Systematic Review and Meta-Analysis for Prevention of Cardiovascular
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Semaglutide Versus Liraglutide for Treatment of Obesity
Archives of Diabetes & Obesity DOI: 10.32474/ADO.2021.03.000162 ISSN: 2638-5910 Review Article Semaglutide versus liraglutide for treatment of obesity Nasser Mikhail* *Department of Medicine, Endocrinology Division, David-Geffen UCLA Medical School, USA *Corresponding author: Nasser Mikhail, Endocrinology Division, Department of Medicine, Olive View-UCLA Medical Center, David- Geffen UCLA Medical School, CA, USA Received: April 02, 2021 Published: April 19, 2021 Abstract Background: Once weekly (OW) semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) currently under evaluation for treatment of obesity at a dose of 2.4 mg OW. Objective Methods : To compare weight-loss efficacy and safety of once daily (OD) liraglutide 3.0 mg versus OW semaglutide 2.4 mg. : Pubmed research up to March 31, 2021. Randomized trials, pertinent animal studies, and reviews are included. Search Results terms were glucagon-like peptide-1 receptor agonists, weight loss, obesity, liraglutide, semaglutide, efficacy, safety. semaglutide 2.4 mg. However, marked resemblance between trials in terms of study protocols and subjects’ characteristics may allow indirect: No comparison. head to head In clinical trials are trials available of OW tosemaglutide, provide direct this comparison drug was consistently of efficacy ofassociated OD liraglutide with greater 3.0 mg weightversus lossOW than in trials of OD liraglutide. Thus, placebo-corrected percentage weight reduction was -10.3 to -12.4% and -5.4% with OW semaglutide and OD liraglutide, respectively. In patients with type 2 diabetes, corresponding weight reduction was less pronounced with both drugs being -6.2% and -4.3% with OW semaglutide and OD liraglutide, respectively. -

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

A 26-Week Randomized Controlled Trial of Semaglutide Once Daily Versus Liraglutide and Placebo in Patients with Type 2 Diabetes
1926 Diabetes Care Volume 41, September 2018 Ildiko Lingvay,1 Cyrus V. Desouza,2 A 26-Week Randomized Katarina S. Lalic,3 Ludger Rose,4 Thomas Hansen,5 Jeppe Zacho,5 and Controlled Trial of Semaglutide Thomas R. Pieber6 EMERGING THERAPIES: DRUGS AND REGIMENS Once Daily Versus Liraglutide and Placebo in Patients With Type 2 Diabetes Suboptimally Controlled on Diet and Exercise With or Without Metformin Diabetes Care 2018;41:1926–1937 | https://doi.org/10.2337/dc17-2381 OBJECTIVE To investigate the efficacy and safety of once-daily semaglutide in comparison with once-daily liraglutide and placebo in patients with type 2 diabetes. RESEARCH DESIGN AND METHODS This 26-week, multicenter, double-blind trial involved patients diagnosed with 1University of Texas Southwestern Medical Cen- type 2 diabetes with HbA1c 7.0–10.0% (53–86 mmol/mol) and treated with diet ter at Dallas, Dallas, TX and exercise with or without metformin. Patients were randomized 2:2:1 to once- 2University of Nebraska Medical Center, Omaha, daily semaglutide, liraglutide, or placebo in one of four volume-matched doses NE 3Faculty of Medicine, University of Belgrade, and (semaglutide 0.05, 0.1, 0.2, or 0.3 mg and liraglutide 0.3, 0.6, 1.2, or 1.8 mg, with Clinic for Endocrinology, Diabetes and Metabolic both compared within each volume-matched dose group). Primary end point was Diseases, Clinical Center of Serbia, Belgrade, Serbia change in HbA1c from baseline to week 26. 4Institute for Diabetes Research in Munster,¨ RESULTS Munster,¨ Germany 5Novo Nordisk A/S, Søborg, Denmark In total, 705 randomized patients were exposed to trial products. -

OZEMPIC (Semaglutide) Injection, for Subcutaneous Use Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙CONTRAINDICATIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ These highlights do not include all the information needed to use Personal or family history of medullary thyroid carcinoma or in patients OZEMPIC® safely and effectively. See full prescribing information with Multiple Endocrine Neoplasia syndrome type 2 (4). for OZEMPIC. Known hypersensitivity to OZEMPIC or any of the product components (4). OZEMPIC (semaglutide) injection, for subcutaneous use Initial U.S. Approval: 2017 ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙WARNINGS AND PRECAUTIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ Pancreatitis: Has been reported in clinical trials. Discontinue promptly if WARNING: RISK OF THYROID C-CELL TUMORS pancreatitis is suspected. Do not restart if pancreatitis is confirmed (5.2). See full prescribing information for complete boxed warning. Diabetic Retinopathy Complications: Has been reported in a clinical trial. Patients with a history of diabetic retinopathy should be monitored (5.3). In rodents, semaglutide causes thyroid C-cell tumors. It is Never share an OZEMPIC pen between patients, even if the needle is unknown whether OZEMPIC causes thyroid C-cell tumors, changed (5.4). including medullary thyroid carcinoma (MTC), in humans as Hypoglycemia: When OZEMPIC is used with an insulin secretagogue or the human relevance of semaglutide-induced rodent thyroid C- insulin, consider lowering the dose of the secretagogue or insulin to reduce cell tumors has not been determined (5.1, 13.1). the risk of hypoglycemia (5.5). OZEMPIC is contraindicated in patients with a personal or Acute Kidney Injury: Monitor renal function in patients with renal family history of MTC or in patients with Multiple Endocrine impairment reporting severe adverse gastrointestinal reactions (5.6). Neoplasia syndrome type 2 (MEN 2). -

Subcutaneous Semaglutide, Dulaglutide and Liraglutide 1.2Mg for the Treatment of Type
North Central London Joint Formulary Committee Factsheet Subcutaneous SEMAGLUTIDE▼ (Ozempic®), DULAGLUTIDE▼ (Trulicity®) and LIRAGLUTIDE 1.2mg (Victoza®) Treatment of Type 2 Diabetes Mellitus Start date: December 2019 Review date: August 2022 Document Control Date Version Action July 2016 1.0 New guideline August 2019 1.1 Subcutaneous semaglutide added as the preferred GLP-1 receptor agonist November 2019 1.2 Supply quantities added Agreed by NCL Shared Care Group: December 2019 FACTSHEET TO FACILITATE PRESCRIBING PLEASE NOTE THIS IS NOT A SHARED CARE GUIDELINE, NOR IS IT A FULL SUMMARY OF DRUG INFORMATION. ALWAYS REFER TO THE MOST RECENT BNF AND/OR SUMMARY OF PRODUCT CHARACTERISTICS. Disclaimer This Fact Sheet is registered at North Central London (NCL) Joint Formulary Committee (JFC) and is intended solely for use by healthcare professionals to aid the treatment of patients within NCL. However, this fact sheet is for guidance only, its interpretation and application remains the responsibility of the individual clinician. If in doubt, contact a senior colleague or expert. Clinicians are advised to refer to the manufacturer’s current prescribing information before treating individual patients. The authors and NCL JFC accept no liability for use of this information from this beyond its intended use. While we have tried to compile accurate information in this document, and to keep it updated in a timely manner, we cannot guarantee that it is fully complete and correct at all times. If you identify information within this document that is inaccurate, please report this to the [email protected]. If a patient is harmed as a consequence of following this document, please complete a local incident report and inform [email protected]. -

125469Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125469Orig1s000 SUMMARY REVIEW Division Director Review 1. Introduction On September 18, 2013 Eli Lilly and Company submitted a Biologics License Application (BLA) for Trulicity under section 351 of the Public Health Service Act. The applicant is seeking to indicate Trulicity as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Trulicity is a solution for injection containing either 0.75 or 1.5 mg of dulaglutide [i.e., a glucagon-like peptide 1 (GLP-1) receptor agonist]. Trulicity is to be administered by subcutaneous injection at once weekly intervals. Once approved, Trulicity will be the fifth GLP-1 agonist indicated for use in the management of patients with type 2 diabetes mellitus in the United States. This document serves as the division director’s memorandum for the application. 2. Background The drug substance in Trulicity is dulaglutide. In this memorandum, I will use Trulicity and dulaglutide interchangeably. Dulaglutide is a homodimer that consists of two identical polypeptide chains linked to each other by a disulfide bond. The polypeptide chain is a fusion protein that consists of a glucagon-like peptide 1 (GLP-1) variant, a linker, and the Fc portion of a human IgG4 variant antibody. The GLP-1 analog portion of dulaglutide is (b) (4) homologous to native human GLP-1 (7-37) (b) (4) (b) (4) Dulaglutide was demonstrated to bind and activate the GLP-1 receptor. The biological effects of endogenous GLP-1 on glucose homeostasis include augmentation of glucose stimulated insulin secretion, inhibition of glucagon release, and delay of gastric emptying. -
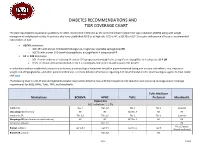
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -
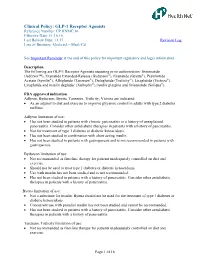
GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal
Clinical Policy: GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are GLP-1 Receptor Agonists requiring prior authorization: lixisenatide (Adlyxin™), Exenatide Extended-Release (Bydureon®), Exenatide (Byetta®), Pramlintide Acetate (Symlin®), Albiglutide (Tanzeum®), Dulaglutide (Trulicity®), Liraglutide (Victoza®), Liraglutide and insulin degludec (Xultophy®),Insulin glargine and lixisenatide (Soliqua®). FDA approved indication Adlyxin, Bydureon, Byetta, Tanzeum, Trulicity, Victoza are indicated: As an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Adlyxin limitation of use: Has not been studied in patients with chronic pancreatitis or a history of unexplained pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Not for treatment of type 1 diabetes or diabetic ketoacidosis. Has not been studied in combination with short acting insulin. Has not been studied in patients with gastroparesis and is not recommended in patients with gastroparesis. Bydureon limitation of use: Not recommended as first-line therapy for patients inadequately controlled on diet and exercise. Should not be used to treat type 1 diabetes or diabetic ketoacidosis. Use with insulin has not been studied and is not recommended. Has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Byetta limitation of use: Not a substitute for insulin. Byetta should not be used for the treatment of type 1 diabetes or diabetic ketoacidosis. -

New Drug Update
7/1/2014 New Drug Update LaKeisha Williams, PharmD, MSPH Drug Information Specialist Xavier University of Louisiana College of Pharmacy LPA Annual Convention –July 18, 2014 Speaker Disclosures • The speaker declares no conflicts of interest, real or apparent, and no financial interests in any company, product, or service mentioned in this program. 1 7/1/2014 Learning Objectives • At the completion of this activity, PHARMACISTS will be able to: – Recognize the clinical indications for selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Explain the mechanisms of action for new therapeutic agents discussed. – Identify common adverse reactions, relevant drug interactions and key contraindications for the new approved therapeutic agents. – Discuss pertinent patient education for newly approved agents. Learning Objectives • At the completion of this activity, PHARMACY TECHNICIANS will be able to: – Describe selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Recognize the indications of selected new therapeutic agents. – Summarize adverse reactions and precautions when evaluating FDA approved agents. – List counseling tips for newly approved therapeutic agents. 2 7/1/2014 New Drug Approvals of 2013 • Food and Drug Administration (FDA) approved 27 new molecular entities (NMEs) – More than a third (36%) of novel drugs approved are for rare diseases – Nearly one out of three (32%) are the first in their class – Approximately three‐quarters (72%) of novel drugs were first approved in the U.S. Jenkins J. U.S. Food and Drug Administration/FY 2013 New Drug Review. www.fda.gov New Drug Approvals of 2014 • Food and Drug Administration (FDA) approved 16 new molecular entities (NMEs) – Innovative new products that never before have been used in clinical practice – Many contain active moieties that have not been approved by FDA previously, either as a single ingredient drug or as part of a combination product Food and Drug Administration. -

Weekly Semaglutide Vs. Liraglutide Efficacy Profile: a Network Meta
healthcare Systematic Review Weekly Semaglutide vs. Liraglutide Efficacy Profile: A Network Meta-Analysis Hassan A. Alsugair 1,* , Ibrahim F. Alshugair 2 , Turki J. Alharbi 1,*, Abdulaziz M. Bin Rsheed 1 , Ayla M. Tourkmani 1 and Wedad Al-Madani 3 1 Family Medicine Department, Prince Sultan Military Medical City, Riyadh 12624, Saudi Arabia; [email protected] (A.M.B.R.); [email protected] (A.M.T.) 2 Orthopedic Surgery Department, King Saud Medical City, Riyadh 12746, Saudi Arabia; [email protected] 3 General Authority of Statistics, Riyadh 11481, Saudi Arabia; [email protected] * Correspondence: [email protected] or [email protected] (H.A.A.); [email protected] or [email protected] (T.J.A.); Tel.: +966-114777714-40438 (T.J.A.) Abstract: Introduction: Glucagon-like peptide 1 receptor agonist (GLP-1 RA) is a class of hypo- glycemic medications. Semaglutide once-weekly (QW) and liraglutide once-daily (OD) significantly improved glycemic control compared to placebo. To date, no long-term phase III trials directly comparing semaglutide and liraglutide are available. This network meta-analysis (NMA) aims to compare the long-term efficacy of semaglutide and liraglutide. Methods: PubMed, Embase, and Cochrane Library were searched from inception until June 2019 to identify relevant articles. Nine long-term randomized controlled trials comparing once-weekly semaglutide or liraglutide with placebo or other active comparisons were identified. The outcomes of interest were changes in HbA1c and weight after 52 weeks. A Bayesian framework and NMA were used for data synthesis. Citation: Alsugair, H.A.; This is a sub-study of the protocol registered in PROSPERO (number CRD42018091598). -

Prior Authorization Protocol NATL
Prior Authorization Protocol BYDUREON™ (exenatide extended-release for injectable suspension), BYETTA TM (exenatide), SYMLIN PEN (pramlintide acetate), TANZEUM TM (albiglutide) TRULICITY™ (dulaglutide), VICTOZA ® (liraglutide) NATL Coverage of drugs is first determined by the member`s pharmacy or medical benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: • Bydureon, Byetta, Tanzeum, Trulicity, Victoza: An adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus • Symlin: Adjunctive treatment in patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose control despite optimal insulin therapy. II. Health Net Approved Indications and Usage Guidelines: Bydureon/ Byetta/Tanzeum/Trulicity/Victoza: • Diagnosis of type 2 diabetes AND • Documentation of baseline A1C AND • Failure or clinically significant adverse effects to at least a 3 month trial of metformin (unless contraindicated) REAUTHORIZATION REQUESTS: If inadequate response to GLP-1 receptor agonist ( i.e. <0.5% reduction in A1c) at the end of initial authorization period, either a switch to insulin therapy, addition of insulin(s) to Victoza or a referral to an endocrinologist will be required. Reauthorization requests require documentation of continued metformin therapy (unless contraindicated). Symlin: • Diagnosis of Diabetes Mellitus Type 1 or 2 AND • Failure to achieve desired blood glucose level despite 3 months of three or more daily mealtime insulin (e.g. Humalog ®, Humulin ® R) injections or use of an insulin pump Confidential & Proprietary Page 1 Draft Prepared: 06.17.05 JP Approved by Health Net Pharmacy & Therapeutics Committee: 11.16.05, 04.06, 5.21.08, 11.19.08, 11.19.09, 8.25.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 04.07.06. -

Management of Type 2 Diabetes Mellitus Dr Naomi Achong Endocrinologist MBBS(Hons) Bsc FRACP Phd Overview
Management of Type 2 Diabetes Mellitus Dr Naomi Achong Endocrinologist MBBS(Hons) BSc FRACP PhD Overview • Overview of T2DM & glycaemic targets • Treatment after metformin – newer agents on the market • SGLT2 inhibitors • DPP4 agonists • GLP1 antagonists • Insulin options • Newer options – coformulation Diagnosis • ADS position statement • Criteria: • HbA1c > 6.5% • Fasting glucose > 7mmol/L. • Random glucose > 11.1mmol/L • GTT showing fasting > 7 or 2hr > 11.1mmol/L • Patients with IGT have an increased risk of death and vascular disease (regardless of progression to diabetes) as well as microvascular complications • Risk of progression to T2DM is reduced by 58% with lifestyle modification and 31% with metformin 1.The DECODE Study. Arch Intern Med 2001; 161:397-405 2. Singleton JR et al. Diabetes 2003;52(12):2867-2873 3. Diabetes Prevention Program Research Group. N Engl J Med 2002; 346:393-403 Optimising health outcomes in diabetes • Glucose control • Smoking cessation • Blood pressure control • Lipid management with priority to statins • Some circumstances, antiplatelet therapy ADA/EASD – 2015 position statement • Glycaemic targets need to be individualised • Based on modifiable and non-modifiable factors 1. Inzucchi S.E., Bergenstal R.M., Buse J.B., Diamant M., Ferrannini E., Nauck M. et al Diabetologia. 2015; 58: 429-442 1. Inzucchi S.E. et al. Diabetologia. 2015; 58: 429-442 Importance of glycaemic control GOOD GLYCAEMIC CONTROL Reduces diabetes-related complications Reduces total diabetes-related costs UKPDS1 Retrospective database analysis2 1% mean HbA1c reduction results in: HbA1c ≤7% continuously for 1 year results in . 37% 14% 21% 25% Which included: Myocardial 22% lower diabetes infarction medical costs Diabetes-related 28% lower diabetes mortality Diabetes-related pharmacy costs treatment costs Microvascular complications .