Nobel Laureate Surgeons
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unrestricted Immigration and the Foreign Dominance Of
Unrestricted Immigration and the Foreign Dominance of United States Nobel Prize Winners in Science: Irrefutable Data and Exemplary Family Narratives—Backup Data and Information Andrew A. Beveridge, Queens and Graduate Center CUNY and Social Explorer, Inc. Lynn Caporale, Strategic Scientific Advisor and Author The following slides were presented at the recent meeting of the American Association for the Advancement of Science. This project and paper is an outgrowth of that session, and will combine qualitative data on Nobel Prize Winners family histories along with analyses of the pattern of Nobel Winners. The first set of slides show some of the patterns so far found, and will be augmented for the formal paper. The second set of slides shows some examples of the Nobel families. The authors a developing a systematic data base of Nobel Winners (mainly US), their careers and their family histories. This turned out to be much more challenging than expected, since many winners do not emphasize their family origins in their own biographies or autobiographies or other commentary. Dr. Caporale has reached out to some laureates or their families to elicit that information. We plan to systematically compare the laureates to the population in the US at large, including immigrants and non‐immigrants at various periods. Outline of Presentation • A preliminary examination of the 609 Nobel Prize Winners, 291 of whom were at an American Institution when they received the Nobel in physics, chemistry or physiology and medicine • Will look at patterns of -

書 名 等 発行年 出版社 受賞年 備考 N1 Ueber Das Zustandekommen Der
書 名 等 発行年 出版社 受賞年 備考 Ueber das Zustandekommen der Diphtherie-immunitat und der Tetanus-Immunitat bei thieren / Emil Adolf N1 1890 Georg thieme 1901 von Behring N2 Diphtherie und tetanus immunitaet / Emil Adolf von Behring und Kitasato 19-- [Akitomo Matsuki] 1901 Malarial fever its cause, prevention and treatment containing full details for the use of travellers, University press of N3 1902 1902 sportsmen, soldiers, and residents in malarious places / by Ronald Ross liverpool Ueber die Anwendung von concentrirten chemischen Lichtstrahlen in der Medicin / von Prof. Dr. Niels N4 1899 F.C.W.Vogel 1903 Ryberg Finsen Mit 4 Abbildungen und 2 Tafeln Twenty-five years of objective study of the higher nervous activity (behaviour) of animals / Ivan N5 Petrovitch Pavlov ; translated and edited by W. Horsley Gantt ; with the collaboration of G. Volborth ; and c1928 International Publishing 1904 an introduction by Walter B. Cannon Conditioned reflexes : an investigation of the physiological activity of the cerebral cortex / by Ivan Oxford University N6 1927 1904 Petrovitch Pavlov ; translated and edited by G.V. Anrep Press N7 Die Ätiologie und die Bekämpfung der Tuberkulose / Robert Koch ; eingeleitet von M. Kirchner 1912 J.A.Barth 1905 N8 Neue Darstellung vom histologischen Bau des Centralnervensystems / von Santiago Ramón y Cajal 1893 Veit 1906 Traité des fiévres palustres : avec la description des microbes du paludisme / par Charles Louis Alphonse N9 1884 Octave Doin 1907 Laveran N10 Embryologie des Scorpions / von Ilya Ilyich Mechnikov 1870 Wilhelm Engelmann 1908 Immunität bei Infektionskrankheiten / Ilya Ilyich Mechnikov ; einzig autorisierte übersetzung von Julius N11 1902 Gustav Fischer 1908 Meyer Die experimentelle Chemotherapie der Spirillosen : Syphilis, Rückfallfieber, Hühnerspirillose, Frambösie / N12 1910 J.Springer 1908 von Paul Ehrlich und S. -
Fleming Vs. Florey: It All Comes Down to the Mold Kristin Hess La Salle University
The Histories Volume 2 | Issue 1 Article 3 Fleming vs. Florey: It All Comes Down to the Mold Kristin Hess La Salle University Follow this and additional works at: https://digitalcommons.lasalle.edu/the_histories Part of the History Commons Recommended Citation Hess, Kristin () "Fleming vs. Florey: It All Comes Down to the Mold," The Histories: Vol. 2 : Iss. 1 , Article 3. Available at: https://digitalcommons.lasalle.edu/the_histories/vol2/iss1/3 This Paper is brought to you for free and open access by the Scholarship at La Salle University Digital Commons. It has been accepted for inclusion in The iH stories by an authorized editor of La Salle University Digital Commons. For more information, please contact [email protected]. The Histories, Vol 2, No. 1 Page 3 Fleming vs. Florey: It All Comes Down to the Mold Kristen Hess Without penicillin, the world as it is known today would not exist. Simple infections, earaches, menial operations, and diseases, like syphilis and pneumonia, would possibly all end fatally, shortening the life expectancy of the population, affecting everything from family-size and marriage to retirement plans and insurance policies. So how did this “wonder drug” come into existence and who is behind the development of penicillin? The majority of the population has heard the “Eureka!” story of Alexander Fleming and his famous petri dish with the unusual mold growth, Penicillium notatum. Very few realize that there are not only different variations of the Fleming discovery but that there are also other people who were vitally important to the development of penicillin as an effective drug. -

Special Edition Inside
A Publication by The American Society for the Pharmacology and Experimental Therapeutics Pharmacologist Inside: Feature articles from 2014-2015 Special Edition VISIT THE ASPET CAREER CENTER TODAY! WWW.ASPET.ORG/CAREERCENTER/ 4 5 12 21 30 41 WHAT YOU NEED: ASPET’S CAREER CENTER HAS IT 52 Jobseekers: Employers: No registration fee Searchable résumé database Advanced search options Hassle-free posting; online account management tools 61 Sign up for automatic email notifi cations of new jobs that Reach ASPET’s Twitter followers (over 1,000), match your criteria LinkedIn Members (over 2,000), and email subscribers (over 4,000) Free & confi dential résumé posting 71 Post to just ASPET or to entire NHCN network Access to jobs posted on the National Healthcare Career Network (NHCN) Sign up for automatic email notifications of new résumés that match your criteria Career management resources including career tips, coaching, résumé writing, online profi le development, Job activity tracking and much more ASPET is committed to your success: The ASPET Career Center is the best resource for matching job seekers and employers in the pharmacology and related health science fi elds. Our vast range of resources and tools will help you look for jobs, fi nd great employees, and proactively manage 9650 Rockville Pike, Bethesda, MD 20814-3995 your career goals. Main Office: 301.634.7060 www.aspet.org ASPET Career Center Full Page Ad 2015 Updated.indd 1 1/15/2016 3:18:16 PM The Pharmacologist is published and distributed by the American Society for Pharmacology and Experimental Therapeutics. THE PHARMACOLOGIST VISIT THE ASPET CAREER CENTER TODAY! PRODUCTION TEAM Rich Dodenhoff Catherine Fry, PhD WWW.ASPET.ORG/CAREERCENTER/ Judith A. -

October 24–26, 2021 2
SCIENCE · INNOVATION · POLICIES WORLD HEALTH SUMMIT BERLIN, GERMANY & DIGITAL OCTOBER 24–26, 2021 2 “No-one is safe from COVID-19; “All countries have signed up to Universal no-one is safe until we are all Health Coverage by 2030. But we cannot safe from it. Even those who wait ten years. We need health systems conquer the virus within their that work, before we face an outbreak own borders remain prisoners of something more contagious than within these borders until it is COVID-19; more deadly; or both.” conquered everywhere.” ANTÓNIO GUTERRES Secretary-General, United Nations FRANK-WALTER STEINMEIER Federal President, Germany “We firmly believe that the “All pulling together—this must rights of women and girls be the hallmark of the European are not negotiable.” Health Union. I believe this can NATALIA KANEM be a test case for true global Executive Director, United Nations Population Fund (UNFPA) health compact. The need for leadership is clear and I believe the European Union must as- sume this responsibility.” “The lesson is clear: a strong health URSULA VON DER LEYEN system is a resilient health system. Health President, European Commission systems and preparedness are not only “Governments of countries an investment in the future, they are the that are doing well during foundation of our response today.” the pandemic have not TEDROS ADHANOM GHEBREYESUS Director-General, World Health Organization (WHO) only shown political leader- ship, but also have listened “If we don’t address the concerns and to scientists and followed fears we will not do ourselves a favor. their recommendations.” In the end, it is about how technology SOUMYA SWAMINATHAN Chief Scientist, World Health can be advanced as well as how Organization (WHO) we can make healthcare more human.” BERND MONTAG President and CEO, Siemens Healthineers AG, Germany “The pandemic has brought to light the “Academic collabo ration is importance of digital technologies and in place and is really a how it can radically bridging partnership. -

See the Scientific Petition
May 20, 2016 Implement the Endangered Species Act Using the Best Available Science To: Secretary Sally Jewell and Secretary Penny Prtizker We, the under-signed scientists, recommend the U.S. government place species conservation policy on firmer scientific footing by following the procedure described below for using the best available science. A recent survey finds that substantial numbers of scientists at the U.S. Fish and Wildlife Service (FWS) and the National Oceanic and Atmospheric Administration believe that political influence at their agency is too high.i Further, recent species listing and delisting decisions appear misaligned with scientific understanding.ii,iii,iv,v,vi For example, in its nationwide delisting decision for gray wolves in 2013, the FWS internal review failed the best science test when reviewed by an independent peer-review panel.vii Just last year, a FWS decision not to list the wolverine ran counter to the opinions of agency and external scientists.viii We ask that the Departments of the Interior and Commerce make determinations under the Endangered Species Actix only after they make public the independent recommendations from the scientific community, based on the best available science. The best available science comes from independent scientists with relevant expertise who are able to evaluate and synthesize the available science, and adhere to standards of peer-review and full conflict-of-interest disclosure. We ask that agency scientific recommendations be developed with external review by independent scientific experts. There are several mechanisms by which this can happen; however, of greatest importance is that an independent, external, and transparent science-based process is applied consistently to both listing and delisting decisions. -

Sir Charles Sherrington'sthe Integrative Action of the Nervous System: a Centenary Appreciation
doi:10.1093/brain/awm022 Brain (2007), 130, 887^894 OCCASIONAL PAPER Sir Charles Sherrington’sThe integrative action of the nervous system: a centenary appreciation Robert E. Burke Formerly Chief of the Laboratory of Neural Control, National Institute of Neurological Disorders, National Institutes of Health, Bethesda, MD, USA Present address: P.O. Box 1722, El Prado, NM 87529,USA E-mail: [email protected] In 1906 Sir Charles Sherrington published The Integrative Action of the Nervous System, which was a collection of ten lectures delivered two years before at Yale University in the United States. In this monograph Sherrington summarized two decades of painstaking experimental observations and his incisive interpretation of them. It settled the then-current debate between the ‘‘Reticular Theory’’ versus ‘‘Neuron Doctrine’’ ideas about the fundamental nature of the nervous system in mammals in favor of the latter, and it changed forever the way in which subsequent generations have viewed the organization of the central nervous system. Sherrington’s magnum opus contains basic concepts and even terminology that are now second nature to every student of the subject. This brief article reviews the historical context in which the book was written, summarizes its content, and considers its impact on Neurology and Neuroscience. Keywords: Neuron Doctrine; spinal reflexes; reflex coordination; control of movement; nervous system organization Introduction The first decade of the 20th century saw two momentous The Silliman lectures events for science. The year 1905 was Albert Einstein’s Sherrington’s 1906 monograph, published simultaneously in ‘miraculous year’ during which three of his most celebrated London, New Haven and New York, was based on a series papers in theoretical physics appeared. -
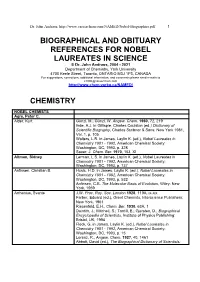
Biographical References for Nobel Laureates
Dr. John Andraos, http://www.careerchem.com/NAMED/Nobel-Biographies.pdf 1 BIOGRAPHICAL AND OBITUARY REFERENCES FOR NOBEL LAUREATES IN SCIENCE © Dr. John Andraos, 2004 - 2021 Department of Chemistry, York University 4700 Keele Street, Toronto, ONTARIO M3J 1P3, CANADA For suggestions, corrections, additional information, and comments please send e-mails to [email protected] http://www.chem.yorku.ca/NAMED/ CHEMISTRY NOBEL CHEMISTS Agre, Peter C. Alder, Kurt Günzl, M.; Günzl, W. Angew. Chem. 1960, 72, 219 Ihde, A.J. in Gillispie, Charles Coulston (ed.) Dictionary of Scientific Biography, Charles Scribner & Sons: New York 1981, Vol. 1, p. 105 Walters, L.R. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 328 Sauer, J. Chem. Ber. 1970, 103, XI Altman, Sidney Lerman, L.S. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 737 Anfinsen, Christian B. Husic, H.D. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 532 Anfinsen, C.B. The Molecular Basis of Evolution, Wiley: New York, 1959 Arrhenius, Svante J.W. Proc. Roy. Soc. London 1928, 119A, ix-xix Farber, Eduard (ed.), Great Chemists, Interscience Publishers: New York, 1961 Riesenfeld, E.H., Chem. Ber. 1930, 63A, 1 Daintith, J.; Mitchell, S.; Tootill, E.; Gjersten, D., Biographical Encyclopedia of Scientists, Institute of Physics Publishing: Bristol, UK, 1994 Fleck, G. in James, Laylin K. (ed.), Nobel Laureates in Chemistry 1901 - 1992, American Chemical Society: Washington, DC, 1993, p. 15 Lorenz, R., Angew. -

DMJ.1936.2.1.A02.Young.Pdf (3.644Mb)
DALHOUSIE MEDICAL JOURNAL 5 A Memorable Conference THE HARVARD TERCENTENARY 1636 - 1936 E. GORDON YOUNG, B.A., M.Sc., Ph.D., F.R.S.C. OMEONE has said that the most valuable and rarest thing in the world S is a new idea. It is the verdict or the intellectual world of science, of art and of music that progress centres largely about the thoughts ex pressed by the few great minds of the centuries. The work of the scientists of the world has been likened to a great canvas, the subject of which has been chosen by the few and the first bold lines inserted, but the great mass of colour and detail has been supplied by the many faithful apprentices. It was most fitting that the oldest and greatest of American Universities should celebrate its three hundredth birthday in an intellec tual feast and that it should invite to its table as leaders of conversation the greatest minds of the world in those subjects which were proposed for discussion. Harvard.!J.as a magnificent record of intellectual tolerance and its hospitality was open to individuals of all nationalities and all re- ligious and political creeds. To Cambridge thus in the early days of September, 1936, there came, by invitation, a group of about two thousand five hundred American and Canadian scholars to participate in a memorable series of symposia led by a special group of sixty-seven eminent scientists and men of letters from fifteen different countries. These included no fewer than eleven men who had the greatest single distinction in the realms of science and of letters, the Nobel Prize. -

Nobel Prizes
W W de Herder Heroes in endocrinology: 1–11 3:R94 Review Nobel Prizes Open Access Heroes in endocrinology: Nobel Prizes Correspondence Wouter W de Herder should be addressed to W W de Herder Section of Endocrinology, Department of Internal Medicine, Erasmus MC, ’s Gravendijkwal 230, 3015 CE Rotterdam, Email The Netherlands [email protected] Abstract The Nobel Prize in Physiology or Medicine was first awarded in 1901. Since then, the Nobel Key Words Prizes in Physiology or Medicine, Chemistry and Physics have been awarded to at least 33 " diabetes distinguished researchers who were directly or indirectly involved in research into the field " pituitary of endocrinology. This paper reflects on the life histories, careers and achievements of 11 of " thyroid them: Frederick G Banting, Roger Guillemin, Philip S Hench, Bernardo A Houssay, Edward " adrenal C Kendall, E Theodor Kocher, John J R Macleod, Tadeus Reichstein, Andrew V Schally, Earl " neuroendocrinology W Sutherland, Jr and Rosalyn Yalow. All were eminent scientists, distinguished lecturers and winners of many prizes and awards. Endocrine Connections (2014) 3, R94–R104 Introduction Endocrine Connections Among all the prizes awarded for life achievements in In 1901, the first prize was awarded to the German medical research, the Nobel Prize in Physiology or physiologist Emil A von Behring (3, 4). This award heralded Medicine is considered the most prestigious. the first recognition of extraordinary advances in medicine The Swedish chemist and engineer, Alfred Bernhard that has become the legacy of Nobel’s prescient idea to Nobel (1833–1896), is well known as the inventor of recognise global excellence. -

John Burchenal Oral History Interview
Joseph Burchenal Interview, January 26, 2001 1 National Cancer Institute Oral History Interview Project Interview with Joseph Burchenal Conducted on January 26, 2001 by Peggy Dillon Darien, Connecticut PD: Good morning. This is Peggy Dillon of History Associates Incorporated. I am speaking with Dr. Joseph Burchenal for the NCI oral history interview series. We are at his home in Darien, Connecticut. Today is January 26, 2001. JB: Good morning. PD: I would like to talk with you today about your work in cancer chemotherapy in general and also your involvement with the National Cancer Institute in particular. Before we get into your career overall and NCI, I'd like to ask you about your background. If you could just tell me a little bit about your upbringing and education . I understand that you were interested in chemistry from a very early age. JB: I was born in Milford, Delaware, but I lived in Wilmington, Delaware, for the first part of my life. My mother died when I was three, in childbirth. So I lived with my father in Wilmington. He was a lawyer. I went to school at Tower Hill School. The majority of my friends in the school had fathers or mothers–fathers mainly–who worked for Dupont. They were very likely to, so that there was a lot of interest in chemistry there. In fact, it was the same way on the street where we lived, where the fathers were mostly chemists. But my interest in chemistry, I guess, started when I was eight years old and I had a cousin who was eleven who was given a Chemcraft set and he used to show us all of the interesting things that he could do with it. -

Microorganisms: Friend and Foe : MCQ for VIII: Biology 1.The Yeast
Microorganisms: Friend and Foe : MCQ for VIII: Biology 1.The yeast multiply by a process called (a) Binary fission (b) Budding (c) Spore formation (d) None of the above 2.The example of protozoan is (a) Penicillium (b) Blue green algae (c) Amoeba (d) Bacillus 3.The most common carrier of communicable diseases is (a) Ant (b) Housefly (c) Dragonfly (d) Spider 4.The following is an antibiotics (a) Alcohol (b) Yeast (c) Sodium bicarbonate (d) Streptomycin 5.Yeast produces alcohol and carbon dioxide by a process called (a) Evaporation (b) Respiration (c) Fermentation (d) Digestion 6.The algae commonly used as fertilizers are called (a) Staphylococcus (b) Diatoms (c) Blue green algae (d) None of the above 7.Cholera is caused by (a) Bacteria (b) Virus (c) Protozoa (d) Fungi 8.Plant disease citrus canker is caused by (a) Virus (b) Fungi (c) Bacteria (d) None of these 9.The bread dough rises because of (a) Kneading (b) Heat (c) Grinding (d) Growth of yeast cells 10.Carrier of dengue virus is (a) House fly (b) Dragon fly (c) Female Aedes Mosquito (d) Butterfly 11. Yeast is used in the production of (a) Sugar (b) Alcohol (c) Hydrochloric acid (d) Oxygen 12. The vaccine for smallpox was discovered by (a) Robert Koch (b) Alexander Fleming (c) Sir Ronald Ross (d) Edward Jenner 13.Chickenpox is caused by (a) Virus (b) Fungi (c) Protozoa (d) Bacteria 14.The bacterium which promote the formation of curd (a) Rhizobium (b) Spirogyra (c) Breadmould (d) Lactobacillus 15.Plasmodium is a human parasite which causes (a) dysentery (b) Sleeping sickness (c) Malaria