And Prevention of New World Hantaviruses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABSTRACT Vector-Borne Viral Infections in South-West
저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다. l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer August 2016 Master’s Degree Thesis Vector-Borne Viral Infections in South-West Region of Korea Graduate School of Chosun University Department of Biomedical Sciences Babita Jha August 2016 Master’s Degree Thesis Vector-Borne Viral Infections in South-West Region of Korea Graduate School of Chosun University Department of Biomedical Sciences Babita Jha Vector-Borne Viral Infections in South-West Region of Korea 한국의 남서부 지역에서 매개체 관련 바이러스 질환 August, 2016 Graduate School of Chosun University Department of Biomedical Sciences Babita Jha Vector-Borne Viral Infections in South-West Region of Korea Advisor: Prof. Dong-Min Kim, MD, PhD THESIS SUBMITTED TO THE DEPARTMENT OF BIOMEDICAL SCIENCES, CHOSUN UNIVERSITY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF BIOMEDICAL SCIENCES April, 2016 Graduate School of Chosun University Department of Biomedical Sciences Submitted by Babita Jha August Master’s Vector-Borne Viral Infections in Babita Jha Degree 2016 Thesis South-West Region of Korea Table of Contents LIST OF TABLES……………………….................iv LIST OF FIGURES…………………………………v ABBREVIATIONS AND SYMBOLS…………….vi ABSTRACT…………………………………...…….ix 한 글 요 약……………………………………...…..xii I. -

Hantavirus Disease Were HPS Is More Common in Late Spring and Early Summer in Seropositive in One Study in the U.K
Hantavirus Importance Hantaviruses are a large group of viruses that circulate asymptomatically in Disease rodents, insectivores and bats, but sometimes cause illnesses in humans. Some of these agents can occur in laboratory rodents or pet rats. Clinical cases in humans vary in Hantavirus Fever, severity: some hantaviruses tend to cause mild disease, typically with complete recovery; others frequently cause serious illnesses with case fatality rates of 30% or Hemorrhagic Fever with Renal higher. Hantavirus infections in people are fairly common in parts of Asia, Europe and Syndrome (HFRS), Nephropathia South America, but they seem to be less frequent in North America. Hantaviruses may Epidemica (NE), Hantavirus occasionally infect animals other than their usual hosts; however, there is currently no Pulmonary Syndrome (HPS), evidence that they cause any illnesses in these animals, with the possible exception of Hantavirus Cardiopulmonary nonhuman primates. Syndrome, Hemorrhagic Nephrosonephritis, Epidemic Etiology Hemorrhagic Fever, Korean Hantaviruses are members of the genus Orthohantavirus in the family Hantaviridae Hemorrhagic Fever and order Bunyavirales. As of 2017, 41 species of hantaviruses had officially accepted names, but there is ongoing debate about which viruses should be considered discrete species, and additional viruses have been discovered but not yet classified. Different Last Updated: September 2018 viruses tend to be associated with the two major clinical syndromes in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary (or cardiopulmonary) syndrome (HPS). However, this distinction is not absolute: viruses that are usually associated with HFRS have been infrequently linked to HPS and vice versa. A mild form of HFRS in Europe is commonly called nephropathia epidemica. -

Molecular Phylogeny of Mobatviruses (Hantaviridae) in Myanmar and Vietnam
viruses Article Molecular Phylogeny of Mobatviruses (Hantaviridae) in Myanmar and Vietnam Satoru Arai 1, Fuka Kikuchi 1,2, Saw Bawm 3 , Nguyễn Trường Sơn 4,5, Kyaw San Lin 6, Vương Tân Tú 4,5, Keita Aoki 1,7, Kimiyuki Tsuchiya 8, Keiko Tanaka-Taya 1, Shigeru Morikawa 9, Kazunori Oishi 1 and Richard Yanagihara 10,* 1 Infectious Disease Surveillance Center, National Institute of Infectious Diseases, Tokyo 162-8640, Japan; [email protected] (S.A.); [email protected] (F.K.); [email protected] (K.A.); [email protected] (K.T.-T.); [email protected] (K.O.) 2 Department of Chemistry, Faculty of Science, Tokyo University of Science, Tokyo 162-8601, Japan 3 Department of Pharmacology and Parasitology, University of Veterinary Science, Yezin, Nay Pyi Taw 15013, Myanmar; [email protected] 4 Institute of Ecology and Biological Resources, Vietnam Academy of Science and Technology, Hanoi, Vietnam; [email protected] (N.T.S.); [email protected] (V.T.T.) 5 Graduate University of Science and Technology, Vietnam Academy of Science and Technology, Hanoi, Vietnam 6 Department of Aquaculture and Aquatic Disease, University of Veterinary Science, Yezin, Nay Pyi Taw 15013, Myanmar; [email protected] 7 Department of Liberal Arts, Faculty of Science, Tokyo University of Science, Tokyo 162-8601, Japan 8 Laboratory of Bioresources, Applied Biology Co., Ltd., Tokyo 107-0062, Japan; [email protected] 9 Department of Veterinary Science, National Institute of Infectious Diseases, Tokyo 162-8640, Japan; [email protected] 10 Pacific Center for Emerging Infectious Diseases Research, John A. -

COMENIUS UNIVERSITY in BRATISLAVA Faculty of Natural Sciences
COMENIUS UNIVERSITY IN BRATISLAVA Faculty of Natural Sciences UNIVERSITY OF CAGLIARI Department of Biomedical Sciences MOLECULAR EPIDEMIOLOGY OF HANTAVIRUSES IN CENTRAL EUROPE AND ANTIVIRAL SCREENING AGAINST ZOONOTIC VIRUSES CAUSING HEMORRHAGIC FEVERS DISSERTATION 2017 RNDr. PaedDr. Róbert SZABÓ COMENIUS UNIVERSITY IN BRATISLAVA Faculty of Natural Sciences UNIVERSITY OF CAGLIARI Department of Biomedical Sciences MOLECULAR EPIDEMIOLOGY OF HANTAVIRUSES IN CENTRAL EUROPE AND ANTIVIRAL SCREENING AGAINST ZOONOTIC VIRUSES CAUSING HEMORRHAGIC FEVERS Dissertation Study program: Virology Molecular and Translational Medicine Field of Study: Virology Place of the study: Biomedical Research Center, SAS in Bratislava, Slovakia Department of Biomedical Sciences, Cittadella Universitaria, Monserrato, Italy Supervisors: RNDr. Boris Klempa, DrSc. Prof. Alessandra Pani Bratislava, 2017 RNDr. PaedDr. Róbert SZABÓ 25276874 Univerzita Komenského v Bratislave Prírodovedecká fakulta ZADANIE ZÁVEREČNEJ PRÁCE Meno a priezvisko študenta: RNDr. PaedDr. Róbert Szabó Študijný program: virológia (Jednoodborové štúdium, doktorandské III. st., denná forma) Študijný odbor: virológia Typ záverečnej práce: dizertačná Jazyk záverečnej práce: anglický Sekundárny jazyk: slovenský Názov: Molecular epidemiology of hantaviruses in Central Europe and antiviral screening against zoonotic viruses causing hemorrhagic fevers Molekulárna epidemiológia hantavírusov v strednej Európe a antivírusový skríning proti zoonotickým vírusom spôsobujúcim hemoragické horúčky Cieľ: Main objectives -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Immunogenicity and Serological Applications of Flavivirus Ed Iii Proteins and Multiplex Rt-Pcr for Detecting Novel Southern African Viruses
IMMUNOGENICITY AND SEROLOGICAL APPLICATIONS OF FLAVIVIRUS ED III PROTEINS AND MULTIPLEX RT-PCR FOR DETECTING NOVEL SOUTHERN AFRICAN VIRUSES Lehlohonolo Mathengtheng Thesis submitted in fulfillment of the requirements for the degree Ph.D Virology in the Department of Medical Microbiology and Virology, Faculty of Health Sciences, University of the Free State, Bloemfontein Promotor: Prof Felicity Burt, Department of Medical Microbiology and Virology, Faculty of Health Sciences, University of the Free State, Bloemfontein January 2015 Table of contents Table of contents ................................................................................................................................................. 2 Declaration ............................................................................................................................................................ i Acknowledgements .............................................................................................................................................. ii Financial Support ................................................................................................................................................ iii Lehlohonolo Mathengtheng, An Obituary ........................................................................................................... v Publications and presentations........................................................................................................................... vii List of figures ....................................................................................................................................................... -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -

Taxonomy of the Order Bunyavirales: Second Update 2018
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Arch Virol Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 March 01. Published in final edited form as: Arch Virol. 2019 March ; 164(3): 927–941. doi:10.1007/s00705-018-04127-3. TAXONOMY OF THE ORDER BUNYAVIRALES: SECOND UPDATE 2018 A full list of authors and affiliations appears at the end of the article. Abstract In October 2018, the order Bunyavirales was amended by inclusion of the family Arenaviridae, abolishment of three families, creation of three new families, 19 new genera, and 14 new species, and renaming of three genera and 22 species. This article presents the updated taxonomy of the order Bunyavirales as now accepted by the International Committee on Taxonomy of Viruses (ICTV). Keywords Arenaviridae; arenavirid; arenavirus; bunyavirad; Bunyavirales; bunyavirid; Bunyaviridae; bunyavirus; emaravirus; Feraviridae; feravirid, feravirus; fimovirid; Fimoviridae; fimovirus; goukovirus; hantavirid; Hantaviridae; hantavirus; hartmanivirus; herbevirus; ICTV; International Committee on Taxonomy of Viruses; jonvirid; Jonviridae; jonvirus; mammarenavirus; nairovirid; Nairoviridae; nairovirus; orthobunyavirus; orthoferavirus; orthohantavirus; orthojonvirus; orthonairovirus; orthophasmavirus; orthotospovirus; peribunyavirid; Peribunyaviridae; peribunyavirus; phasmavirid; phasivirus; Phasmaviridae; phasmavirus; phenuivirid; Phenuiviridae; phenuivirus; phlebovirus; reptarenavirus; tenuivirus; tospovirid; Tospoviridae; tospovirus; virus classification; virus nomenclature; virus taxonomy INTRODUCTION The virus order Bunyavirales was established in 2017 to accommodate related viruses with segmented, linear, single-stranded, negative-sense or ambisense RNA genomes classified into 9 families [2]. Here we present the changes that were proposed via an official ICTV taxonomic proposal (TaxoProp 2017.012M.A.v1.Bunyavirales_rev) at http:// www.ictvonline.org/ in 2017 and were accepted by the ICTV Executive Committee (EC) in [email protected]. -
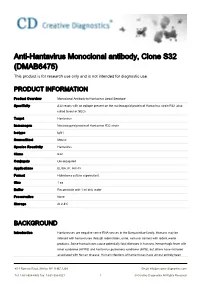
Anti-Hantavirus Monoclonal Antibody, Clone S32 (DMAB6475) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-Hantavirus Monoclonal antibody, Clone S32 (DMAB6475) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Monoclonal Antibody to Hantavirus Seoul Serotype Specificity S32 reacts with an epitope present on the nucleocapsid protein of Hantavirus strain R22 (also called Seoul or SEO) Target Hantavirus Immunogen Nucleocapsid protein of Hantavirus R22 strain Isotype IgG1 Source/Host Mouse Species Reactivity Hantavirus Clone S32 Conjugate Unconjugated Applications ELISA, IF, IHC-Fr Format Hybridoma culture supernatant Size 1 ea Buffer Reconstitute with 1 ml dist. water Preservative None Storage At 2-8℃ BACKGROUND Introduction Hantaviruses are negative sense RNA viruses in the Bunyaviridae family. Humans may be infected with hantaviruses through rodent bites, urine, saliva or contact with rodent waste products. Some hantaviruses cause potentially fatal diseases in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS), but others have not been associated with human disease. Human infections of hantaviruses have almost entirely been 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved linked to human contact with rodent excrement, but recent human-to-human transmission has been reported with the Andes virus in South America. The name hantavirus is derived from the Hantan River area in South Korea, which provided the founding member of the group: Hantaan virus (HTNV), isolated in the late 1970s by Ho-Wang Lee and colleagues. HTNV is one of several hantaviruses that cause HFRS, formerly known as Korean hemorrhagic fever. -

Zoonotické Viry U Volně Žijících Endotermních Obratlovců
MASARYKOVA UNIVERZITA PŘÍRODOVĚDECKÁ FAKULTA Ústav experimentální biologie Oddělení mikrobiologie a molekulární biotechnologie Zoonotické viry u volně žijících endotermních obratlovců Dizertační práce Brno 2017 Petra Straková MASARYKOVA UNIVERZITA PŘÍRODOVĚDECKÁ FAKULTA Ústav experimentální biologie Oddělení mikrobiologie a molekulární biotechnologie Zoonotické viry u volně žijících endotermních obratlovců Dizertační práce Petra Straková Školitel: prof. RNDr. Zdeněk Hubálek, DrSc. Brno 2017 Bibliografický záznam Autor: Mgr. Petra Straková Ústav biologie obratlovců AV ČR v.v.i., Brno - detašované pracoviště Valtice a Ústav experimentální biologie, PřF MU, Brno Název práce: Zoonotické viry u volně žijících endotermních obratlovců Studijní program: Biologie Studijní obor: Mikrobiologie Školitel: prof. RNDr. Zdeněk Hubálek, DrSc. Ústav biologie obratlovců AV ČR v.v.i., Brno - detašované pracoviště Valtice a Ústav experimentální biologie, PřF MU, Brno Valtice Akademický rok: 2016/2017 Počet stran: 155 + publikace Klíčová slova: emergentní zoonózy, hantaviry, flaviviry, virus západonilské horečky, virus Usutu, virus hepatitidy E, Česká republika, Evropa Bibliographic entry Author: Mgr. Petra Straková Institute of Vertebrate Biology of the Czech Academy of Sciences, Brno – laboratory Valtice, and Department of Experimental Biology, Faculty of Science, Masaryk University, Brno Title of Dissertation: Zoonotic viruses associated with free-living endotherm vertebrates Degree Programme: Biology Field of Study: Microbiology Supervisor: prof. RNDr. -

Viruses 2014, 6, 1112-1134; Doi:10.3390/V6031112 OPEN ACCESS
Viruses 2014, 6, 1112-1134; doi:10.3390/v6031112 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Article Changes in Diversification Patterns and Signatures of Selection during the Evolution of Murinae-Associated Hantaviruses Guillaume Castel *, Maria Razzauti, Emmanuelle Jousselin, Gael J. Kergoat and Jean-François Cosson INRA, UMR 1062 CBGP (INRA, IRD, Cirad, Montpellier SupAgro), Campus de Baillarguet, 34988 Montferrier-sur-Lez, France; E-Mails: [email protected] (M.R.); [email protected] (E.J.); [email protected] (G.J.K.); [email protected] (J.F.C.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +33-499-623-311; Fax: +33-499-623-345. Received: 29 November 2013; in revised form: 19 February 2014 / Accepted: 24 February 2014 / Published: 10 March 2014 Abstract: In the last 50 years, hantaviruses have significantly affected public health worldwide, but the exact extent of the distribution of hantavirus diseases, species and lineages and the risk of their emergence into new geographic areas are still poorly known. In particular, the determinants of molecular evolution of hantaviruses circulating in different geographical areas or different host species are poorly documented. Yet, this understanding is essential for the establishment of more accurate scenarios of hantavirus emergence under different climatic and environmental constraints. In this study, we focused on Murinae-associated hantaviruses (mainly Seoul Dobrava and Hantaan virus) using sequences available in GenBank and conducted several complementary phylogenetic inferences. We sought for signatures of selection and changes in patterns and rates of diversification in order to characterize hantaviruses’ molecular evolution at different geographical scales (global and local). -

Aus Dem Institut Für Medizinische Virologie Der Medizinischen Fakultät Charité – Universitätsmedizin Berlin
Aus dem Institut für medizinische Virologie der Medizinischen Fakultät Charité – Universitätsmedizin Berlin DISSERTATION Genetic reassortment between members of different Dobrava-Belgrade virus lineages and allocation of innate immune response modulation to particular genome segments zur Erlangung des akademischen Grades Doctor rerum medicarum (Dr. rer. medic.) vorgelegt der Medizinischen Fakultät Charité – Universitätsmedizin Berlin von Sina Kirsanovs aus Bremen Gutachter/in: 1. Prof. Dr. med. D. H. Krüger 2. Prof. Dr. med. H.-W. Presber 3. Priv.-Doz. Dr. R. Ulrich Datum der Promotion: 03.09.2010 Abstract Hantaviruses possess a tri-segmented negative-stranded RNA genome with the potency of genetic reassortment. Reassortment processes between genome segments might cause dramatic changes in the virulence of viruses as has been shown for influenza viruses. The European Dobrava-Belgrade virus species (DOBV) forms distinct lineages associated with different Apodemus mice species and can cause hemorrhagic fever with renal syndrome of different clinical severities. In this study, virological and molecular tools to monitor RNA reassortment in cell culture between two genetic lineages of DOBV were established. Representatives of the DOBV-Af (associated with A. flavicollis) and DOBV-Aa (associated with A. agrarius) lineages were used for dual infection of Vero E6 cells. Two hundred and seven individual virus clones were isolated and screened for reassortment by a newly established strain- and segment-specific multiplex PCR (MP-PCR). After co-infection, as much as 31% of virus progeny population was represented by genetically stable reassortants. Reassortment was proven by sequence analyses of the complete S and M segments as well as L-ORF. Two stable reassortment patterns where identified.