Magnesium Sulfate for Neuroprotection Practice Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Magnesium Sulfate
MAGNESIUM SULFATE Prepared at the 68th JECFA (2007), published in FAO JECFA Monographs 4 (2007), superseding the specifications prepared at the 63rd JECFA (2004) and published the Combined Compendium of Food Additive Specifications, FAO JECFA Monographs 1 (2005). An ADI “not specified” was established at the 68th JECFA (2007). SYNONYMS Epsom salt (heptahydrate); INS No.518 DEFINITION Magnesium sulfate occurs naturally in sea water, mineral springs and in minerals such as kieserite and epsomite. It is recovered from them or by reacting sulfuric acid and magnesium oxide. It is produced with one or seven molecules of water of hydration or in a dried form containing the equivalent of between 2 and 3 waters of hydration. Chemical names Magnesium sulfate C.A.S. number Monohydrate: 14168-73-1 Heptahydrate: 10034-99-8 Dried: 15244-36-7 Chemical formula Monohydrate: MgSO4.H2O Heptahydrate: MgSO4.7H2O Dried: MgSO4.xH2O, where x is the average hydration value (between 2 and 3) Formula weight Monohydrate: 138.38 Heptahydrate: 246.47 Assay Not less than 99.0 % and not more than 100.5% on the ignited basis DESCRIPTION Colourless crystals, granular crystalline powder or white powder. Crystals effloresce in warm, dry air. FUNCTIONAL USES Nutrient; flavour enhancer; firming agent; and processing aid (fermentation aid in the production of beer and malt beverages) CHARACTERISTICS IDENTIFICATION Solubility (Vol. 4) Freely soluble in water, very soluble in boiling water, and sparingly soluble in ethanol. Test for magnesium (Vol. 4) Passes test Test for sulfate (Vol. 4) Passes test PURITY Loss on ignition (Vol. 4) Monohydrate: between 13.0 and 16.0 %, Heptahydrate: between 40.0 and 52.0 %, Dried: between 22.0 and 32.0 % (105°, 2h, then 400° to constant weight) pH (Vol. -

Mechanosynthesis of Magnesium and Calcium Salt?Urea Ionic Cocrystal
Letter pubs.acs.org/journal/ascecg Mechanosynthesis of Magnesium and Calcium Salt−Urea Ionic Cocrystal Fertilizer Materials for Improved Nitrogen Management Kenneth Honer, Eren Kalfaoglu, Carlos Pico, Jane McCann, and Jonas Baltrusaitis* Department of Chemical and Biomolecular Engineering, Lehigh University, B336 Iacocca Hall, 111 Research Drive, Bethlehem, Pennsylvania 18015, United States *S Supporting Information ABSTRACT: Only 47% of the total fertilizer nitrogen applied to the environment is taken up by the plants whereas approximately 40% of the total fertilizer nitrogen lost to the environment reverts back into unreactive atmospheric dinitrogen that greatly affects the global nitrogen cycle including increased energy consumption for NH3 synthesis, as well as accumulation of nitrates in drinking water. In this letter, we provide a mechanochemical method of inorganic magnesium and calcium salt−urea ionic cocrystal synthesis to obtain enhanced stability nitrogen fertilizers. The solvent-free mechanochemical synthesis presented can result in a greater manufacturing process sustainability by reducing or eliminating the need for solution handling and evaporation. NH3 emission testing suggests that urea ionic cocrystals are capable of decreasing NH3 emissions to the environment when compared to pure urea, thus providing implications for a sustainable global solution to the management of the nitrogen cycle. KEYWORDS: Fertilizers, Nitrogen, urea, Mechanochemistry, Cocrystal, pXRD, NH3 Emissions, Stability ■ INTRODUCTION ammonia as opposed to up to 61.1% of soil treated with urea 7,8 fi only, which suggests that major improvements to the global Atmospheric dinitrogen, N2, xation to synthesize ammonia, 9,10 ’ 1 nitrogen cycle are achievable. Additionally, urea molecular NH3, consumes more than 1% of the world s primary energy. -
The Importance of Minerals in the Long Term Health of Humans Philip H
The Importance of Minerals in the Long Term Health of Humans Philip H. Merrell, PhD Technical Market Manager, Jost Chemical Co. Calcium 20 Ca 40.078 Copper 29 Cu 63.546 Iron Magnesium 26 12 Fe Mg 55.845 24.305 Manganese Zinc 25 30 Mn Zn 55.938 65.380 Table of Contents Introduction, Discussion and General Information ..................................1 Calcium ......................................................................................................3 Copper .......................................................................................................7 Iron ...........................................................................................................10 Magnesium ..............................................................................................13 Manganese ..............................................................................................16 Zinc ..........................................................................................................19 Introduction Daily intakes of several minerals are necessary for the continued basic functioning of the human body. The minerals, Calcium (Ca), Iron (Fe), Copper (Cu), Magnesium (Mg), Manganese (Mn), and Zinc (Zn) are known to be necessary for proper function and growth of the many systems in the human body and thus contribute to the overall health of the individual. There are several other trace minerals requirements. Minimum (and in some cases maximum) daily amounts for each of these minerals have been established by the Institute of -

Sulfate Resistance Study of Carbonated Low-Calcium Silicate Systems
Sixth International Conference on Durability of Concrete Structures Paper Number PSE12 18 - 20 July 2018 University of Leeds, Leeds, West Yorkshire, LS2 9JT, United Kingdom Sulfate Resistance Study of Carbonated Low-Calcium Silicate Systems R. Tokpatayeva and J. Olek Lyles School of Civil Engineering, Purdue University, West Lafayette, IN, USA J. Jain, A. Seth and N. DeCristofaro Solidia Technologies Inc., Piscataway, NJ, USA ABSTRACT This paper summarizes the results of sulfate resistance study of carbonated mortar specimens made with Solidia Cement (SC) and tested for expansion according to ASTM C1012 specification while exposed to three types of soak solutions: sodium sulfate, magnesium sulfate and deionized water. A control set of ordinary portland cement (OPC) mortars was also evaluated. Besides the length change measurements, visual observations of changes in the appearance of specimens were conducted after various lengths of exposure. In addition, microstructural characterization of the specimens was conducted using scanning electron microscopy (SEM), X-ray diffraction (XRD) and thermo-gravimetric analysis (TGA) techniques. Finally, changes in the concentration of the chemical species present in the soak solutions in contact with the SC specimens were evaluated using both, the ion chromatography (IC) and the inductively coupled plasma optical emission spectrometry (ICP-OES). As expected, the OPC mortar specimens started deteriorating early and reached the critical (i.e.0.1%) level of expansion in about 4 months in case of sodium sulfate solution and in about 6 months in case of magnesium sulfate solution. With respect to the SC mortar specimens, those exposed to magnesium sulfate solution showed higher expansion than those exposed to sodium sulfate solution. -

Managing Ferret Toxicoses J
CLINICIAN’S NOTEBOOK Managing Ferret Toxicoses J. RICHARDSON AND R. BALABUSZKO Jill A. Richardson, DVM, Dipl ACFE ASPCA National Animal Poison Control Center 1717 South Philo Road Suite 36 Urbana, Illinois 61802 [email protected] FERRETS ARE EXTREMELY CURIOUS and adept at accessing areas where PRACTICE TIP baits, cleaners, chemicals and medica- Rachel A. Balabuszko, CVT tions are stored. Ferrets can even pry ASPCA National Animal Poison caps from child-resistant bottles or Control Center chew through heavy plastic contain- ers. Products such as antifreeze, Dr. Jill A. Richardson received her DVM flavored medications or pest control degree from Tuskegee University in baits have an appealing taste. Because 1994. In 1996, following experience in the average weight of the adult ferret small animal practices in Tennessee and is less than 2 kg, even small amounts in West Virginia, Dr. Richardson joined of toxins can be dangerous when the ASPCA National Animal Poison ingested. Therefore, prompt treatment Control Center as a Veterinary Poison of toxicoses is essential. Information Specialist. Rachel Balabuszko, CVT, joined the In cases of oral exposure, ferrets have ASPCA National Animal Poison Control the ability to vomit. However, the Center as a Certified Veterinary length of time since ingestion of the Ferrets can be restrained by scruffing Technician in 1998, after receiving her toxicant, the ferret’s age, its previous the loose skin on the back of the neck. associate degree in veterinary technol- medical history, and the type of ogy from Parkland College. poison ingested all affect the decision to induce emesis. Tom Schaefges Photography Sidney, Illinois [email protected] EXOTIC DVM VOLUME 2.4 2000 23 CLINICIAN’S NOTEBOOK STEPS IN MANAGING FERRET TOXICOSES START ASSESS THE SITUATION STABILIZE THE FERRET ✖ Is the ferret seizuring? ✖ Administer oxygen if necessary ✖ Is the ferret breathing? ✖ Control seizures ✖ What is the heart rate? ✖ Correct any cardiovascular ✖ What color are the mucous abnormality membranes? Table 1. -
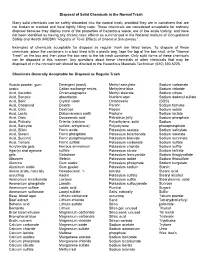
Disposal of Solid Chemicals in the Normal Trash
Disposal of Solid Chemicals in the Normal Trash Many solid chemicals can be safety discarded into the normal trash, provided they are in containers that are not broken or cracked and have tightly fitting caps. These chemicals are considered acceptable for ordinary disposal because they display none of the properties of hazardous waste, are of low acute toxicity, and have not been identified as having any chronic toxic effects as summarized in the National Institute of Occupational Safety and Health (NIOSH) “Registry of Toxic Effects of Chemical Substances”. Examples of chemicals acceptable for disposal as regular trash are listed below. To dispose of these chemicals, place the containers in a box lined with a plastic bag, tape the top of the box shut, write “Normal Trash” on the box and then place the box next to the lab trash container. Only solid forms of these chemicals can be disposed in this manner. Any questions about these chemicals or other chemicals that may be disposed of in the normal trash should be directed to the Hazardous Materials Technician (610) 330-5225. Chemicals Generally Acceptable for Disposal as Regular Trash Acacia powder, gum Detergent (most) Methyl salicylate Sodium carbonate arabic Cation exchange resins Methylene blue Sodium chloride Acid, Ascorbic Chromatographic Methyl stearate Sodium citrate Acid, Benzoic absorbents Nutrient agar Sodium dodecyl sulfate Acid, Boric Crystal violet Octacosane (SDS) Acid, Casamind Dextrin Parafin Sodium formate Acid, Citric Dextrose Pepsin Sodium iodide Acid, Lactic Diatomaceous -

Calcium Gluconate
CALCIUM GLUCONATE CLASSIFICATION Minerals and electrolytes TRADE NAME(S) Calcium Gluconate 10% (for IV use) Calcium Gluconate gel 2.5% (for topical use) DESIRED EFFECTS Lower potassium levels; pain relief and neutralizing fluoride ion MECHANISM OF ACTION Calcium is the primary component of skeletal tissue. Bone serves as a calcium depot and as a reservoir for electrolytes and buffers. INDICATIONS Suspected hyperkalemia in adult PEA/Asystole Antidote for calcium channel blocker overdose and magnesium sulfate toxicity Gel is used for hydrofluoric acid burns Suspected hyperkalemia with adult crush injury or peaked T-waves on EKG CONTRAINDICATIONS Should not be given to patients with digitalis toxicity Should be used with caution in patients with dehydration ADVERSE REACTIONS When given too rapidly or to someone on digitalis, can cause sudden death from ventricular fibrillation May cause mild to severe IV site irritation SPECIAL CONSIDERATIONS Must either use a different IV line or flush line with copious normal saline if being given with sodium bicarbonate. When used on hydroflouric acid burns, relief of pain is the only indication of treatment efficacy. Therefore, use of analgesic agents is not recommended. DOSING REGIMEN Suspected hyperkalemia in adult PEA/asystole or adult crush injury, or evidence of EKG changes (Ex. peaked T-waves) o Calcium gluconate 10% 15-30 ml IV/IO over 2-5 minutes KNOWN calcium channel blocker overdose - administer 3 grams IV/IO may repeat dose in 10 minutes if no effect. Hydrofluoric acid burns apply calcium gluconate gel 2.5% every 15 minutes to burned area and massage continuously until pain disappears. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Magnesium Sulfate
MODULE III MAGNESIUM SULFATE Manual for Procurement & Supply of Quality-Assured MNCH Commodities MAGNESIUM SULFATE INJECTION, 500 MG/ML IN 2-ML AND 10-ML AMPOULE GENERAL PRODUCT INFORMATION Pre-eclampsia and eclampsia is the second-leading cause of maternal death in low- and middle-income countries. It is most often detected through the elevation of blood pressure during pregnancy, which can be followed by seizures, kidney and liver damage, and maternal and fetal death, if untreated. Magnesium sulfate is recognized by WHO as the safest, most effective, and lowest-cost medicine for treating pre-eclampsia and eclampsia. It is also considered an essential medicine by the UN Commission on Life-Saving Commodities for Women and Children. Other anticonvulsant medicines, such as diazepam and phenytoin, are less effective and riskier. Magnesium sulfate should be the sole first-line treatment of pre-eclampsia and eclampsia that should be procured over other anticonvulsants and made available in all health facilities to help lower maternal death rates and improve overall maternal health. MSꟷ1 | Manual for Procurement & Supply of Quality-Assured MNCH Commodities Magnesium Sulfate KEY CONSIDERATIONS IN PROCUREMENT Procurement should be made from trusted sources. This includes manufacturers prequalified by WHO or approved by a SRA for magnesium sulfate injection and 1. those with a proven record of quality products. Procurers need to focus on product quality to ensure that it is sterile and safe for patient use as magnesium sulfate is an injectable medicine. 2. KEY QUALITY CONSIDERATIONS Product specification Products that are procured must comply with pharmacopoeial specifications, such as those of the International Pharmacopoeia, US Pharmacopoeia, and British Pharmacopoeia, as detailed in the “Supply” section 4 below. -

Magnesium for Constipation
Magnesium for Constipation What is Magnesium Oxide? Magnesium is a mineral that the body uses to keep the organs functioning, particularly the kidneys, heart, and muscles. Magnesium can be obtained from foods such as green vegetables, nuts, and whole grain products. Though most people maintain adequate magnesium levels on their own, some disorders can lower magnesium levels, such as gastrointestinal disorders like Irritable Bowel Syndrome (IBS). Magnesium helps to increase the amount of water in the intestines, which can help with bowel movements. It may be used as a laxative due to these properties, or as a supplement for magnesium deficiency. What is the dose amount? The maximum dose for Magnesium is 2 grams or 2000 milligrams. You should not take more than 4 tablets or capsules in one day. Magnesium comes in tablets and capsules (500 mg): take orally as directed by your doctor and take with a full 8-ounce glass of liquid. One Tablespoon of Milk of Magnesium is equal to 500 mg. Tablets/Caplets may be taken all at bedtime or separately throughout the day. Side Effects There can be many side effects related to the intake of oral Magnesium. Some of the frequent side effects include diarrhea. You should notify your doctor immediately if you have any of the following severe side effects: black, tarry stools nausea Michigan Bowel Control Program - 1 - slow reflexes vomit that looks like coffee grounds Where can I purchase Magnesium? You can find Magnesium over the counter at most stores that sell supplements and at pharmacies. It typically costs $5 for a 100-count bottle. -

Plant Health Solutions
Plant Health Solutions NUTRITION PORTFOLIO ■ Foliar Nutrients ■ Chelated Nutrients ■ Complexed Nutrients ■ Nutrient Efficiency Enhancers ■ Botanical Blends ■ Humic Acids About BRANDT ® BRANDT is a privately owned U.S. manufacturer and leading supplier of specialty inputs for the agriculture, turf, ornamental, and lawn and garden markets. BRANDT has one of the largest portfolios of micronutrients and OMRI Listed products available today. Its products are used on some of the world’s most notable farms, vineyards and orchards. Contact Us 800 300 6559 [email protected] Visit us online at: www.BRANDT.co 2 Contents Foliar Nutrients . 4 Chelated Nutrients . 8 Complexed Nutrients . 10 Nutrient Efficiency Enhancers. 14 Botanical Blends. 17 Humic Acid Soil Amendments . 18 Not all products are registered for sale in every country and all 50 U.S. states. Please check label for use and contact your BRANDT representative with any questions. 3 Foliar Nutrients BRANDT Smart System BRANDT Manni-Plex 4 BRANDT Smart System® Advanced Compatibility Foliar Nutrition Smarter Foliar Nutrient Delivery BRANDT Smart System foliar nutrients were designed for use in tank mix environments where compatibility concerns may have previously been a challenge. The proprietary formulations provide supplemental secondary and micronutrients to plant growing points quickly and effectively, and may be used in a wide range of tank mix solutions. BRANDT Smart System is an excellent option for in-season nutrient enhancement and replenishment and optimal plant health. Key Advantages -

Therapeutic Uses of Magnesium MARY P
COMPLEMENTARY AND ALTERNATIVE MEDICINE Therapeutic Uses of Magnesium MARY P. GUERRERA, MD, University of Connecticut School of Medicine, Farmington, Connecticut STELLA LUCIA VOLPE, P,hD University of Pennsylvania School of Nursing, Philadelphia, Pennsylvania JUN JAMES MAO, MD, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania Magnesium is an essential mineral for optimal metabolic function. Research has shown that the mineral content of magnesium in food sources is declining, and that magnesium depletion has been detected in persons with some chronic diseases. This has led to an increased awareness of proper magnesium intake and its potential therapeutic role in a number of medical conditions. Studies have shown the effectiveness of magnesium in eclampsia and preeclampsia, arrhythmia, severe asthma, and migraine. Other areas that have shown promising results include lowering the risk of metabolic syndrome, improving glucose and insulin metabolism, relieving symptoms of dysmenorrhea, and alleviat- ing leg cramps in women who are pregnant. The use of magnesium for constipation and dyspepsia are accepted as standard care despite limited evidence. Although it is safe in selected patients at appropriate dosages, magnesium may cause adverse effects or death at high dosages. Because magnesium is excreted renally, it should be used with caution in patients with kidney disease. Food sources of magnesium include green leafy vegetables, nuts, legumes, and whole grains. (Am Fam Physician. 2009;80(2):157-162. Copyright © 2009 American Academy of Family Physicians.) agnesium is the fourth most use (e.g., diuretics, antibiotics); alcoholism; abundant essential mineral and older age (e.g., decreased absorption of in the body. It is distributed magnesium, increased renal exertion).1 approximately one half in the There are challenges in diagnosing mag- Mbone and one half in the muscle and other nesium deficiency because of its distribution soft tissues; less than one percent is in the in the body.