABI and offers a helpline service to anyone who works on the land in Scotland, and also their families. Myalgic Encephalomyelitis/Chronic They offer a friendly, listening ear and a sounding post for Fatigue Syndrome (ME/CFS) you at difficult times, whatever the reason. If you’re The aims of the support group are to give support to worried, stressed, or feeling isolated, they can help. -

BMA Scotland – Guide to Information Available Through the Model Publication Scheme for GP Practices
BMA Scotland – Guide to information available through the model publication scheme for GP practices BMA Scotland – Guide to information available through the model publication scheme for GP practices Carnoustie Medical Group Guide to information available through the Scottish Information Commissioner’s Model Publication Scheme This guide was last updated on 24 July 2019 BMA Scotland – Guide to information available through the model publication scheme for GP practices Index Section 1 Introduction Section 2 About Carnoustie Medical Group Section 3 Our functions and services Section 4 How we take decisions and what we have decided Section 5 What we spend and how we spend it Section 6 Accessing information under the scheme Section 7 Information that we may withhold Section 8 Our charging policy Section 9 Our copyright policy Section 10 Our records management and disposal policy Section 11 Feedback Section 12 Complaints Section 13 How to access information which is not available under this scheme Section 14 Classes of information BMA Scotland – Guide to information available through the model publication scheme for GP practices Section 1: Introduction The Freedom of Information (Scotland) Act 2002 requires Scottish public authorities to produce and maintain a publication scheme. Authorities are under a legal obligation to: Publish the classes of information they make routinely available Tell the public how to access the information and what it might cost Carnoustie Medical Group has adopted the Model Publication Scheme produced by the Scottish Information Commissioner. The scheme will be reviewed from time to time and updated in line with guidance from the Scottish Information Commissioner. You can see the model publication scheme on the Commissioner’s website at www.itspublicknowledge.info/mps or by contacting us at the address provided below. -

Tayside November 2014
Regional Skills Assessment Tayside November 2014 Angus Perth and Kinross Dundee City Acknowledgement The Regional Skills Assessment Steering Group (Skills Development Scotland, Scottish Enterprise, the Scottish Funding Council and the Scottish Local Authorities Economic Development Group) would like to thank SQW for their highly professional support in the analysis and collation of the data that forms the basis of this Regional Skills Assessment. Regional Skills Assessment Tayside Contents 1 Introduction 2 2 Context 5 3 Economic Performance 7 4 Profile of the Workforce 20 5 People and Skills Supply 29 6 Education and Training Provision 43 7 Skills Mismatches 63 8 Economic and Skills Outlook 73 9 Questions Arising 80 sds.co.uk 1 Regional Skills Assessment Section 1 Tayside Introduction 1 Introduction 1.1 The purpose of Regional Skills Assessments This document is one of a series of Regional Skills Assessments (RSAs), which have been produced to provide a high quality and consistent source of evidence about economic and skills performance and delivery at a regional level. The RSAs are intended as a resource that can be used to identify regional strengths and any issues or mismatches arising, and so inform thinking about future planning and investment at a regional level. 1.2 The development and coverage of RSAs The content and geographical coverage of the RSAs was decided by a steering group comprising Skills Development Scotland, Scottish Enterprise, the Scottish Funding Council and extended to include the Scottish Local Authorities Economic Development Group during the development process. It was influenced by a series of discussions with local authorities and colleges, primarily about the most appropriate geographic breakdown. -

NHS Tayside CONSULTANT PSYCHIATRIST
NHS Tayside CONSULTANT PSYCHIATRIST General Adult Psychiatry VACANCY Consultant in General Adult Psychiatry (x2 posts) Wedderburn House / Carseview Centre: Dundee Community Mental Health Team 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent NHS Tayside is looking for committed, innovative and enthusiastic Consultant Psychiatrists (full or part time) to join our Community Mental Health Team based in Dundee the ‘City of Discovery’. These posts include opportunities to see and treat a wide variety of psychiatric disorders in patients aged from eighteen to sixty-five years old, with the support of our enthusiastic and well staffed multi-disciplinary and multi- agency social work and health Community Mental Health Team with access to our 20 bed inpatient unit. We have local drug and alcohol, forensic, eating disorder, liaison and advanced intervention services as well as psychotherapy and psychology services available for our patients, and enjoy excellent relations with our local General Practitioners and voluntary service colleagues. There are many learning and training opportunities, including the teaching and supervision of 4th year medical students and Specialty Trainees attached to our team. There is a monthly continuing professional development programme and other continuing professional development will also be encouraged. Active involvement in service improvement is available through membership of our Service Improvement Group. We have close links with the University of Dundee division of Neuroscience where academic and research opportunities are available: http://medicine.dundee.ac.uk/medical-research-institute/divisions/division- neuroscience. Dundee is a coastal city on the Firth of Tay estuary in eastern Scotland. Its regenerated waterfront has the new Victoria and Albert Museum which stands on the banks of the Tay and two nautical museums: RRS Discovery, Captain Scott’s Antarctic expedition ship, and 19th-century warship, HM Frigate Unicorn. -

TAYSIDE VALUATION APPEAL PANEL LIST of APPEALS for CONSIDERATION by the VALUATION APPEAL COMMITTEE at Robertson House, Whitefriars Crescent, PERTH on 24 June 2021
TAYSIDE VALUATION APPEAL PANEL LIST OF APPEALS FOR CONSIDERATION BY THE VALUATION APPEAL COMMITTEE At Robertson House, Whitefriars Crescent, PERTH on 24 June 2021 Assessor's Appellant's Case No Details & Contact Description & Situation Appellant NAV RV NAV RV Remarks 001 08SKB2786000 SORTING OFFICE ROYAL MAIL GROUP LIMITED £11,900 £11,900 757371 0002 87-93 HIGH STREET 100 VICTORIA EMBANKMENT Update 2019 KINROSS LONDON 31 March 2020 KY13 8AA EC4Y 0HQ 002 12PTR0127000 WAREHOUSE DMS PARTNERS LTD £35,100 £35,100 £17,550 £17,550 719396 0005 UNIT 1A PER ANDREW REILLY ASSOC. LTD Update 2020 ARRAN ROAD 31 RUTLAND SQUARE 12 June 2020 PERTH EDINBURGH PH1 3DZ EH1 2BW 003 12PTR0127125 WAREHOUSE DMS PARTNERS LTD £17,200 £17,200 £8,600 £8,600 524162 0002 UNIT 1B PER ANDREW REILLY ASSOC. LTD Update 2020 ARRAN ROAD 31 RUTLAND SQUARE 12 June 2020 PERTH EDINBURGH PH1 3DZ EH1 2BW 004 12PTR0095000 WAREHOUSE & OFFICE REMBRAND TIMBER LTD £36,900 £36,900 £18,450 £18,450 772904 0003 ARRAN ROAD PER ANDREW REILLY ASSOC. LTD Update 2020 PERTH 31 RUTLAND SQUARE 19 June 2020 PH1 3DZ EDINBURGH EH1 2BW 005 12PTR0127250 WAREHOUSE BELLA & DUKE LTD £30,100 £30,100 522012 0002 UNIT 2 PER ANDREW REILLY ASSOCIATES LTD Update 2020 ARRAN ROAD 31 RUTLAND SQUARE 23 June 2020 PERTH EDINBURGH PH1 3DZ EH1 2BW 006 09SUC0144000 YARD SUEZ RECYCLING & RECOVERY UK LTD £49,800 £49,800 766760 0002 WOOD CHIP PROCESSING PLANT PER AVISON YOUNG Update 2019 BINN HILL 1ST FLOOR, SUTHERLAND HOUSE 29 March 2020 GLENFARG 149 ST VINCENT STREET PERTH GLASGOW PH2 9PX G2 5NW Page 1 Assessor's Appellant's -

Stewart2019.Pdf
Political Change and Scottish Nationalism in Dundee 1973-2012 Thomas A W Stewart PhD Thesis University of Edinburgh 2019 Abstract Prior to the 2014 independence referendum, the Scottish National Party’s strongest bastions of support were in rural areas. The sole exception was Dundee, where it has consistently enjoyed levels of support well ahead of the national average, first replacing the Conservatives as the city’s second party in the 1970s before overcoming Labour to become its leading force in the 2000s. Through this period it achieved Westminster representation between 1974 and 1987, and again since 2005, and had won both of its Scottish Parliamentary seats by 2007. This performance has been completely unmatched in any of the country’s other cities. Using a mixture of archival research, oral history interviews, the local press and memoires, this thesis seeks to explain the party’s record of success in Dundee. It will assess the extent to which the character of the city itself, its economy, demography, geography, history, and local media landscape, made Dundee especially prone to Nationalist politics. It will then address the more fundamental importance of the interaction of local political forces that were independent of the city’s nature through an examination of the ability of party machines, key individuals and political strategies to shape the city’s electoral landscape. The local SNP and its main rival throughout the period, the Labour Party, will be analysed in particular detail. The thesis will also take time to delve into the histories of the Conservatives, Liberals and Radical Left within the city and their influence on the fortunes of the SNP. -

Assessment of Landscape Sensitivity to Wind Turbine Development in Highland
Assessment of Landscape Sensitivity to Wind Turbine Development in Highland D.R. Miller, S. Bell, M. McKeen, P.L. Horne, J.G. Morrice and D. Donnelly Summary Report Macaulay Land Use Research Institute September 2010 TABLE OF CONTENTS LIST OF FIGURES .................................................................................................................................II ACKNOWLEDGEMENTS.......................................................................................................................II 1 INTRODUCTION.............................................................................................................................1 1.1 OBJECTIVES..........................................................................................................................1 1.2 DEFINITION OF KEY TERMS.................................................................................................2 1.3 LIMITATIONS..........................................................................................................................3 2 METHODOLOGY............................................................................................................................4 2.1 BACKGROUND.......................................................................................................................4 2.2 LANDSCAPE CHARACTER ASSESSMENT..........................................................................5 2.3 LANDSCAPE CHARACTER SENSITIVITY ............................................................................6 -

National System for Sexual Health (Nash)
National System for Sexual Health (NaSH) Protecting your Personal Information How do you protect my personal information? NHS Scotland cares about your personal data and it’s important that you know how we use it and keep it safe. We use a computer system, just for sexual health clinics in Scotland, called ‘NaSH’. You may be asked to complete a registration form so we can create an electronic record using your personal details. Some people will register directly through our on-line booking site. We prefer to download your name and address details electronically, using your NHS Scotland number (CHI number), as this saves time and reduces errors. The registration form will record your permission to use CHI. You can also choose to use an assumed (‘made-up’) name and not use your CHI number but please be aware that we would not be able to refer you for any x-ray investigations or communicate with your GP or other health professional under an assumed name. You will be given a sexual health clinic number called a ‘NaSH number’ which starts with ‘AN’ (e.g. AN012345678). Please keep this number safe as it may be required to access your test results. You can use this number to access care in any specialist sexual health clinic in NHS Scotland. We are committed to protecting your privacy and will only process personal confidential data in accordance with the Data Protection Act 2018. Who can access the NaSH system and my personal information? The NaSH system can only be accessed by staff working under the oversight of specialist sexual health and HIV services in Scotland who have a legal duty to keep information about you confidential. -

Foi202000130010
The First Minister’s 2019 Christmas Card Project will benefit the following charities: Marine Conservation Society Glasgow & Clyde Rape Crisis Friends of Victoria & Whyteman’s Brae Hospitals Celebrated and named as one of the 100 Greatest Singers of All Time by Rolling Stone Magazine, Annie Lennox’s iconic musical career spans over four decades. Her collaboration with partner Dave Stewart formed Eurythmics in the early ‘80s. Lennox has also enjoyed a widely acclaimed solo career, selling over 83 million albums worldwide altogether. In 2012, Annie Lennox was awarded the Order of the British Empire for her work towards the eradication of AIDS and poverty in Africa. She is a Royal Academician, a respected social activist and philanthropist, and the first female Chancellor of Glasgow Caledonian University. Her work in the visual arts has included an exhibition at the Victoria and Albert Museum, London; ‘The House of Annie Lennox’ which travelled to Manchester, Aberdeen; and The National Portrait Gallery of Edinburgh. Her installation ‘Now I Let You Go’… is currently exhibited at Massachusetts Museum of Contemporary Art. Annie has been awarded the Royal Scottish Geographical Society’s ‘Livingstone Medal’ and, in 2017, her philanthropic work was honoured with the George Harrison Global Citizen Award, and a second prestigious German Sustainability Award. Merry Christmas and a Happy New Year Nollaig Chridheil agus Bliadhna Mhath Ùr Season’s Greetings Beannachdan aig àm na Nollaige The Rt Hon Nicola Sturgeon MSP and Mr Peter Murrell Bute ButeHouse, -

NHS Guidlines
NHSScotland Identity guidelines Identikit Introduction In December 2000, Susan Deacon MSP, In this publication, the Minister said: “The public relate to and recognise Minister for Health and Community Care, the NHS. They believe their care is launched ‘Our National Health: provided by a national health service and staff take pride in the fact that a plan for action, a plan for change’ they work for the NHS. Research tells us that the variety of differently which set out a clear direction for the NHS named NHS bodies confuses the in Scotland with the aims of improving public and alienates staff. As part of our proposals to rebuild the National people’s health and creating a 21st century Health Service we will promote a new identity for the NHS in Scotland.” health service. The guidelines that follow provide an essential design toolkit to establish “Alongside the changes in NHS this new identity. The guidelines cover signage, vehicles, uniforms, stationery, boardrooms, we will re-establish literature, forms and other items. The a national identity for the aim is to replace, over time, the array of existing identities within NHS NHS in Scotland.” organisations with the single NHS identity while avoiding wastage and unnecessary expenditure. Our National Health: a plan for action, a plan for change section 3/page 31 2 Contents Section 1 Our national identity 4 Exclusion zone 6 Minimum size 6 Section 2 Identity structure 7 Essential elements 9 Identity variants 10 Caring device 12 Positioning the identity 14 Other identities 15 Working in partnership 16 Section 3 Identities for ideas & initiatives 17 Initiatives 18 Section 4 NHSScotland typefaces 19 Stone Sans 20 Arial 24 Garamond 25 Times New Roman 26 Literature 27 Section 5 Colour 28 Using colour 29 Primary colours 30 Colour palette 31 Tints 32 Printing the identity 33 3 Section One Our national identity Together, the initials ‘NHS’ and the caring symbol form the foundations of our identity.