Convergence for Improvedplan of Action
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FULL SECTOR ASSESSMENT: WATER and OTHER URBAN INFRASTRUCTURE and SERVICES A. India Urban Scenario 1. About 377 Million (31%)1 Of
Madhya Pradesh Urban Sector Investment Program (RRP IND 42486) FULL SECTOR ASSESSMENT: WATER AND OTHER URBAN INFRASTRUCTURE AND SERVICES A. India Urban Scenario 1. About 377 million (31%)1 of India’s population lives in 7,935 urban areas and contributes 63% of gross domestic product (GDP). About 70% of the urban population resides in 4682 rapidly growing urban agglomerations and cities with a population of over 100,000, including 53 cities with a population of more than a million. Growth in the remaining small towns was nominal. The contribution to GDP from the urban areas is expected to increase to about 75% as the proportion of urban population reaches 40% of the total population by 2030. 2. Urban water supply in India is characterized by intermittent water supply (often for a couple of hours in a week) and low coverage, high nonrevenue water, and poor cost recovery. No city in India can claim for universal coverage with continuous pressurized water supply. The service levels are even lower in small towns, which have been upgraded from village character to a town. These small towns mostly depend on local groundwater sources with no treatment and no planned hydraulic networks. The small town local bodies have been struggling with limited financial resources further aggravated by a lack of competent and skilled human resources capable of delivering services expected from a fully functional water utility. 3. The investment in urban infrastructure3 up to the year 2031 was estimated at $53.5 billion for water supply and $40.5 billion for sewerage services at 2009–10 prices. -

O.I.H. Government of India Ministry of Housing & Urban Affairs Lok Sabha Unstarred Question No. 2803 to Be Answered on March
O.I.H. GOVERNMENT OF INDIA MINISTRY OF HOUSING & URBAN AFFAIRS LOK SABHA UNSTARRED QUESTION NO. 2803 TO BE ANSWERED ON MARCH 13, 2018 DEVELOPMENT OF CITIES No.2803 SHRI LAXMI NARAYAN YADAV: Will the Minister of HOUSING AND URBAN AFFAIRS be pleased to state: (a) the proposals for the development of cities forwarded by the State Government of Madhya Pradesh to the Union Government during the last three years; (b) the names of the cities and the nature of work to which the said schemes are related to; and (c) the action taken so far by the Union Government on the said proposals along with the final outcome thereof? ANSWER THE MINISTER OF STATE ((INDEPENDENT CHARGE) OF THE MINISTRY OF HOUSING & URBAN AFFAIRS (SHRI HARDEEP SINGH PURI) (a) to (c) Urban Development is a State subject. The Ministry of Housing and Urban Affairs facilitates and assists States/Union Territories (UTs), including Madhya Pradesh, in this endeavour through its various Missions- Swachh Bharat Mission (SBM), Atal Mission for Rejuvenation and Urban Transformation (AMRUT), Smart Cities Mission (SCM), Pradhan Mantri Awas Yogana(Urban)(PMAY-U) and through Metro Rail Projects to improve urban infrastructure to improve the quality of life in cities and towns covered under these Mission. List of such cities/towns in the State of Madhya Pradesh along with details of funds released are in Annexure. Under the Missions the Central Government approves the State Plans and provides the Central Assistance to the States. The projects are designed, approved and executed by the States/UTs and the Cities. Annexure Annexure referred to in reply to part (a) to (c) of Lok Sabha Unstarred Question No 2803 regarding ‘Development of Cities’ for answer on 13 March,2018 Atal Mission for Rejuvenation and Urban Transformation(AMRUT) Cities covered under AMRUT Sl.No. -

Industrial Land Bank 2016
22 - 23 2016 22 - 23 2016 INDUSTRIAL LAND BANK 2016 22 - 23 2016 INDUSTRIAL LAND BANK 2016 22 - 23 2016 22 - 23 2016 Publisher: MP Trade and Investment Facilitation Corporation Limited “CEDMAP BHAWAN” 16-A, Arera Hills Bhopal - 462001, M.P(India) Tel. :(91) 755-2575618, 2571830 Fax : (91) 755-2559973 E-mail : [email protected] http://www.mptrifac.gov.in http://www.invest.mp.gov.in/ INDUSTRIAL LAND BANK 2016 CONTENT 1. Preface 2 2. Introduction 3 3. Industrial land bank available with Government of Madhya Pradesh 5 4. Industrial land bank with Audyogik Kendra Vikas Nigam (AKVN) 6 4a. Developed/Developing land bank available with AKVNs 9 • Bhopal AKVN 9 • IIDC Gwalior 22 • Indore AKVN 36 • Jabalpur AKVN 70 • Rewa AKVN 81 • Sagar AKVN 89 • Ujjain AKVN 99 4b. Undeveloped land bank available with AKVNs 113 4c. Undeveloped land allotment guidelines 131 5. Developed Industrial land bank with department of Micro Small and Medium Enterprises (MSME) 137 6. Industrial land bank available with Madhya Pradesh State Electronic Development Corporation (MPSEDC) 143 1 INDUSTRIAL LAND BANK 2016 1 2 INDUSTRIAL LAND BANK 2016 2 INTRODUCTION Madhya Pradesh has emerged as a Growth Centre of the country in the last decade. Madhya Pradesh has witnessed a radical transformation in terms of economic and social development. Madhya Pradesh’s central location makes it an ideal destination as a manufacturing and sourcing hub to tap the constantly growing Indian market. Owing to its rich soil, several rivers and large irrigation projects, Madhya Pradesh is a thriving destination for agriculture and food processing business. -

LIST of MINING PROJECTS - MPSEAC PENDING S.No
LIST OF MINING PROJECTS - MPSEAC PENDING S.No. Case No Category Name of Project Proponent Activity 1 59/2008 1(a) Agrawal Mineral process, Manganese ore mine 5.00 ha. Gwari-wadhana, 1(a) NagpurRoad , Chhindwara M.P. Teh-Sausar, Distt-Chhindwara M.P. 2 70/20081 1(a) M/s Ismail & Sons MissionChowk, Lime stone mine 10-748 ha. Village Bhatgaon (a) Katni M.P. Sunehra Teh-Murwada Katni M.P. 3 99/2008 1(a) M/s Nirmala Minerals Dubiyara Iron Ore Mine 32.375 ha. at 1(a) PathalewardKatni M.P. DubiyaraTalluka-Sihora Jabalpur M.P. 4 104/2008 1(a) Anand mining corporation Dubiyara-Tikaria Iron ore mine 26.00 ha at Village 1(a) Pathakward, Katni- M.P. Dubiyara Tikaria Jabalpur 5 411/2009 1(a) Shri Kishore Kumar Station Road , Limestone & Dolomite mine 5.605 ha. 6200 TPA 1(a) Katni-M.P. at Village- Chandan Teh- Murwara, Distt-Katni- M.P. 6 412/2009 1(a) M/s Kamal lime Industries Station Lime stone & Dolomite mine 7.205 11500 TPA at 1(a) Road Katni-M.P. Village ChandanTeh-Murwara Katni-M.P. 7 434/2009 1(a) Smt. Rekha Sharma 192, Second Laterite, clay and Red ochre deposit mine 6.83 ha. 1(a) Floor, Rachna Nagar Bhopal-M.P. at village Salebhar Teh- Bahoriband, Distt-Katni- M.P. 8 472/2009 1(a) N.M. Dubash Stone & Lime Co. Pvt Lime stone & Dolomite mine 7.42 ha. production 1(a) Ltd Station Raod, Maihar Satna capacity 1.6 lakhs TPA at village Kachhgawan, –M.P. -
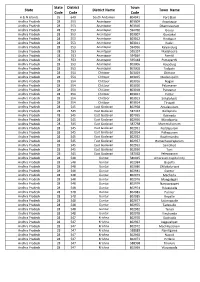
Statutory Towns Size
State District Town State District Name Town Name Code Code Code A & N Islands 35 640 South Andaman 804041 Port Blair Andhra Pradesh 28 553 Anantapur 803009 Anantapur Andhra Pradesh 28 553 Anantapur 803010 Dharmavaram Andhra Pradesh 28 553 Anantapur 594760 Gooty Andhra Pradesh 28 553 Anantapur 803007 Guntakal Andhra Pradesh 28 553 Anantapur 803012 Hindupur Andhra Pradesh 28 553 Anantapur 803011 Kadiri Andhra Pradesh 28 553 Anantapur 594956 Kalyandurg Andhra Pradesh 28 553 Anantapur 595357 Madakasira Andhra Pradesh 28 553 Anantapur 594864 Pamidi Andhra Pradesh 28 553 Anantapur 595448 Puttaparthi Andhra Pradesh 28 553 Anantapur 803006 Rayadurg Andhra Pradesh 28 553 Anantapur 803008 Tadpatri Andhra Pradesh 28 554 Chittoor 803019 Chittoor Andhra Pradesh 28 554 Chittoor 803015 Madanapalle Andhra Pradesh 28 554 Chittoor 803016 Nagari Andhra Pradesh 28 554 Chittoor 803020 Palamaner Andhra Pradesh 28 554 Chittoor 803018 Punganur Andhra Pradesh 28 554 Chittoor 803017 Puttur Andhra Pradesh 28 554 Chittoor 803013 Srikalahasti Andhra Pradesh 28 554 Chittoor 803014 Tirupati Andhra Pradesh 28 545 East Godavari 802958 Amalapuram Andhra Pradesh 28 545 East Godavari 587337 Gollaprolu Andhra Pradesh 28 545 East Godavari 802955 Kakinada Andhra Pradesh 28 545 East Godavari 802956 Mandapeta Andhra Pradesh 28 545 East Godavari 587758 Mummidivaram Andhra Pradesh 28 545 East Godavari 802951 Peddapuram Andhra Pradesh 28 545 East Godavari 802954 Pithapuram Andhra Pradesh 28 545 East Godavari 802952 Rajahmundry Andhra Pradesh 28 545 East Godavari 802957 Ramachandrapuram -

Madhya Pradesh Size:( 5.5
37th Meeting of the Central Sanctioning cum Monitoring Committee(CSMC) under Pradhan Mantri Awas Yojana - Housing For All rd Urban Development & Housing Department 23 August, 2018 Government of Madhya Pradesh Indicators Current Status (No.) . Cities Approved 378 . Demand Survey Completed 378 . Total Demand 11.52 Lakh . Demand received through Common Service Centre 4,44,606 and Online Application . Cases accepted/rejected 2,07,397 . Whether HFAPoA Submitted Yes, For all 378 Towns . Whether AIP Submitted Yes 10,49,665 Surveyed Data Entries have been entered in PMAY . Whether HFAPoA & AIP entered in MIS MIS . SLTC/CLTC staffs approved vs. placed SLTC:10 vs 10 / CLTC: 454 vs 521 Sanctioning: 2.47 Lakh DUs (Excluding CLSS) . Target of DUs in 2018-19 Completion: 5.00 Lakh DUs As per provision of GoI matching budgetary provisions is . State Budgetary Provision for PMAY (U) in 2018-19 ensured in state budget 2 Indicators Current Status (No.) .Survey entry made (%) 87.60% .Projects approved: 887 .Projects entered (7A/B/C/D) 851 .DUs approved under BLC 3,47,242 (Excluding 35,475 Surrendered DUs) .Beneficiaries attached 3,04,186 .Geo-tagged Points 6,77,539 (No. of Unique Houses Geo-Tagged: 2,56,075) 3 Grounded for Construction / In-Progress EWS Work Verticals Houses Tendered Order Completed Approved Issued Foundation Lintel Roof Total AHP 1,49,645 48,499 1,01,146 58,816 18,643 5,748 83,207 17,939 (Including RAY) BLC (N) 3,47,242 - - 1,24,110 26,775 18,767 1,69,652 97,313 ISSR 2,172 960 - - - - - - CLSS 11,616 - - - - - - 11,616 (Including LIG/MIG) -

1. Location of the Plastic Park: Village- Bilaua, Madhya Pradesh 2
1. Location of the Plastic Park: Village- Bilaua, Madhya Pradesh 2. Area of the Park: 93 Acre 3. Total Plots for allotment to units: 107 4. Contact details for further information: Chief General Manager, MP Plastic City Development Corporation Gwalior Ltd IIDC Plaza, 39- City Center, Gwalior-474011 (MP) Ph No: 0751-2374506 Email: [email protected] Website: www.iidcgwalior.com Detailed brochure: See below Plastic Park Billowa, Gwalior District Gwalior Billlowa, Gwalior Madhya Pradesh: A Land of Infinite Business Opportunities MPIDC Government Department of Chemicals & Petro Chemicals A Government. of M.P. Undertaking of Madhya Pradesh Government of India Madhya Pradesh Plastic Park Development Corporation Ltd. (A Government. of M.P. Undertaking) Plastic Park Billowa Distt. Gwalior Govt. of MP’s endeavor to boost manufacturing sector by facilitating the plastic industry to establish base and create employment Industrial Area Profile: Name of Industrial Area :- Plastic Park Billowa Village/Tehsil/District :- Billowa, Dabra, Gwalior Area :- 37.63 Hectare Sector :- Plastic & Polymer based unit Critical Infrastructure Water Availability :- Available – 1 MLD Water Supply Scheme i/c WTP & OHT Power Supply :- Available – 33/11 KV Power Sub Station within Plastic Park Drainage :- Available Street Light :- Available Support Infrastructure Inland Container Depot :- Inland Container Depot Malanpur 45 Kms from Gwalior with direct rail link. Connectivity Airport :- Airport Gwalior 35 Kms from Billowa Dry Port :- Inland Container Depot Malanpur Road -

District Census Handbook, Gwalior, Part XIII-B, Series-11
~TIT XIII-~ ~"tTGJ;rT ~T • sn~fq~ ~T\ttr • iti. m. Ii, "1\(f1q srmuf;{1ti ~"t fifbrcti at,,~, ~rot 1)81, 'ERSUS-PUBLJCATION PLAN (1981 Cen.rus Publications, Series 11 in All India Series will be published in the following parIS) GOVERNMENT OF INDIA PUBLICATIONS Part I-A Administration Report- Enumeration Part I-B Administration Report-Tabulation Part II-A General Population Tables P:ut U-B Pr imary Census Abstract Part III General Economic Tables Part IV Social and Cultural Tables Part V Migration Tables Part VI Fertility Tables Part VII Tables on Houses and Disabled Population P:lIt VIII Household Tables Part IX Special Tables on Scheduled Caltes and Schedlued Tribes Part X-A T own Directory Part X-B Survey Reports on selected Towns Part X-C Survey Reports on selected Villages Part XI Ethnographic Notes and special studies ()n Scheduled Castes and Scheduled Tribes, Part XU . CensUS Atlas Paper I of 198,2 Primary Census Abstract for Scheduled Castes and Scheduled Tribes Pa per I of 198-' Household Population by Religion of Head of Hous.ebold. STA fE GOVERNMENT PUBLICATIONS Part XIlI-A&B District Cellsus Handbook for each of the 45 districts in the State. (Village and Town Directory and Primary Cen,susAbUralOt) fq\1t( ,:q) CONTENTS ~ISO Pages Fbreword j-iv Preface v-vi Map of Gwalior District Important Statistics vii Analytical Note 1Slfr~'11f~<Ii' fcCCfI1;t, ~~~f:qcr ;jfrTcr ~!~ 9;[~~f'T.fq Notes & E.<planations: LIst of Scheduled ~'f~rfij 'fiT ~'CfT (~'!lT)a<f), fqa-l1Cfi 1 979; Castes and Scheduled Tribes Order f:srt:JJ ~'f~QFfT ~ffffCfit -

Indigenous People Planning Framework India: Madhya Pradesh
Indigenous People Planning Framework Document Stage: Draft for Consultation Project Number: 42486-016 November 2016 India: Madhya Pradesh Urban Services Improvement Project (MPUSIP) Prepared by Government of Madhya Pradesh for the Asian Development Bank. ABBREVIATIONS ADB – Asian Development Bank BPL – below poverty line EMP – Environmental Management Plan GOI – Government of India GOMP – Government of Madhya Pradesh GRC – Grievance Redress Committee GRM – Grievance Redress Mechanism IPP – Indigenous People’s Plan MPUDC : Madhya Pradesh Urban Development Company Limited MPUIF : Madhya Pradesh Urban Infrastructure Fund MPUSIP : Madhya Pradesh Urban Services Improvement Project PIU – project implementation unit PMC – project management consultants PMU – Project management unit PO (SSG) – Project Officer (Social Safeguard and Gender) NGO – non-government organization SPS – safeguard policy statement UADD - Urban Administration and Development Directorate UDHD - Urban Development and Housing Department ULB - urban local body WTP - water treatment plant WEIGHTS AND MEASURES Cum – cubic meter Ha – hectares Km – Kilometer mm – Millimeter MCM – micrograms per cubic meter NOTES (i) The fiscal year (FY) of the Government of India and its agencies begins on 1 April and ends on 31 March. “FY” before a calendar year denotes the year in which the fiscal year ends, e.g., FY2016 begins on 1 April 2016 and ends on 31 March 2017. (ii) In this report, "$" refers to US dollars. This indigenous peoples planning framework is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, ADB does not intend to make any judgments as to the legal or other status of any territory or area. -

District Census Handbook, Shivpuri, Part XIII-B, Series-11
1ITtT XIII-V ;fifQvr;:rT 'fiT • sn~f,,~ m'(m • itr. m. ~i, 'lTR:t=im smtfff;{qr; it., f"~~ iII';f'fQfifT q't;qsrQ "198i*crNSUS-PUBLlCATION PI.AN (1981 C~MUJ Publications, Series 11 in All India Series will be published in the following 'parl&) GOVERNMENT OF INDIA PUBLICATIONS Part I-A Administration Report-Enumeration Part I-B Administration Report-Tahulation Part II-A General Population Tables Part II-B Primary Census Abstract Part 111 General Economic Tables Part IV Social and Cultural Tables Part V Migration Tables Part VI Ferti Iity Tahles Part VU Tables on Houses and Disahled Population Part VIII Household Tables Part IX Special Tables on Sched uled Castes and Schedlued Tribes Part X-A Town Directory Part X-8 Survey Reports on selected Towns Part X-C Survey Reports on selec ted ViUages Part Xl Ethnographic Notes and special stud ies on Sched uled Castes and Scheduled Tribes Part XU . Census Atlas Paper I of [982 Primary Census Abstra::t for Scheduled Castes and Sche il.hi Tribes Paper I of 1984 HousehoJd Population by Relighn of Head of Household STATE GOVERNMENT PUBLICATrONS Part XIH-A&B District Census Handbook for each of the 45 districts in tile Stlt:. (Village and Town Dir~ctory anti Primary Census Abstract) CONTENTS '{ISO' Pages Fereword i-iv Preface v-vi District Map Important Statistics vii Analytical Note 1-25 G~T191.fTc~iIi fztq'1JI1, q'i~f:qcr mfcr 1R')'t ~i~f:qij' Notes & EXplanations: List of Scheduled \ifi'f"l'Tfcr ~r ~'<it (ij'~ra<f), fq~zrili I 979; Castes and Scheduled Tribes Order r\if~T \ifi'f~QJi'fT ~r~crilir -

Action Plan for Municipal Solid Waste Management in Madhya Pradesh
l3J MADHYA PRAI)ESII POLLTJ'I'ION CONTIIOL BoARI) -462016 # PatyqworaspaMaL E:5-4!9ra lE'o lonl Uhopal \l7t (0755)246,1428. 24661 9l lrax: (0755)2'161742 E-mailiit'mppcb'rlrcdillinail'com l6aj Bhopcl. Ddlcd 17,08 /lli l8 No i II()/MSWi N4PPCI}/]OI X lo. l'hc Membcr Secrelxn'. (-cntral Pollulion Conlrol Board. Parivash Bhawan. CBD curr oltice Cornplex' llast Ariun Nagar..l)clhi Ll00l2 ol'Solid Wasle Managomcnl Rrrlo\' ]0 I ()' Subi /\nnual liepofl 1br )car 20 I 7- I 8 on Implementrlion Sir. Managcrncnt Rulcs l0l6' ,\s per the provision of thc rulc 24 (ll) ol'Solid Wastc year 2017-18 on Solid Wa\lu Mltna':ctrcnr in PI,-'0sc find cnclosed herc\\ith the Annual lleport Ibr liom (\') tbr your inlbrmation & neccssary action plcase' subrrission ol Anrlual llenons- l he d'iir 'l hc report is dcla)'cd as TJADD is nol regular in O{llccs ol'M l']'lL( prcsenlsd irr the report have bccn galhered through Regional 'll' lrncl i As abole i\h ral S((rrlx r t tl7Y Bh,'Fal. l)atcd l7 /U8 'l(rl 8 I)rdl.No. n ro/MSW/MPPClli 2018 Cop\ to :- Itousing & Dcptl- C(}vl. {l1' \1 l' t. Prir(ipcl \((r.lar\. I rhdn D(\LIrplnurll \tintraldlc. Bh,\pll lbr inll'rmallon plca'(' 1br upload thc sanrc on Wch Si{c ()1. 2. tl M.P. PollLrtion Conlrol Board llhopal M PPf] B. |nc| | r\s ahovc olc \9( Form - V lsco rulc 2,1(.3)l Annurl rcport ol Municipal Solicl Wdste i\lxnaiacmcnt oflladhla I,radcsh PART - A l'o, The Chairman Central Pollution Control Bo{rd Parivesh Bhawan, llast Arjun Nagar Dr.].HI- I100032 . -

Service Electors Voter List
FINAL ELECTORAL ROLL - 2021 STATE - (S12) MADHYA PRADESH No., Name and Reservation Status of Assembly Constituency: 14-GWALIOR Last Part RURAL(GEN) No., Name and Reservation Status of Parliamentary Service Constituency in which the Assembly Constituency is located: 3-GWALIOR(GEN) Electors 1. DETAILS OF REVISION Year of Revision : 2021 Type of Revision : Special Summary Revision Qualifying Date :01/01/2021 Date of Final Publication: 15/01/2021 2. SUMMARY OF SERVICE ELECTORS A) NUMBER OF ELECTORS 1. Classified by Type of Service Name of Service No. of Electors Members Wives Total A) Defence Services 823 13 836 B) Armed Police Force 0 0 0 C) Foreign Service 0 0 0 Total in Part (A+B+C) 823 13 836 2. Classified by Type of Roll Roll Type Roll Identification No. of Electors Members Wives Total I Original Mother roll Integrated Basic roll of revision 823 13 836 2021 II Additions Supplement 1 After Draft publication, 2021 0 0 0 List Sub Total: 0 0 0 III Deletions Supplement 1 After Draft publication, 2021 0 0 0 List Sub Total: 0 0 0 Net Electors in the Roll after (I + II - III) 823 13 836 B) NUMBER OF CORRECTIONS/MODIFICATION Roll Type Roll Identification No. of Electors Supplement 1 After Draft publication, 2021 0 Total: 0 Elector Type: M = Member, W = Wife Page 1 Final Electoral Roll, 2021 of Assembly Constituency 14-GWALIOR RURAL (GEN), (S12) MADHYA PRADESH A . Defence Services Sl.No Name of Elector Elector Rank Husband's Address of Record House Address Type Sl.No. Officer/Commanding Officer for despatch of Ballot Paper (1) (2) (3) (4) (5) (6) (7) Assam Rifles 1 JITENDRA SINGH M Rifleman Headquarter Directorate General N.C.H.