(Rh) Factor Studies, Dr. Bruce Chown, and the Faculty Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DMJ.1936.2.1.A02.Young.Pdf (3.644Mb)
DALHOUSIE MEDICAL JOURNAL 5 A Memorable Conference THE HARVARD TERCENTENARY 1636 - 1936 E. GORDON YOUNG, B.A., M.Sc., Ph.D., F.R.S.C. OMEONE has said that the most valuable and rarest thing in the world S is a new idea. It is the verdict or the intellectual world of science, of art and of music that progress centres largely about the thoughts ex pressed by the few great minds of the centuries. The work of the scientists of the world has been likened to a great canvas, the subject of which has been chosen by the few and the first bold lines inserted, but the great mass of colour and detail has been supplied by the many faithful apprentices. It was most fitting that the oldest and greatest of American Universities should celebrate its three hundredth birthday in an intellec tual feast and that it should invite to its table as leaders of conversation the greatest minds of the world in those subjects which were proposed for discussion. Harvard.!J.as a magnificent record of intellectual tolerance and its hospitality was open to individuals of all nationalities and all re- ligious and political creeds. To Cambridge thus in the early days of September, 1936, there came, by invitation, a group of about two thousand five hundred American and Canadian scholars to participate in a memorable series of symposia led by a special group of sixty-seven eminent scientists and men of letters from fifteen different countries. These included no fewer than eleven men who had the greatest single distinction in the realms of science and of letters, the Nobel Prize. -

Animal Models of Obesity and Diabetes Mellitus
UC Davis UC Davis Previously Published Works Title Animal models of obesity and diabetes mellitus. Permalink https://escholarship.org/uc/item/3z3879vp Journal Nature reviews. Endocrinology, 14(3) ISSN 1759-5029 Authors Kleinert, Maximilian Clemmensen, Christoffer Hofmann, Susanna M et al. Publication Date 2018-03-01 DOI 10.1038/nrendo.2017.161 Peer reviewed eScholarship.org Powered by the California Digital Library University of California REVIEWS Animal models of obesity and diabetes mellitus Maximilian Kleinert1–4, Christoffer Clemmensen1–3, Susanna M. Hofmann3,5,6, Mary C. Moore7, Simone Renner3,8, Stephen C. Woods9, Peter Huypens3,10, Johannes Beckers3,10,11, Martin Hrabe de Angelis3,10,11, Annette Schürmann3,12, Mostafa Bakhti3,5,13, Martin Klingenspor14,15,16, Mark Heiman17, Alan D. Cherrington7, Michael Ristow18, Heiko Lickert3,5,13, Eckhard Wolf3,8, Peter J. Havel19, Timo D. Müller1–3 and Matthias H. Tschöp1–3 Abstract | More than one-third of the worldwide population is overweight or obese and therefore at risk of developing type 2 diabetes mellitus. In order to mitigate this pandemic, safer and more potent therapeutics are urgently required. This necessitates the continued use of animal models to discover, validate and optimize novel therapeutics for their safe use in humans. In order to improve the transition from bench to bedside, researchers must not only carefully select the appropriate model but also draw the right conclusions. In this Review, we consolidate the key information on the currently available animal models of obesity and diabetes and highlight the advantages, limitations and important caveats of each of these models. On the current trajectory, over half of the adult pop- To tackle these objectives, researchers rely on diverse ani- ulation in the United States will be obese by 2030, and mal models that span multiple species and strategic scien- similar increments are likely to occur in other developed tific approaches. -

Polyuria) Mellitus – Sweet
Hormones: the birth of a concept and how it gained recognition U3A Course, Spring Series 2017 Gil Barbezat What I plan to talk about: • First Session: History of hormones; concepts to chemicals Stories behind some key discovery milestones Technological help in advances • Second Session: How hormones work Hormones’ role in digestion Gut hormones in excess (tumours) What do you associate with the word ‘Hormone’ • Sex, Puberty, Menopause? • Body building, Athletes? • Maybe? Digestion Urine production Blood production and BP Brain function • Regulates our entire metabolism Early ‘application’ - Eunuchs • Intentional castration • Summerian city of Lagash in 21st C BCE Southern Mesopotamia (Iraq) • Applications: Guardians of rulers or women Singers Courtiers and domestics Why did this happen? Albrecht von Haller (1708 – 77) • Swiss poet, naturalist, theologian, anatomist, physiologist • “Father of experimental physiology” • Body ‘emanations’: Bile digests fat Body a reactive organism Salivary gland duct a blood vessel (MD) Theophile de Bordeu (1722 – 76) • French poet, philosopher, physician • Organs specific sensibilities • Each organ of the body produced a specific ‘emanation’ (humour) which it secreted into the bloodstream Claude Bernard (1813 – 78) Claude Bernard • Vaudeville comedy to medicine Med School in Paris 1834; physiology • Father of “Experimental medicine” Vivisection • ‘Milieu interieur’ Walter Bradford Cannon (1871 – 1945) • American physiologist at Harvard • Worked in lab of Henry Bowditch, a pupil of Bernard • Enlarged Bernard’s -

Banting and Best: the Extraordinary Discovery of Insulin
106 Rev Port Endocrinol Diabetes Metab. 2017;12(1):106-115 Revista Portuguesa de Endocrinologia, Diabetes e Metabolismo www.spedmjournal.com Artigo de Revisão Banting and Best: The Extraordinary Discovery of Insulin Luís Cardosoa,b, Dírcea Rodriguesa,b, Leonor Gomesa,b, Francisco Carrilhoa a Department of Endocrinology, Diabetes, and Metabolism, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal b Faculty of Medicine of the University of Coimbra, Coimbra, Portugal INFORMAÇÃO SOBRE O ARTIGO ABSTRACT Historial do artigo: Diabetes was a feared disease that most certainly led to death before insulin discovery. During the first Recebido a XX de XXXX de 201X two decades of the 20th century, several researchers tested pancreatic extracts, but most of them caused Aceite a XX de XXXX de 201X Online a 30 de junho de 2017 toxic reactions impeding human use. On May 1921, Banting, a young surgeon, and Best, a master’s student, started testing the hypothesis that, by ligating the pancreatic ducts to induce atrophy of the exocrine pancreas and minimizing the effect of digestive enzymes, it would be possible to isolate the Keywords: internal secretion of the pancreas. The research took place at the Department of Physiology of the Diabetes Mellitus University of Toronto under supervision of the notorious physiologist John MacLeod. Banting and Insulin/history Best felt several difficulties depancreatising dogs and a couple of weeks after the experiments had Pancreatic Extracts/history begun most of the dogs initially allocated to the project had succumbed to perioperative complications. When they had depancreatised dogs available, they moved to the next phase of the project and prepared pancreatic extracts from ligated atrophied pancreas. -

Nobel Laureate Surgeons
Literature Review World Journal of Surgery and Surgical Research Published: 12 Mar, 2020 Nobel Laureate Surgeons Jayant Radhakrishnan1* and Mohammad Ezzi1,2 1Department of Surgery and Urology, University of Illinois, USA 2Department of Surgery, Jazan University, Saudi Arabia Abstract This is a brief account of the notable contributions and some foibles of surgeons who have won the Nobel Prize for physiology or medicine since it was first awarded in 1901. Keywords: Nobel Prize in physiology or medicine; Surgical Nobel laureates; Pathology and surgery Introduction The Nobel Prize for physiology or medicine has been awarded to 219 scientists in the last 119 years. Eleven members of this illustrious group are surgeons although their awards have not always been for surgical innovations. Names of these surgeons with the year of the award and why they received it are listed below: Emil Theodor Kocher - 1909: Thyroid physiology, pathology and surgery. Alvar Gullstrand - 1911: Path of refracted light through the ocular lens. Alexis Carrel - 1912: Methods for suturing blood vessels and transplantation. Robert Barany - 1914: Function of the vestibular apparatus. Frederick Grant Banting - 1923: Extraction of insulin and treatment of diabetes. Alexander Fleming - 1945: Discovery of penicillin. Walter Rudolf Hess - 1949: Brain mapping for control of internal bodily functions. Werner Theodor Otto Forssmann - 1956: Cardiac catheterization. Charles Brenton Huggins - 1966: Hormonal control of prostate cancer. OPEN ACCESS Joseph Edward Murray - 1990: Organ transplantation. *Correspondence: Shinya Yamanaka-2012: Reprogramming of mature cells for pluripotency. Jayant Radhakrishnan, Department of Surgery and Urology, University of Emil Theodor Kocher (August 25, 1841 to July 27, 1917) Illinois, 1502, 71st, Street Darien, IL Kocher received the award in 1909 “for his work on the physiology, pathology and surgery of the 60561, Chicago, Illinois, USA, thyroid gland” [1]. -

The Worshipful Society of Apothecaries of London Galen Medal Winners
The Worshipful Society of Apothecaries of London Galen Medal Winners 1926 Prof WE DIXON, BSc, MA, MD, DPH, FRS Pharmacology 1927 Sir Gowland HOPKINS, MA, LLD, DSc, FRCP, FRIC, FRS Discovery of vitamins 1928 Prof JJ ABEL, MD, ScD, LLD Isolation of Adrenaline 1930 Prof E FOURNEAU, Directeur de 1'Institute Pasteur Pharmacology of amino-alcohols 1932 Sir Henry DALE, OM, GBE, MA, MD, FRCP, FRS Neurophysiology 1934 Prof Sir Frederick BANTING, MC, Hon FRCS, DSc, LLD Discovery of Insulin 1946 Sir Alexander FLEMING, FRCP, FRCS, FRS Penicillin Lord FLOREY, MA, MD, FRCP, FRS 1947 F CURD, BSc, PhD D DAVEY, MSc, PhD Discovery of Paludrine F ROSE, BSc, PhD 1948 Sir Lionel WHITBY, CVO, MC, MD, FRCP Sulphonamides 1949 Prof J TREFOUEL, Directeur de 1'Institute Pasteur Sulphonamides 1951 Prof Sir Charles DODDS, Bt, MVO, MD, FRCP, FRS Biochemistry 1953 Sir Charles HARINGTON, MA, PhD, FRS Synthesised Thyroxin 1954 EL SMITH, DSc, FRIC Vitamin B12 1955 Lord BROCK, MS, FRCS Cardiac surgery 1957 Prof Sir Ernst CHAIN, MA, DPhil, FRS Production of Penicillin 1958 Sir Macfarlane BURNET, OM, MD, FRCP, FRS Vaccines for virus infections 1959 Prof Sir Bradford HILL, CBE, PhD, DSc, FRS Medical statistics 1960 Sir Tudor THOMAS, DSc, MD, MS, FRCS Corneo-plastic surgery 1961 Prof R PATERSON, CBE, MC, MD, FRCS, FFR Radiotherapy 1962 Prof W PENFIELD, OM, CMG, MD, DSc, FRS Neurosurgery & Neurophysiology 1963 Prof Sir Alexander HADDOW, MD, DSc, PhD, FRS Experimental pathology & cancer research 1964 FP DOYLE, MSc, FRIC Chemical & biological GN ROLINSON, BSc, PhD development -

ILAE Historical Wall02.Indd 2 6/12/09 12:02:12 PM
1920–1929 1923 1927 1929 John Macloed Julius Wagner–Jauregg Sir Frederick Hopkins 1920920 1922922 1924924 1928928 August Krogh Otto Meyerhof Willem Einthoven Charles Nicolle 1922922 1923923 1926926 192992929 Archibald V Hill Frederick Banting Johannes Fibiger Christiann Eijkman 1920 The positive eff ect of the ketogenic diet on epilepsy is documented critically 1921 First case of progressive myoclonic epilepsy described 1922 Resection of adrenal gland used as treatment for epilepsy 1923 Dandy carries out the fi rst hemispherectomy in a human patient 1924 Hans Berger records the fi rst human EEG (reported in 1929) 1925 Pavlov fi nds a toxin from the brain of a dog with epilepsy which when injected into another dog will cure epilepsy – hope for human therapy 1926 Publication of L.J.J. Musken’s book Epilepsy: comparative pathogenesis, symptoms and treatment 1927 Cerebral angiography fi rst attempted by Egaz Moniz 1928 Wilder Penfi eld spends time in Foerster’s clinic and learns epilepsy surgical techniques. 1928 An abortive attempt to restart the ILAE fails 1929 Penfi eld’s fi rst ‘temporal lobectomy’ (a cortical resection) 1920 Cause of trypanosomiasis discovered 1925 Vitamin B discovered by Joseph Goldberger 1921 Psychodiagnostics and the Rorschach test invented 1926 First enzyme (urease) crystallised by James Sumner 1922 Insulin isolated by Frecerick G. Banting and Charles H. Best treats a diabetic patient 1927 Iron lung developed by Philip Drinker and Louis Shaw for the fi rst time 1928 Penicillin discovered by Alexander Fleming 1922 State Institute for Racial Biology formed in Uppsala 1929 Chemical basis of nerve impulse transmission discovered 1923 BCG vaccine developed by Albert Calmette and Jean–Marie Camille Guérin by Henry Dale and Harold W. -
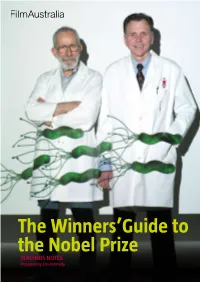
The Winners'guide to the Nobel Prize
The Winners’Guide to the Nobel Prize TEACHERS NOTES Prepared by Cris Kennedy THE WINNERS’ GUIDE TO THE NOBEL PRIZE TEACHERS Notes PAGE 1 Synopsis What does it take to win a Nobel Prize? Guts? Brilliance? Eccentricity? This film travels behind the scenes of the world’s most prestigious prize and into the minds of two of the people who have reached this pinnacle of excellence. In the most isolated capital city in the world, Perth, Western Australia, two scientists are interrupted while enjoying their fish and chips lunch by a phone call from Stockholm, Sweden. They have just been informed that they have been awarded the 2005 Nobel Prize for Medicine and could they make it to the awards ceremony? Australian scientists Barry Marshall and Robin Warren journey to the prize-winners’ podium is more than just a trip to the opposite side of the world to sub-zero temperatures, cultural pomp and extreme Swedish scheduling—it has been a career of trial and error, endless research and Aussie-battler-style stubborn determination. Today, this odd couple of science travel the globe as heroes—ambassadors to the science world—but it was 23 years ago in a modest hospital laboratory in Perth, that Marshall and Warren discovered a bacterium that survived in the human stomach that they called Helicobacter pylori. They believed that this bacterium, not stress, caused gastritis and peptic stomach ulcers, much to the chagrin of the medical world, which at the time scorned them. After years of careful observation, luck and persistence, they finally had the breakthrough they needed, but not before Marshall infected himself, using his own body as a guinea pig to test their theory. -

Frederick Banting and the Group of Seven
Nouvelles et analyses Frederick Banting and the Group of Seven In 1925, fame rested heavily on the shoulders of Sir Frederick This interest led him to membership in Toronto’s Arts Banting, whose name had become closely associated with the and Letters Club, the meeting place for some of Canada’s discovery of insulin 3 years earlier. A reticent man, Banting best-known artists, including the Group of Seven. Banting found public speaking difficult and the hounding of the press became friends with the group’s founding member and one unbearable. He found relief from the rigours of professional of Canada’s leading landscape artists, A.Y. Jackson. life through his passion for water colours and sketching. At first glance the scientist and artist might appear to have little in common, but there were many common threads. Both men served on the Western Front during WW I, and both had been wounded and convalesced in England. Both had an interest in military art and a passion for the outdoors and landscape painting. Over the next 16 years, Jackson invited Banting to ac- company him on a number of his sketching trips — some lasting as long as 2 months. They sketched from the Geor- gian Bay area to wintertime rural Quebec; there, they bil- leted with local farm families. They also travelled to the Eastern Arctic, where they became the first artists to sketch Hudson Bay trading posts. For Banting, these trips meant a break from the pres- sures of his medical research. Jackson was a mentor and teacher, often looking over Banting’s work and making suggestions for improving it. -

Physiology and Behavioral Science in Gaetano Martino: Reflections on A
Mediterranean Journal of Clinical Psychology MJCP ISSN: 2282-1619 VOL III N.3 (2015) Physiology and behavioral Science in Gaetano Martino: Reflections on a physiologist’s endeavor to discover the mind Salvatore Settineri1, Carmela Mento1, Giuseppe Gembillo2, Maria Midili2 1Department of Biomedical and Dental Sciences and Morphofunctional Imaging University of Messina 2Department of Cognitive Science, Education and Cultural Studies, University of Messina, Italy. 3 Psychological Student, University of Messina Email Corresponding author: [email protected] Abstract: This article aims to underline the organic way of working of an eclectic scientist and politician by the name of Gaetano Martino and his studies on nutrition, experimental reflex epilepsy and conditioned reflexes. The studies on conditioned reflexes were analyzing by Martino because he did not fully agree with Pavlov’s ideas regarding the modifications of the reflex arc subsequent to the formation of a conditioned reflex. Furthermore, thanks to his studies on conditioned reflexes, psychology and psychiatry have found, and continue to find, important developments towards the understanding of man's personality. The Messines physiologist, by virtue of his indisputable dedication and passion for research, managed to open a prolific dialogue between two apparently distinct and distant disciplines, actively moving towards an interdisciplinary approach, thus anticipating a basic principle of present-day science. Keywords: Gaetano Martino, Ivan Pavlov, conditioned reflexes, classical conditioning, psychology, nutrition, psychiatry, experimental reflex epilepsy. 2 SETTINERI, MENTO ET AL. Introduction In the past century, psychological and medical disciplines have become progressively more specialized and, thanks to interdisciplinary approaches, they currently work together actively and in total synergy in order to promote the advancement of knowledge. -

Timecapsule Insulin's Centenary
TimeCapsule Insulin’s centenary: the birth of an idea Robert A Hegele, Grant M Maltman At 2:00 h on Oct 31, 1920, Frederick G Banting, a surgeon practising in London, ON, Canada, conceived an idea to Lancet Diabetes Endocrinol 2020 isolate the internal secretion of the pancreas. The following week, he met with noted scientist John J R Macleod in Published Online Toronto, ON, Canada, and they developed a research plan. By August, 1921, Banting and his student assistant October 29, 2020 Charles H Best had prepared an effective extract from a canine pancreas. In January, 1922, biochemist James B Collip https://doi.org/10.1016/ S2213-8587(20)30337-5 isolated insulin that was sufficiently pure for human use. On Oct 25, 1923, Banting and Macleod received the Nobel Department of Medicine, Prize in Physiology or Medicine for the discovery of insulin. Here, we recount the most relevant events before and Department of Biochemistry, after the fateful early morning of Oct 31, 1920, which culminated in the discovery and clinical use of insulin. and Robarts Research Institute, Schulich School of Medicine Introduction Captain and posted near the front line in France. At the and Dentistry, Western University, London, ON, The discovery of insulin in Canada ranks among the Battle of Cambrai in September, 1918, he suffered a Canada (R A Hegele MD); and leading triumphs of medical research; but is there an shrapnel wound to his dominant right arm, which Banting House National appropriate date to observe the centenary of this became infected and healed slowly. Although he received Historic Site of Canada, landmark achievement? There are several candidate the Military Cross for valour, he most likely endured Diabetes Canada, London, ON, Canada (G M Maltman BA) milestones in the timeline that culminated in the post-traumatic stress disorder.10 Correspondence to: isolation of insulin suitable for human use (figure 1). -

List of Nobel Laureates 1
List of Nobel laureates 1 List of Nobel laureates The Nobel Prizes (Swedish: Nobelpriset, Norwegian: Nobelprisen) are awarded annually by the Royal Swedish Academy of Sciences, the Swedish Academy, the Karolinska Institute, and the Norwegian Nobel Committee to individuals and organizations who make outstanding contributions in the fields of chemistry, physics, literature, peace, and physiology or medicine.[1] They were established by the 1895 will of Alfred Nobel, which dictates that the awards should be administered by the Nobel Foundation. Another prize, the Nobel Memorial Prize in Economic Sciences, was established in 1968 by the Sveriges Riksbank, the central bank of Sweden, for contributors to the field of economics.[2] Each prize is awarded by a separate committee; the Royal Swedish Academy of Sciences awards the Prizes in Physics, Chemistry, and Economics, the Karolinska Institute awards the Prize in Physiology or Medicine, and the Norwegian Nobel Committee awards the Prize in Peace.[3] Each recipient receives a medal, a diploma and a monetary award that has varied throughout the years.[2] In 1901, the recipients of the first Nobel Prizes were given 150,782 SEK, which is equal to 7,731,004 SEK in December 2007. In 2008, the winners were awarded a prize amount of 10,000,000 SEK.[4] The awards are presented in Stockholm in an annual ceremony on December 10, the anniversary of Nobel's death.[5] As of 2011, 826 individuals and 20 organizations have been awarded a Nobel Prize, including 69 winners of the Nobel Memorial Prize in Economic Sciences.[6] Four Nobel laureates were not permitted by their governments to accept the Nobel Prize.