One Target, Different Effects: a Comparison of Distinct Therapeutic Antibodies Against the Same Targets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Activity of Rituximab and Ofatumumab Against Mantle
ACTIVITY OF RITUXIMAB AND OFATUMUMAB AGAINST MANTLE CELL LYMPHOMA(MCL) IN VITRO IN MCL CELL LINES BY COMPLEMENT DEPENDENT CYTOTOXICITY (CDC)AND ANTIBODY-DEPENDENT CELL MEDIATED CYTOTOXICITY ASSAYS(ADCC) Dr. Gopichand Pendurti M.B.B.S Mentor: Dr. Francisco J. Hernandez-Ilizaliturri MD Overview of presentation •Introduction to mantle cell lymphoma. •Concept of minimal residual disease. •Anti CD 20 antibodies. •51Cr release assays. •Flow cytometry on cell lines. •Results. •Future. MANTLE CELL LYMPHOMA •Mantle cell lymphoma is characterized by abnormal proliferation of mature B lymphocytes derived from naïve B cells. •Constitutes about 5% of all patients with Non Hodgkin's lymphoma. •Predominantly in males with M:F ratio 2.7:1 with onset at advanced age (median age 60yrs). •It is an aggressive lymphoma with median survival of patients being 3-4 years. •Often presents as stage III-IV with lymphadenopathy, hepatosplenomegaly, gastrointestinal involvement, peripheral blood involvement. Pedro Jares, Dolors Colomer and Elias Campo Genetic and molecular pathogenesis of mantle cell lymphoma: perspectives for new targeted therapeutics Nature revision of cancer 2007 October:7(10):750-62 •Genetic hallmark is t(11:14)(q13:q32) translocation leading to over expression of cyclin D1 which has one of the important pathogenetic role in deregulating the cell cycle. •Other pathogentic mechanisms include molecular and chromosomal alterations that Target proteins that regulate the cell cycle and senecense (BMI1,INK4a,ARF,CDK4 AND RB1). Interfere with cellular -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

Nimotuzumab, an Antitumor Antibody That Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding While Permitting the Active Receptor Conformation
Published OnlineFirst July 7, 2009; DOI: 10.1158/0008-5472.CAN-08-4518 Experimental Therapeutics, Molecular Targets, and Chemical Biology Nimotuzumab, an Antitumor Antibody that Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding while Permitting the Active Receptor Conformation Ariel Talavera,1,2 Rosmarie Friemann,2,3 Silvia Go´mez-Puerta,1 Carlos Martinez-Fleites,4 Greta Garrido,1 Ailem Rabasa,1 Alejandro Lo´pez-Requena,1 Amaury Pupo,1 Rune F. Johansen,3 Oliberto Sa´nchez,5 Ute Krengel,2 and Ernesto Moreno1 1Center of Molecular Immunology, Havana, Cuba; 2Department of Chemistry, University of Oslo, Oslo, Norway; and 3Center for Molecular and Behavioral Neuroscience, Institute of Medical Microbiology, University of Oslo, Rikshospitalet HF, Oslo, Norway; 4Department of Chemistry, University of York, Heslington, York, United Kingdom; and 5Center for Genetic Engineering and Biotechnology, Havana, Cuba Abstract region of the EGFR (eEGFR), leaving the dimerization ‘‘arm’’ in Overexpression of the epidermal growth factor (EGF) receptor domain II ready for binding a second monomer (4, 5). It has been (EGFR) in cancer cells correlates with tumor malignancy and shown that the eEGFR adopts a ‘‘tethered’’ or inactive conformation poor prognosis for cancer patients. For this reason, the EGFR in the absence of EGF (6). In this characteristic conformation, has become one of the main targets of anticancer therapies. the dimerization arm is hidden by interactions with domain IV, Structural data obtained in the last few years have revealed whereas domains I and III remain separated. Thus, to adopt the the molecular mechanism for ligand-induced EGFR dimeriza- ‘‘extended’’ or active conformation observed in the crystal structure tion and subsequent signal transduction, and also how this of the complex with EGF (4), the receptor must undergo a major signal is blocked by either monoclonal antibodies or small conformational change that brings together domains I and III (6). -

Targeted and Novel Therapy in Advanced Gastric Cancer Julie H
Selim et al. Exp Hematol Oncol (2019) 8:25 https://doi.org/10.1186/s40164-019-0149-6 Experimental Hematology & Oncology REVIEW Open Access Targeted and novel therapy in advanced gastric cancer Julie H. Selim1 , Shagufta Shaheen2 , Wei‑Chun Sheu3 and Chung‑Tsen Hsueh4* Abstract The systemic treatment options for advanced gastric cancer (GC) have evolved rapidly in recent years. We have reviewed the recent data of clinical trial incorporating targeted agents, including inhibitors of angiogenesis, human epidermal growth factor receptor 2 (HER2), mesenchymal–epithelial transition, epidermal growth factor receptor, mammalian target of rapamycin, claudin‑18.2, programmed death‑1 and DNA. Addition of trastuzumab to platinum‑ based chemotherapy has become standard of care as front‑line therapy in advanced GC overexpressing HER2. In the second‑line setting, ramucirumab with paclitaxel signifcantly improves overall survival compared to paclitaxel alone. For patients with refractory disease, apatinib, nivolumab, ramucirumab and TAS‑102 have demonstrated single‑agent activity with improved overall survival compared to placebo alone. Pembrolizumab has demonstrated more than 50% response rate in microsatellite instability‑high tumors, 15% response rate in tumors expressing programmed death ligand 1, and non‑inferior outcome in frst‑line treatment compared to chemotherapy. This review summarizes the current state and progress of research on targeted therapy for advanced GC. Keywords: Gastric cancer, Targeted therapy, Human epidermal growth factor receptor 2, Programmed death‑1, Vascular endothelial growth factor receptor 2 Background GC mortality which is consistent with overall decrease in Gastric cancer (GC), including adenocarcinoma of the GC-related deaths [4]. gastroesophageal junction (GEJ) and stomach, is the ffth Tere have been several eforts to perform large-scale most common cancer and the third leading cause of can- molecular profling and classifcation of GC. -
Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -

New Biological Therapies: Introduction to the Basis of the Risk of Infection
New biological therapies: introduction to the basis of the risk of infection Mario FERNÁNDEZ RUIZ, MD, PhD Unit of Infectious Diseases Hospital Universitario “12 de Octubre”, Madrid ESCMIDInstituto de Investigación eLibraryHospital “12 de Octubre” (i+12) © by author Transparency Declaration Over the last 24 months I have received honoraria for talks on behalf of • Astellas Pharma • Gillead Sciences • Roche • Sanofi • Qiagen Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author Paul Ehrlich (1854-1915) • “side-chain” theory (1897) • receptor-ligand concept (1900) • “magic bullet” theory • foundation for specific chemotherapy (1906) • Nobel Prize in Physiology and Medicine (1908) (together with Metchnikoff) Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author 1981: B-1 antibody (tositumomab) anti-CD20 monoclonal antibody 1997: FDA approval of rituximab for the treatment of relapsed or refractory CD20-positive NHL 2001: FDA approval of imatinib for the treatment of chronic myelogenous leukemia Infections and biologicals: a real concern? (two-hour symposium): New biological therapies: introduction to the ESCMIDbasis of the risk of infection eLibrary © by author Functional classification of targeted (biological) agents • Agents targeting soluble immune effector molecules • Agents targeting cell surface receptors -
Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -
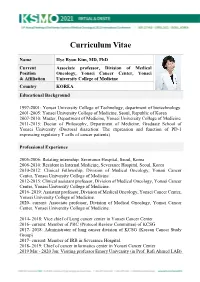
KSMO 2021 CV SS Hye
Curriculum Vitae Name Hye Ryun Kim, MD, PhD Current Associate professor, Division of Medical Position Oncology, Yonsei Cancer Center, Yonsei & Affiliation University College of Medicine Country KOREA Educational Background 1997-2001: Yonsei University College of Technology, department of biotechnology. 2001-2005: Yonsei University College of Medicine, Seoul, Republic of Korea 2007-2010: Master, Department of Medicine, Yonsei University College of Medicine 2011-2015: Doctor of Philosophy, Department of Medicine, Graduate School of Yonsei University (Doctoral dissertion: The expression and function of PD-1 expressing regulatory T cells of cancer patients) Professional Experience 2005-2006: Rotating internship, Severance Hospital, Seoul, Korea 2006-2010: Resident in Internal Medicine, Severance Hospital, Seoul, Korea 2010-2012: Clinical Fellowship, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2012-2015: Clinical assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2016- 2019: Assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2020- current: Associate professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2014- 2018: Vice chief of Lung cancer center in Yonsei Cancer Center 2016- current: Member of PRC (Protocol Review Committee) of KCSG 2017- 2018: Administrator of lung cancer division of KCSG (Korean Cancer Study Group) 2017- current: -

Advances in Epidermal Growth Factor Receptor Specific Immunotherapy: Lessons to Be Learned from Armed Antibodies
www.oncotarget.com Oncotarget, 2020, Vol. 11, (No. 38), pp: 3531-3557 Review Advances in epidermal growth factor receptor specific immunotherapy: lessons to be learned from armed antibodies Fleury Augustin Nsole Biteghe1,*, Neelakshi Mungra2,*, Nyangone Ekome Toung Chalomie4, Jean De La Croix Ndong5, Jean Engohang-Ndong6, Guillaume Vignaux7, Eden Padayachee8, Krupa Naran2,* and Stefan Barth2,3,* 1Department of Radiation Oncology and Biomedical Sciences, Cedars-Sinai Medical, Los Angeles, CA, USA 2Medical Biotechnology & Immunotherapy Research Unit, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 3South African Research Chair in Cancer Biotechnology, Department of Integrative Biomedical Sciences, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 4Sun Yat-Sen University, Zhongshan Medical School, Guangzhou, China 5Department of Orthopedic Surgery, New York University School of Medicine, New York, NY, USA 6Department of Biological Sciences, Kent State University at Tuscarawas, New Philadelphia, OH, USA 7Arctic Slope Regional Corporation Federal, Beltsville, MD, USA 8Department of Physiology, University of Kentucky, Lexington, KY, USA *These authors contributed equally to this work Correspondence to: Stefan Barth, email: [email protected] Keywords: epidermal growth factor receptor (EGFR); recombinant immunotoxins (ITs); targeted human cytolytic fusion proteins (hCFPs); recombinant antibody-drug conjugates (rADCs); recombinant antibody photoimmunoconjugates (rAPCs) Received: May 30, 2020 Accepted: August 11, 2020 Published: September 22, 2020 Copyright: © 2020 Biteghe et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Whither Radioimmunotherapy: to Be Or Not to Be? Damian J
Published OnlineFirst April 20, 2017; DOI: 10.1158/0008-5472.CAN-16-2523 Cancer Perspective Research Whither Radioimmunotherapy: To Be or Not To Be? Damian J. Green1,2 and Oliver W. Press1,2,3 Abstract Therapy of cancer with radiolabeled monoclonal antibodies employing multistep "pretargeting" methods, particularly those has produced impressive results in preclinical experiments and in utilizing bispecific antibodies, have greatly enhanced the thera- clinical trials conducted in radiosensitive malignancies, particu- peutic efficacy of radioimmunotherapy and diminished its toxi- larly B-cell lymphomas. Two "first-generation," directly radiola- cities. The dramatically improved therapeutic index of bispecific beled anti-CD20 antibodies, 131iodine-tositumomab and 90yttri- antibody pretargeting appears to be sufficiently compelling to um-ibritumomab tiuxetan, were FDA-approved more than a justify human clinical trials and reinvigorate enthusiasm for decade ago but have been little utilized because of a variety of radioimmunotherapy in the treatment of malignancies, particu- medical, financial, and logistic obstacles. Newer technologies larly lymphomas. Cancer Res; 77(9); 1–6. Ó2017 AACR. "To be, or not to be, that is the question: Whether 'tis nobler in the pembrolizumab (anti-PD-1), which are not directly cytotoxic mind to suffer the slings and arrows of outrageous fortune, or to take for cancer cells but "release the brakes" on the immune system, arms against a sea of troubles, And by opposing end them." Hamlet. allowing cytotoxic T cells to be more effective at recognizing –William Shakespeare. and killing cancer cells. Outstanding results have already been demonstrated with checkpoint inhibiting antibodies even in far Introduction advanced refractory solid tumors including melanoma, lung cancer, Hodgkin lymphoma and are under study for a multi- Impact of monoclonal antibodies on the field of clinical tude of other malignancies (4–6). -

B-Cell Targets to Treat Antibody-Mediated Rejection In
Muro et al. Int J Transplant Res Med 2016, 2:023 Volume 2 | Issue 2 International Journal of Transplantation Research and Medicine Commentary: Open Access B-Cell Targets to Treat Antibody-Mediated Rejection in Transplantation Manuel Muro1*, Santiago Llorente2, Jose A Galian1, Francisco Boix1, Jorge Eguia1, Gema Gonzalez-Martinez1, Maria R Moya-Quiles1 and Alfredo Minguela1 1Immunology Service, University Clinic Hospital Virgen de la Arrixaca, Spain 2Nephrology Service, University Clinic Hospital Virgen de la Arrixaca, Spain *Corresponding author: Manuel Muro, PhD, Immunology Service, University Clinic Hospital “Virgen de la Arrixaca”, Biomedical Research Institute of Murcia (IMIB), Murcia, Spain, Tel: 34-968-369599, E-mail: [email protected] Antibody-mediated rejection (AMR) in allograft transplantation APRIL (a proliferation-inducing ligand). These co-activation signals can be defined with a rapid increase in the levels of specific are required for B-cell differentiation into plasma cell and enhancing serological parameters after organ transplantation, presence of donor their posterior survival and are a key determinant of whether specific antibodies (DSAs) against human leukocyte antigen (HLA) developing B-cells will survive or die during the establishment molecules, blood group (ABO) antigens and/or endothelial cell of immuno-tolerance [5,6]. Important used agents commercially antigens (e.g. MICA, ECA, Vimentin, or ETAR) and also particular available are Tocilizumab (anti-IL6R) and Belimumab (BAFF). histological parameters [1,2]. If the AMR persists or progresses, the The receptors of BAFF and APRIL could also be important as treatment to eliminate the humoral component of acute rejection eventual targets, for example BAFF-R, TACI (transmembrane include three sequential steps: (a) steroid pulses, antibody removal activator and calcium modulator and cyclophyllin ligand interactor) (plasma exchange or immuno-adsorption) and high doses of and BCMA (B-cell maturation antigen).