Carbonic Anhydrases and Metabolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Association Analyses of Known Genetic Variants with Gene
ASSOCIATION ANALYSES OF KNOWN GENETIC VARIANTS WITH GENE EXPRESSION IN BRAIN by Viktoriya Strumba A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Bioinformatics) in The University of Michigan 2009 Doctoral Committee: Professor Margit Burmeister, Chair Professor Huda Akil Professor Brian D. Athey Assistant Professor Zhaohui S. Qin Research Statistician Thomas Blackwell To Sam and Valentina Dmitriy and Elizabeth ii ACKNOWLEDGEMENTS I would like to thank my advisor Professor Margit Burmeister, who tirelessly guided me though seemingly impassable corridors of graduate work. Throughout my thesis writing period she provided sound advice, encouragement and inspiration. Leading by example, her enthusiasm and dedication have been instrumental in my path to becoming a better scientist. I also would like to thank my co-advisor Tom Blackwell. His careful prodding always kept me on my toes and looking for answers, which taught me the depth of careful statistical analysis. His diligence and dedication have been irreplaceable in most difficult of projects. I also would like to thank my other committee members: Huda Akil, Brian Athey and Steve Qin as well as David States. You did not make it easy for me, but I thank you for believing and not giving up. Huda’s eloquence in every subject matter she explained have been particularly inspiring, while both Huda’s and Brian’s valuable advice made the completion of this dissertation possible. I would also like to thank all the members of the Burmeister lab, both past and present: Sandra Villafuerte, Kristine Ito, Cindy Schoen, Karen Majczenko, Ellen Schmidt, Randi Burns, Gang Su, Nan Xiang and Ana Progovac. -
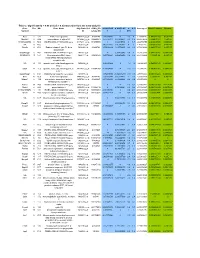
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Supplementary Information
Supplementary Information Network-based Drug Repurposing for Novel Coronavirus 2019-nCoV Yadi Zhou1,#, Yuan Hou1,#, Jiayu Shen1, Yin Huang1, William Martin1, Feixiong Cheng1-3,* 1Genomic Medicine Institute, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44195, USA 2Department of Molecular Medicine, Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH 44195, USA 3Case Comprehensive Cancer Center, Case Western Reserve University School of Medicine, Cleveland, OH 44106, USA #Equal contribution *Correspondence to: Feixiong Cheng, PhD Lerner Research Institute Cleveland Clinic Tel: +1-216-444-7654; Fax: +1-216-636-0009 Email: [email protected] Supplementary Table S1. Genome information of 15 coronaviruses used for phylogenetic analyses. Supplementary Table S2. Protein sequence identities across 5 protein regions in 15 coronaviruses. Supplementary Table S3. HCoV-associated host proteins with references. Supplementary Table S4. Repurposable drugs predicted by network-based approaches. Supplementary Table S5. Network proximity results for 2,938 drugs against pan-human coronavirus (CoV) and individual CoVs. Supplementary Table S6. Network-predicted drug combinations for all the drug pairs from the top 16 high-confidence repurposable drugs. 1 Supplementary Table S1. Genome information of 15 coronaviruses used for phylogenetic analyses. GenBank ID Coronavirus Identity % Host Location discovered MN908947 2019-nCoV[Wuhan-Hu-1] 100 Human China MN938384 2019-nCoV[HKU-SZ-002a] 99.99 Human China MN975262 -

An Investigation Into the Carbonic Anhydrase Isozymes from Zea
This file is part of the following reference: Tems, Ursula (2009) Characterization of the carbonic anhydrase isozymes of zea mays. PhD thesis, James Cook University. Access to this file is available from: http://eprints.jcu.edu.au/8807 Characterization of the Carbonic Anhydrase Isozymes of Zea mays Thesis submitted by Ursula TEMS B.Sc. Hons (JCU) February 2009 for the degree of Doctor of Philosophy in the School of Pharmacy and Molecular Sciences James Cook University Statement of Sources I declare that this thesis is my own work and has not been submitted in any form for another degree or diploma at any university or other institution of tertiary education. Information derived from the published or unpublished work of others has been acknowledged in the text and a list of references is given. Signature Date i Statement of Access I, the undersigned, author of this work, understand that James Cook University will make this thesis available for use within the University Library and, via the Australian Digital Theses network, for use elsewhere. I understand that, as an unpublished work, a thesis has significant protection under the Copyright Act and; I do not wish to place any further restriction on access to this work. Signature Date Declaration I, the undersigned, the author of this work, declare that the electronic copy of this thesis provided to the James Cook University Library is an accurate copy of the print thesis submitted, within the limits of the technology available. Signature Date ii Acknowledgements I would like to express my sincere gratitude to my supervisor Jim Burnell for his enthusiasm, encouragement and guidance. -

Computational Drug Target Screening Through Protein Interaction Profiles
www.nature.com/scientificreports OPEN Computational Drug Target Screening through Protein Interaction Profiles Received: 27 June 2016 Santiago Vilar1,2, Elías Quezada3, Eugenio Uriarte2, Stefano Costanzi4, Fernanda Borges3, Accepted: 24 October 2016 Dolores Viña5 & George Hripcsak1 Published: 15 November 2016 The development of computational methods to discover novel drug-target interactions on a large scale is of great interest. We propose a new method for virtual screening based on protein interaction profile similarity to discover new targets for molecules, including existing drugs. We calculated Target Interaction Profile Fingerprints (TIPFs) based on ChEMBL database to evaluate drug similarity and generated new putative compound-target candidates from the non-intersecting targets in each pair of compounds. A set of drugs was further studied in monoamine oxidase B (MAO-B) and cyclooxygenase-1 (COX-1) enzyme through molecular docking and experimental assays. The drug ethoxzolamide and the natural compound piperlongumine, present in Piper longum L, showed hMAO-B activity with IC50 values of 25 and 65 μM respectively. Five candidates, including lapatinib, SB-202190, RO-316233, GW786460X and indirubin-3′-monoxime were tested against human COX-1. Compounds SB-202190 and RO-316233 showed a IC50 in hCOX-1 of 24 and 25 μM respectively (similar range as potent inhibitors such as diclofenac and indomethacin in the same experimental conditions). Lapatinib and indirubin- 3′-monoxime showed moderate hCOX-1 activity (19.5% and 28% of enzyme inhibition at 25 μM respectively). Our modeling constitutes a multi-target predictor for large scale virtual screening with potential in lead discovery, repositioning and drug safety. Discovery of new targets for molecules is of great interest in drug design and development1,2. -

Role of Amylase in Ovarian Cancer Mai Mohamed University of South Florida, [email protected]
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School July 2017 Role of Amylase in Ovarian Cancer Mai Mohamed University of South Florida, [email protected] Follow this and additional works at: http://scholarcommons.usf.edu/etd Part of the Pathology Commons Scholar Commons Citation Mohamed, Mai, "Role of Amylase in Ovarian Cancer" (2017). Graduate Theses and Dissertations. http://scholarcommons.usf.edu/etd/6907 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Role of Amylase in Ovarian Cancer by Mai Mohamed A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Pathology and Cell Biology Morsani College of Medicine University of South Florida Major Professor: Patricia Kruk, Ph.D. Paula C. Bickford, Ph.D. Meera Nanjundan, Ph.D. Marzenna Wiranowska, Ph.D. Lauri Wright, Ph.D. Date of Approval: June 29, 2017 Keywords: ovarian cancer, amylase, computational analyses, glycocalyx, cellular invasion Copyright © 2017, Mai Mohamed Dedication This dissertation is dedicated to my parents, Ahmed and Fatma, who have always stressed the importance of education, and, throughout my education, have been my strongest source of encouragement and support. They always believed in me and I am eternally grateful to them. I would also like to thank my brothers, Mohamed and Hussien, and my sister, Mariam. I would also like to thank my husband, Ahmed. -

High-Throughput Screening Studies of Inhibition of Human Carbonic Anhydrase II and Bacterial Flagella Antimicrobial Activity
Western Michigan University ScholarWorks at WMU Dissertations Graduate College 5-2010 High-Throughput Screening Studies of Inhibition of Human Carbonic Anhydrase II and Bacterial Flagella Antimicrobial Activity Albert A. Barrese III Western Michigan University Follow this and additional works at: https://scholarworks.wmich.edu/dissertations Part of the Biochemistry, Biophysics, and Structural Biology Commons, and the Biology Commons Recommended Citation Barrese, Albert A. III, "High-Throughput Screening Studies of Inhibition of Human Carbonic Anhydrase II and Bacterial Flagella Antimicrobial Activity" (2010). Dissertations. 500. https://scholarworks.wmich.edu/dissertations/500 This Dissertation-Open Access is brought to you for free and open access by the Graduate College at ScholarWorks at WMU. It has been accepted for inclusion in Dissertations by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. HIGH-THROUGHPUT SCREENING STUDIES OF INHIBITION OF HUMAN CARBONIC ANHYDRASE II AND BACTERIAL FLAGELLA ANTIMICROBIAL ACTIVITY by Albert A. Barrese III A Dissertation Submitted to the Faculty of The Graduate College in partial fulfillment of the requirements for the Degree of Doctor of Philosophy Department of Biological Sciences Advisor: Brian C. Tripp, Ph.D. Western Michigan University Kalamazoo, Michigan May 2010 UMI Number: 3410393 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. UMT Dissertation Publishing UMI 3410393 Copyright 2010 by ProQuest LLC. -
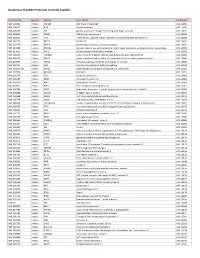
Quantigene Flowrna Probe Sets Currently Available
QuantiGene FlowRNA Probe Sets Currently Available Accession No. Species Symbol Gene Name Catalog No. NM_003452 Human ZNF189 zinc finger protein 189 VA1-10009 NM_000057 Human BLM Bloom syndrome VA1-10010 NM_005269 Human GLI glioma-associated oncogene homolog (zinc finger protein) VA1-10011 NM_002614 Human PDZK1 PDZ domain containing 1 VA1-10015 NM_003225 Human TFF1 Trefoil factor 1 (breast cancer, estrogen-inducible sequence expressed in) VA1-10016 NM_002276 Human KRT19 keratin 19 VA1-10022 NM_002659 Human PLAUR plasminogen activator, urokinase receptor VA1-10025 NM_017669 Human ERCC6L excision repair cross-complementing rodent repair deficiency, complementation group 6-like VA1-10029 NM_017699 Human SIDT1 SID1 transmembrane family, member 1 VA1-10032 NM_000077 Human CDKN2A cyclin-dependent kinase inhibitor 2A (melanoma, p16, inhibits CDK4) VA1-10040 NM_003150 Human STAT3 signal transducer and activator of transcripton 3 (acute-phase response factor) VA1-10046 NM_004707 Human ATG12 ATG12 autophagy related 12 homolog (S. cerevisiae) VA1-10047 NM_000737 Human CGB chorionic gonadotropin, beta polypeptide VA1-10048 NM_001017420 Human ESCO2 establishment of cohesion 1 homolog 2 (S. cerevisiae) VA1-10050 NM_197978 Human HEMGN hemogen VA1-10051 NM_001738 Human CA1 Carbonic anhydrase I VA1-10052 NM_000184 Human HBG2 Hemoglobin, gamma G VA1-10053 NM_005330 Human HBE1 Hemoglobin, epsilon 1 VA1-10054 NR_003367 Human PVT1 Pvt1 oncogene homolog (mouse) VA1-10061 NM_000454 Human SOD1 Superoxide dismutase 1, soluble (amyotrophic lateral sclerosis 1 (adult)) -

An Update on the Metabolic Roles of Carbonic Anhydrases in the Model Alga Chlamydomonas Reinhardtii
H OH metabolites OH Review An Update on the Metabolic Roles of Carbonic Anhydrases in the Model Alga Chlamydomonas reinhardtii Ashok Aspatwar 1,* ID , Susanna Haapanen 1 and Seppo Parkkila 1,2 1 Faculty of Medicine and Life Sciences, University of Tampere, FI-33014 Tampere, Finland; [email protected].fi (S.H.); [email protected].fi (S.P.) 2 Fimlab, Ltd., and Tampere University Hospital, FI-33520 Tampere, Finland * Correspondence: [email protected].fi; Tel.: +358-46-596-2117 Received: 11 January 2018; Accepted: 10 March 2018; Published: 13 March 2018 Abstract: Carbonic anhydrases (CAs) are metalloenzymes that are omnipresent in nature. − + CAs catalyze the basic reaction of the reversible hydration of CO2 to HCO3 and H in all living organisms. Photosynthetic organisms contain six evolutionarily different classes of CAs, which are namely: α-CAs, β-CAs, γ-CAs, δ-CAs, ζ-CAs, and θ-CAs. Many of the photosynthetic organisms contain multiple isoforms of each CA family. The model alga Chlamydomonas reinhardtii contains 15 CAs belonging to three different CA gene families. Of these 15 CAs, three belong to the α-CA gene family; nine belong to the β-CA gene family; and three belong to the γ-CA gene family. The multiple copies of the CAs in each gene family may be due to gene duplications within the particular CA gene family. The CAs of Chlamydomonas reinhardtii are localized in different subcellular compartments of this unicellular alga. The presence of a large number of CAs and their diverse subcellular localization within a single cell suggests the importance of these enzymes in the metabolic and biochemical roles they perform in this unicellular alga. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

Interaction of Benzodiazepines with Central Nervous Glycine Receptors: Possible Mechanism of Action (Strychnine Binding/Behavioral Tests) ANNE B
Proc. Nat. Acad. Sci. USA Vol. 71, No. 6, pp. 2246-2250, June 1974 Interaction of Benzodiazepines with Central Nervous Glycine Receptors: Possible Mechanism of Action (strychnine binding/behavioral tests) ANNE B. YOUNG, STEPHEN R. ZUKIN, AND SOLOMON H. SNYDER* Departments of Pharmacology and Experimental Therapeutics and Psychiatry and the Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205 Communicaed by Cheves Walling, January 29, 1974 ABSTRACT Interaction of 21 benzodiazepines with the ously (4). The specific activity of the labeled strychnine was glycine receptor in the brainstem and spinal cord of rat have been evaluated in terms of their displacement of 13 Ci/mmol, with concentrations determined by comparison ['HIstrychnine binding. The rank order of potency of the with the ultraviolet absorption of standard solutions at 254 21 drugs in displacing specific ['H1strychnine binding cor- nm. relates (p < 0.005) with their rank order of potency in a variety of pharmacological and behavioral tests in Tissue Preparation. Male Sprague-Dawley rats (100-150 g) humans and animals that predict clinical efficacy. There were decapitated and the brainstems and spinal cords re- is a 50-fold variation in potency of the series of benzo- moved. Crude synaptic membrane fractions of these tissues diazepines with mean effective dose (ED5.) values ranging were prepared by the differential centrifugation technique from 19juM to >1000 pM. Diazepam (Valium®) and chlor- diazepoxide (Librium®) have EDN's of 26 MM and 200 pM, previously reported (4). respectively, whereas the ED5. for glycine is 25 ;M. The in- hibitory effects of 10 of the agents in two other central ner- Binding A8say. -

Dissertation Kollipara.Pdf
Characterizing protein processing in the Endoplasmic Reticulum using quantitative proteomics: the pathogenesis of the Marinesco-Sjörgren Syndrome Zur Erlangung des akademischen Grades eines Dr. rer. nat von der Fakultät Bio- und Chemieingenieurwesen der Technischen Universität Dortmund genehmigte Dissertation vorgelegt von MSc. Laxmikanth Kollipara aus Hyderabad, India Tag der mündlichen Prüfung: 20.12.2016 1. Gutachter: Prof. Dr. Albert Sickmann 2. Gutachter: Prof. Dr. Oliver Kayser Dortmund 2016 1. Prüfer: Prof. Dr. Markus Nett Abstract Abstract In this work, characterization of Marinesco-Sjögren Syndrome (MSS) was performed for the first time on the proteome level using mass spectrometry (MS)-based quantitative proteomics strategies. MSS is a neuromuscular and neurodegenerative disorder and it is caused due to the mutational inactivation of SIL1 protein, which results in malfunctioning of protein folding machinery mediated by the chaperone BiP that can lead to the ER stress-induced cell death via apoptotic signaling. The major goals were (i) to understand the rescue mechanisms in SIL1-deficient non-vulnerable tissues from human and (ii) to verify the cellular perturbations caused due to the loss of functional SIL1 in woozy mouse (i.e. mouse model of MSS). To achieve these aims, samples derived from five different MSS cases and two different tissues from woozy along with their respective healthy controls were studied. For this, comparative LC-MS proteomics approaches such as chemical labeling (i.e. iTRAQ) and label- free quantification (precursor ion intensity based and NSAF) were employed. During which, sample preparation workflows were optimized that enabled to process clinical samples related to MSS that included primary cell lines and mammalian tissues for the subsequent quantitative LC-MS analyses.