Building a Metabolic Bridge Between Glycolysis and Sphingolipid Biosynthesis : Implications in Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Gene Symbol Gene Description ACVR1B Activin a Receptor, Type IB
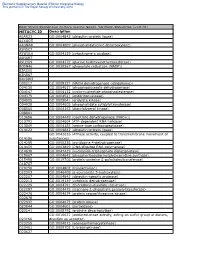
Table S1. Kinase clones included in human kinase cDNA library for yeast two-hybrid screening Gene Symbol Gene Description ACVR1B activin A receptor, type IB ADCK2 aarF domain containing kinase 2 ADCK4 aarF domain containing kinase 4 AGK multiple substrate lipid kinase;MULK AK1 adenylate kinase 1 AK3 adenylate kinase 3 like 1 AK3L1 adenylate kinase 3 ALDH18A1 aldehyde dehydrogenase 18 family, member A1;ALDH18A1 ALK anaplastic lymphoma kinase (Ki-1) ALPK1 alpha-kinase 1 ALPK2 alpha-kinase 2 AMHR2 anti-Mullerian hormone receptor, type II ARAF v-raf murine sarcoma 3611 viral oncogene homolog 1 ARSG arylsulfatase G;ARSG AURKB aurora kinase B AURKC aurora kinase C BCKDK branched chain alpha-ketoacid dehydrogenase kinase BMPR1A bone morphogenetic protein receptor, type IA BMPR2 bone morphogenetic protein receptor, type II (serine/threonine kinase) BRAF v-raf murine sarcoma viral oncogene homolog B1 BRD3 bromodomain containing 3 BRD4 bromodomain containing 4 BTK Bruton agammaglobulinemia tyrosine kinase BUB1 BUB1 budding uninhibited by benzimidazoles 1 homolog (yeast) BUB1B BUB1 budding uninhibited by benzimidazoles 1 homolog beta (yeast) C9orf98 chromosome 9 open reading frame 98;C9orf98 CABC1 chaperone, ABC1 activity of bc1 complex like (S. pombe) CALM1 calmodulin 1 (phosphorylase kinase, delta) CALM2 calmodulin 2 (phosphorylase kinase, delta) CALM3 calmodulin 3 (phosphorylase kinase, delta) CAMK1 calcium/calmodulin-dependent protein kinase I CAMK2A calcium/calmodulin-dependent protein kinase (CaM kinase) II alpha CAMK2B calcium/calmodulin-dependent -

From Genes to Systems: New Global Strategies for the Characterization of NCL Biology ⁎ Anu Jalanko A, , Jaana Tyynelä B, Leena Peltonen A,C,D,E
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1762 (2006) 934–944 www.elsevier.com/locate/bbadis Review From genes to systems: New global strategies for the characterization of NCL biology ⁎ Anu Jalanko a, , Jaana Tyynelä b, Leena Peltonen a,c,d,e a National Public Health Institute, Department of Molecular Medicine, Biomedicum Helsinki, P.O. Box 104, 00251 Helsinki, Finland b University of Helsinki, Institute of Biomedicine/Biochemistry, Finland c University of Helsinki, Department of Medical Genetics, Finland d Research Programme of Molecular Medicine and Research Programme of Neurosciences, Biomedicum Helsinki, Finland e The Broad Institute of MIT and Harvard, Cambridge, Massachusetts, USA Received 22 April 2006; received in revised form 1 September 2006; accepted 5 September 2006 Available online 12 September 2006 Abstract Neuronal ceroid lipofuscinoses (NCL) are rare neurological disorders with a uniform phenotype, caused by mutations in seven known genes. NCL provide a unique model to characterize molecular pathways critical for normal neuronal development and pathological neuronal degeneration. Systems biology based approach utilizes the rapidly developing tools of genomics, proteomics, lipidomics and metabolomics and aims at thorough understanding of the functions of cells, tissues and whole organisms by molecular analysis and biocomputing-assisted modeling. The systems level understanding of NCL is now possible by utilizing different model organisms. Initial work has revealed disturbed metabolic pathways in several NCL disorders and most analyses have utilized the infantile (INCL/CLN1) and juvenile (JNCL/CLN3) disease modeling and utilized mainly human and mouse samples. -

Sphingolipid Metabolism Diseases ⁎ Thomas Kolter, Konrad Sandhoff
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1758 (2006) 2057–2079 www.elsevier.com/locate/bbamem Review Sphingolipid metabolism diseases ⁎ Thomas Kolter, Konrad Sandhoff Kekulé-Institut für Organische Chemie und Biochemie der Universität, Gerhard-Domagk-Str. 1, D-53121 Bonn, Germany Received 23 December 2005; received in revised form 26 April 2006; accepted 23 May 2006 Available online 14 June 2006 Abstract Human diseases caused by alterations in the metabolism of sphingolipids or glycosphingolipids are mainly disorders of the degradation of these compounds. The sphingolipidoses are a group of monogenic inherited diseases caused by defects in the system of lysosomal sphingolipid degradation, with subsequent accumulation of non-degradable storage material in one or more organs. Most sphingolipidoses are associated with high mortality. Both, the ratio of substrate influx into the lysosomes and the reduced degradative capacity can be addressed by therapeutic approaches. In addition to symptomatic treatments, the current strategies for restoration of the reduced substrate degradation within the lysosome are enzyme replacement therapy (ERT), cell-mediated therapy (CMT) including bone marrow transplantation (BMT) and cell-mediated “cross correction”, gene therapy, and enzyme-enhancement therapy with chemical chaperones. The reduction of substrate influx into the lysosomes can be achieved by substrate reduction therapy. Patients suffering from the attenuated form (type 1) of Gaucher disease and from Fabry disease have been successfully treated with ERT. © 2006 Elsevier B.V. All rights reserved. Keywords: Ceramide; Lysosomal storage disease; Saposin; Sphingolipidose Contents 1. Sphingolipid structure, function and biosynthesis ..........................................2058 1.1. -

Supplementary Materials
1 Supplementary Materials: Supplemental Figure 1. Gene expression profiles of kidneys in the Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice. (A) A heat map of microarray data show the genes that significantly changed up to 2 fold compared between Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice (N=4 mice per group; p<0.05). Data show in log2 (sample/wild-type). 2 Supplemental Figure 2. Sting signaling is essential for immuno-phenotypes of the Fcgr2b-/-lupus mice. (A-C) Flow cytometry analysis of splenocytes isolated from wild-type, Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice at the age of 6-7 months (N= 13-14 per group). Data shown in the percentage of (A) CD4+ ICOS+ cells, (B) B220+ I-Ab+ cells and (C) CD138+ cells. Data show as mean ± SEM (*p < 0.05, **p<0.01 and ***p<0.001). 3 Supplemental Figure 3. Phenotypes of Sting activated dendritic cells. (A) Representative of western blot analysis from immunoprecipitation with Sting of Fcgr2b-/- mice (N= 4). The band was shown in STING protein of activated BMDC with DMXAA at 0, 3 and 6 hr. and phosphorylation of STING at Ser357. (B) Mass spectra of phosphorylation of STING at Ser357 of activated BMDC from Fcgr2b-/- mice after stimulated with DMXAA for 3 hour and followed by immunoprecipitation with STING. (C) Sting-activated BMDC were co-cultured with LYN inhibitor PP2 and analyzed by flow cytometry, which showed the mean fluorescence intensity (MFI) of IAb expressing DC (N = 3 mice per group). 4 Supplemental Table 1. Lists of up and down of regulated proteins Accession No. -

Activation of Sphingosine Kinase 1 by ERK1/2Mediated Phosphorylation
The EMBO Journal Vol. 22 No. 20 pp. 5491±5500, 2003 Activation of sphingosine kinase 1 by ERK1/2-mediated phosphorylation Stuart M.Pitson1,2, Paul A.B.Moretti1, second messenger and a ligand for cell-surface receptors Julia R.Zebol1, Helen E.Lynn1, Pu Xia1,3, (Hla et al., 2001; Spiegel and Milstien, 2002). MathewA.Vadas 1,3 and The cellular levels of S1P are controlled by its Binks W.Wattenberg1,4 formation from sphingosine through the activity of sphingosine kinase, and by its degradation by S1P lyase 1Hanson Institute, Division of Human Immunology, Institute of (Van Veldhoven et al., 2000) and S1P phosphatases Medical and Veterinary Science, Frome Road, Adelaide, SA 5000 and (Mandala, 2001). In the basal state, this balance between 3Department of Medicine, Adelaide University, Frome Road, Adelaide, Australia S1P generation and degradation results in low cellular levels of S1P (Pyne and Pyne, 2000). However, when cells 4Present address: James Graham Brown Cancer Center, Dehlia Baxter Research Building, 580 S. Preston Avenue, Louisville, KY 40202, are exposed to speci®c growth factors and other agonists USA like tumour necrosis factor-a (TNFa) or phorbol esters the cellular levels of S1P can increase rapidly and transiently 2Corresponding author e-mail: [email protected] (Pitson et al., 2000b). This results in the triggering of various signalling pathways through as yet unidenti®ed Sphingosine kinase 1 is an agonist-activated signalling intracellular S1P targets, as well as through the engage- enzyme that catalyses the formation of sphingosine ment of cell surface S1P receptors following its release 1-phosphate, a lipid second messenger that has been from cells (Hobson et al., 2001). -

GM2 Gangliosidoses: Clinical Features, Pathophysiological Aspects, and Current Therapies
International Journal of Molecular Sciences Review GM2 Gangliosidoses: Clinical Features, Pathophysiological Aspects, and Current Therapies Andrés Felipe Leal 1 , Eliana Benincore-Flórez 1, Daniela Solano-Galarza 1, Rafael Guillermo Garzón Jaramillo 1 , Olga Yaneth Echeverri-Peña 1, Diego A. Suarez 1,2, Carlos Javier Alméciga-Díaz 1,* and Angela Johana Espejo-Mojica 1,* 1 Institute for the Study of Inborn Errors of Metabolism, Faculty of Science, Pontificia Universidad Javeriana, Bogotá 110231, Colombia; [email protected] (A.F.L.); [email protected] (E.B.-F.); [email protected] (D.S.-G.); [email protected] (R.G.G.J.); [email protected] (O.Y.E.-P.); [email protected] (D.A.S.) 2 Faculty of Medicine, Universidad Nacional de Colombia, Bogotá 110231, Colombia * Correspondence: [email protected] (C.J.A.-D.); [email protected] (A.J.E.-M.); Tel.: +57-1-3208320 (ext. 4140) (C.J.A.-D.); +57-1-3208320 (ext. 4099) (A.J.E.-M.) Received: 6 July 2020; Accepted: 7 August 2020; Published: 27 August 2020 Abstract: GM2 gangliosidoses are a group of pathologies characterized by GM2 ganglioside accumulation into the lysosome due to mutations on the genes encoding for the β-hexosaminidases subunits or the GM2 activator protein. Three GM2 gangliosidoses have been described: Tay–Sachs disease, Sandhoff disease, and the AB variant. Central nervous system dysfunction is the main characteristic of GM2 gangliosidoses patients that include neurodevelopment alterations, neuroinflammation, and neuronal apoptosis. Currently, there is not approved therapy for GM2 gangliosidoses, but different therapeutic strategies have been studied including hematopoietic stem cell transplantation, enzyme replacement therapy, substrate reduction therapy, pharmacological chaperones, and gene therapy. -

Lipid Metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives
cancers Review Lipid metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives 1, 1, 1 2 1 Laurence Pellerin y, Lorry Carrié y , Carine Dufau , Laurence Nieto , Bruno Ségui , 1,3 1, , 1, , Thierry Levade , Joëlle Riond * z and Nathalie Andrieu-Abadie * z 1 Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, Université Fédérale de Toulouse Midi-Pyrénées, Université Toulouse III Paul-Sabatier, Inserm 1037, 2 avenue Hubert Curien, tgrCS 53717, 31037 Toulouse CEDEX 1, France; [email protected] (L.P.); [email protected] (L.C.); [email protected] (C.D.); [email protected] (B.S.); [email protected] (T.L.) 2 Institut de Pharmacologie et de Biologie Structurale, CNRS, Université Toulouse III Paul-Sabatier, UMR 5089, 205 Route de Narbonne, 31400 Toulouse, France; [email protected] 3 Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France * Correspondence: [email protected] (J.R.); [email protected] (N.A.-A.); Tel.: +33-582-7416-20 (J.R.) These authors contributed equally to this work. y These authors jointly supervised this work. z Received: 15 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Simple Summary: Melanoma is a devastating skin cancer characterized by an impressive metabolic plasticity. Melanoma cells are able to adapt to the tumor microenvironment by using a variety of fuels that contribute to tumor growth and progression. In this review, the authors summarize the contribution of the lipid metabolic network in melanoma plasticity and aggressiveness, with a particular attention to specific lipid classes such as glycerophospholipids, sphingolipids, sterols and eicosanoids. -

Glycosphingolipid Metabolism in Cell Fate Specification Domenico Russo1,*, Laura Capolupo1,2, Jaipreet Singh Loomba1,2, Lucia Sticco1 and Giovanni D’Angelo1,2,*
© 2018. Published by The Company of Biologists Ltd | Journal of Cell Science (2018) 131, jcs219204. doi:10.1242/jcs.219204 REVIEW Glycosphingolipid metabolism in cell fate specification Domenico Russo1,*, Laura Capolupo1,2, Jaipreet Singh Loomba1,2, Lucia Sticco1 and Giovanni D’Angelo1,2,* ABSTRACT anchoring. Specifically at the PM, sphingolipids participate in Glycosphingolipids (GSLs) are ubiquitous components of eukaryotic signaling events by recruiting signaling molecules to, or plasma membranes that consist of a ceramide backbone linked to a sequestering them at, membrane microdomains for the modulation glycan moiety. Both the ceramide and the glycan parts of GSLs display of their activities and for their processing into the endocytic cycle structural variations that result in a remarkable repertoire of diverse (Holthuis and Menon, 2014; Holthuis et al., 2001; Simons and compounds. This diversity of GSLs is exploited during embryogenesis, Ikonen, 1997). Given these properties, sphingolipids are proposed to when different GSLs are produced at specific developmental stages and function as fundamental membrane organizers and to make up along several differentiation trajectories. Importantly, plasma membrane the fabric of eukaryotic PMs in order to influence the interaction receptors interact with GSLsto modify their activities. Consequently, two with the extracellular environment (Hannun and Obeid, 2018; otherwise identical cells can respond differently to the same stimulus Holthuis et al., 2001). owing to their different GSL composition. The metabolic reprograming of Interestingly, different cell types exhibit a specific sphingolipid GSLs is in fact a necessary part of developmental programs, as its array at their PMs (Hakomori, 2003; Ngamukote et al., 2007) impairment results in developmental failure or tissue-specific defects. -

TITLE PAGE Oxidative Stress and Response to Thymidylate Synthase
Downloaded from molpharm.aspetjournals.org at ASPET Journals on October 2, 2021 -Targeted -Targeted 1 , University of of , University SC K.W.B., South Columbia, (U.O., Carolina, This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. -

Lipid Rafts Activation of a Neutral Sphingomyelinase in T Cells by + and Proliferation of Human CD4 Cholera Toxin B-Subunit Prev
Cholera Toxin B-Subunit Prevents Activation and Proliferation of Human CD4 + T Cells by Activation of a Neutral Sphingomyelinase in Lipid Rafts This information is current as of October 1, 2021. Alexandre K. Rouquette-Jazdanian, Arnaud Foussat, Laurence Lamy, Claudette Pelassy, Patricia Lagadec, Jean-Philippe Breittmayer and Claude Aussel J Immunol 2005; 175:5637-5648; ; doi: 10.4049/jimmunol.175.9.5637 Downloaded from http://www.jimmunol.org/content/175/9/5637 References This article cites 55 articles, 31 of which you can access for free at: http://www.jimmunol.org/content/175/9/5637.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on October 1, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2005 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Cholera Toxin B-Subunit Prevents Activation and Proliferation of Human CD4؉ T Cells by Activation of a Neutral Sphingomyelinase in Lipid Rafts1 Alexandre K. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase