Kinase-Targeted Cancer Therapies: Progress, Challenges and Future Directions Khushwant S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Mutation Analysis in Myeloproliferative Neoplasms AHS - M2101
Corporate Medical Policy Mutation Analysis in Myeloproliferative Neoplasms AHS - M2101 File Name: mutation_analysis_in_myeloproliferative_neoplasms Origination: 1/1/2019 Last CAP review: 8/2021 Next CAP review: 8/2022 Last Review: 8/2021 Description of Procedure or Service Myeloproliferative neoplasms (MPN) are a heterogeneous group of clonal disorders characterized by overproduction of one or more differentiated myeloid lineages (Grinfeld, Nangalia, & Green, 2017). These include polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). The majority of MPN result from somatic mutations in the 3 driver genes, JAK2, CALR, and MPL, which represent major diagnostic criteria in combination with hematologic and morphological abnormalities (Rumi & Cazzola, 2017). Related Policies: BCR-ABL 1 Testing for Chronic Myeloid Leukemia AHS-M2027 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for mutation analysis in myeloproliferative neoplasms when it is determined to be medically necessary because the medical criteria and guidelines shown below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Mutation Analysis in Myeloproliferative Neoplasms is covered 1. JAK2, CALR or MPL mutation testing is considered medically necessary for the diagnosis of patients presenting with clinical, laboratory, or pathological findings suggesting classic forms of myeloproliferative neoplasms (MPN), that is, polycythemia vera (PV), essential thrombocythemia (ET), or primary myelofibrosis (PMF) when ordered by a hematology and/or oncology specialist in the following situations: A. -

Aurora Kinase a in Gastrointestinal Cancers: Time to Target Ahmed Katsha1, Abbes Belkhiri1, Laura Goff3 and Wael El-Rifai1,2,4*
Katsha et al. Molecular Cancer (2015) 14:106 DOI 10.1186/s12943-015-0375-4 REVIEW Open Access Aurora kinase A in gastrointestinal cancers: time to target Ahmed Katsha1, Abbes Belkhiri1, Laura Goff3 and Wael El-Rifai1,2,4* Abstract Gastrointestinal (GI) cancers are a major cause of cancer-related deaths. During the last two decades, several studies have shown amplification and overexpression of Aurora kinase A (AURKA) in several GI malignancies. These studies demonstrated that AURKA not only plays a role in regulating cell cycle and mitosis, but also regulates a number of key oncogenic signaling pathways. Although AURKA inhibitors have moved to phase III clinical trials in lymphomas, there has been slower progress in GI cancers and solid tumors. Ongoing clinical trials testing AURKA inhibitors as a single agent or in combination with conventional chemotherapies are expected to provide important clinical information for targeting AURKA in GI cancers. It is, therefore, imperative to consider investigations of molecular determinants of response and resistance to this class of inhibitors. This will improve evaluation of the efficacy of these drugs and establish biomarker based strategies for enrollment into clinical trials, which hold the future direction for personalized cancer therapy. In this review, we will discuss the available data on AURKA in GI cancers. We will also summarize the major AURKA inhibitors that have been developed and tested in pre-clinical and clinical settings. Keywords: Aurora kinases, Therapy, AURKA inhibitors, MNL8237, Alisertib, Gastrointestinal, Cancer, Signaling pathways Introduction stage [9-11]. Furthermore, AURKA is critical for Mitotic kinases are the main proteins that coordinate ac- bipolar-spindle assembly where it interacts with Ran- curate mitotic processing [1]. -

Gene Symbol Gene Description ACVR1B Activin a Receptor, Type IB
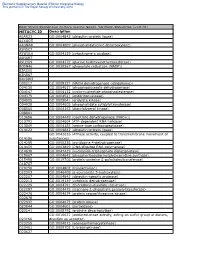
Table S1. Kinase clones included in human kinase cDNA library for yeast two-hybrid screening Gene Symbol Gene Description ACVR1B activin A receptor, type IB ADCK2 aarF domain containing kinase 2 ADCK4 aarF domain containing kinase 4 AGK multiple substrate lipid kinase;MULK AK1 adenylate kinase 1 AK3 adenylate kinase 3 like 1 AK3L1 adenylate kinase 3 ALDH18A1 aldehyde dehydrogenase 18 family, member A1;ALDH18A1 ALK anaplastic lymphoma kinase (Ki-1) ALPK1 alpha-kinase 1 ALPK2 alpha-kinase 2 AMHR2 anti-Mullerian hormone receptor, type II ARAF v-raf murine sarcoma 3611 viral oncogene homolog 1 ARSG arylsulfatase G;ARSG AURKB aurora kinase B AURKC aurora kinase C BCKDK branched chain alpha-ketoacid dehydrogenase kinase BMPR1A bone morphogenetic protein receptor, type IA BMPR2 bone morphogenetic protein receptor, type II (serine/threonine kinase) BRAF v-raf murine sarcoma viral oncogene homolog B1 BRD3 bromodomain containing 3 BRD4 bromodomain containing 4 BTK Bruton agammaglobulinemia tyrosine kinase BUB1 BUB1 budding uninhibited by benzimidazoles 1 homolog (yeast) BUB1B BUB1 budding uninhibited by benzimidazoles 1 homolog beta (yeast) C9orf98 chromosome 9 open reading frame 98;C9orf98 CABC1 chaperone, ABC1 activity of bc1 complex like (S. pombe) CALM1 calmodulin 1 (phosphorylase kinase, delta) CALM2 calmodulin 2 (phosphorylase kinase, delta) CALM3 calmodulin 3 (phosphorylase kinase, delta) CAMK1 calcium/calmodulin-dependent protein kinase I CAMK2A calcium/calmodulin-dependent protein kinase (CaM kinase) II alpha CAMK2B calcium/calmodulin-dependent -

Erb‑B2 Receptor Tyrosine Kinase 2 Is Negatively Regulated by the P53‑Responsive Microrna‑3184‑5P in Cervical Cancer Cells
ONCOLOGY REPORTS 45: 95-106, 2021 Erb‑B2 Receptor Tyrosine Kinase 2 is negatively regulated by the p53‑responsive microRNA‑3184‑5p in cervical cancer cells HONGLI LIU1, YUZHI LI1, JING ZHANG1, NAN WU2, FEI LIU2, LIHUA WANG1, YUAN ZHANG1, JING LIU1, XUAN ZHANG3, SUYANG GUO1 and HONGTAO WANG4 Departments of 1Gynecological Oncology and 2Respiration and Anhui Clinical and Preclinical Key Laboratory of Respiratory Disease, First Affiliated Hospital of Bengbu Medical College; Departments of3 Gynecological Oncology and 4Immunology and Anhui Key Laboratory of Infection and Immunity, Bengbu Medical College, Bengbu, Anhui 233030, P.R. China Received November 30, 2019; Accepted October 2, 2020 DOI: 10.3892/or.2020.7862 Abstract. The oncogenic role of Erb-B2 Receptor Tyrosine Introduction Kinase 2 (ERBB2) has been identified in several types of cancer, but less is known on its function and mechanism of Among women, cervical cancer is ranked 4th in global action in cervical cancer cells. The present study employed cancer-associated deaths (1), with over half a million deaths a multipronged approach to investigate the role of ERBB2 in in 2012 (2). Cervical cancer can be broadly categorized into cervical cancer. ERBB2 and microRNA (miR)-3184-5p expres- squamous cell carcinoma, which constitutes the majority of sion was assessed in patient-derived cervical cancer biopsy cases (70-80%) or adenocarcinoma, which comprises 10-15% tissues, revealing that higher levels of ERBB2 and lower levels of cases (3). Cervical cancer is frequently caused by the of miR-3184-5p were associated with clinicopathological indi- oncovirus human papillomavirus (HPV), mainly by types cators of cervical cancer progression. -

RASSF1A Interacts with and Activates the Mitotic Kinase Aurora-A
Oncogene (2008) 27, 6175–6186 & 2008 Macmillan Publishers Limited All rights reserved 0950-9232/08 $32.00 www.nature.com/onc ORIGINAL ARTICLE RASSF1A interacts with and activates the mitotic kinase Aurora-A L Liu1, C Guo1, R Dammann2, S Tommasi1 and GP Pfeifer1 1Division of Biology, Beckman Research Institute, City of Hope Cancer Center, Duarte, CA, USA and 2Institute of Genetics, University of Giessen, Giessen, Germany The RAS association domain family 1A (RASSF1A) gene tumorigenesis and carcinogen-induced tumorigenesis is located at chromosome 3p21.3 within a specific area of (Tommasi et al., 2005; van der Weyden et al., 2005), common heterozygous and homozygous deletions. RASS- supporting the notion that RASSF1A is a bona fide F1A frequently undergoes promoter methylation-asso- tumor suppressor. However, it is not fully understood ciated inactivation in human cancers. Rassf1aÀ/À mice how RASSF1A is involved in tumor suppression. are prone to both spontaneous and carcinogen-induced The biochemical function of the RASSF1A protein is tumorigenesis, supporting the notion that RASSF1A is a largely unknown. The homology of RASSF1A with the tumor suppressor. However, it is not fully understood how mammalian Ras effector novel Ras effector (NORE)1 RASSF1A is involved in tumor suppression pathways. suggests that the RASSF1A gene product may function Here we show that overexpression of RASSF1A inhibits in signal transduction pathways involving Ras-like centrosome separation. RASSF1A interacts with Aurora-A, proteins. However, recent data indicate that RASSF1A a mitotic kinase. Surprisingly, knockdown of RASS- itself binds to RAS only weakly and that binding to F1A by siRNA led to reduced activation of Aurora-A, RAS may require heterodimerization of RASSF1A and whereas overexpression of RASSF1A resulted in in- NORE1 (Ortiz-Vega et al., 2002). -

Side Effects of Targeted Therapy
Side effects of Targeted Therapy Joanne Bird Clare Warnock NIHR Research Fellow Senior Project Nurse Types of Anti Cancer Therapy Biological Therapies Cytotoxic Drugs • Hormone therapies Ongoing research (Chemotherapy) • Goserelin/Zoladex.® • Anti cancer vaccines • Antibiotics • Tamoxifen • Blood cell growth factors • Monoclonal Antibodies • Blood vessel growth • Antimetabolites • Herceptin blockers • Retuximab • IFN/IL2 • Alkylating agents • Bevacizumab (avastin) • Gene therapy • Radioactive substance • Vinca Alkaloids • Cancer growth inhibiters carriers (conjugated MABs) – Tyrosine Kinase Inhibitors • Anthracyclines – Proteasome inhibitors • Drug carriers – mTOR inhibitors – PI3K inhibitors – Histone deacetylase inhibitors – Hedgehog pathway blockers • Pro cytotoxic Drugs • Capecitabine Tyrosine Kinase Inhibitors • How many do you know!!!!! TKIs • Afatanib • Imatinib • Axitinib • Lapatinib • Bosutinib • Nilotinib • Crizotinib • Pazopanib • Dabrafenib • Regorafenib • Dasatinib • Sorafenib • Erlotinib • Sunitinib • Gefitinib • Trametinib Principles • Growth factor receptors play a role on the normal processes of cell growth and development. – In some cancers these growth receptors are over- expressed leading to unregulated cell growth. • Molecular pathways involved in cancer cell proliferation are identified • Drugs are developed to act on these pathways Symptom grading • Standardised assessment – objective – My small and your small may be different! • Effective communication and documentation • Accurate evaluation of new treatments in -

The Self-Inhibitory Nature of Metabolic Networks and Its Alleviation Through Compartmentalization
ARTICLE Received 30 Oct 2016 | Accepted 23 May 2017 | Published 10 Jul 2017 DOI: 10.1038/ncomms16018 OPEN The self-inhibitory nature of metabolic networks and its alleviation through compartmentalization Mohammad Tauqeer Alam1,2, Viridiana Olin-Sandoval1,3, Anna Stincone1,w, Markus A. Keller1,4, Aleksej Zelezniak1,5,6, Ben F. Luisi1 & Markus Ralser1,5 Metabolites can inhibit the enzymes that generate them. To explore the general nature of metabolic self-inhibition, we surveyed enzymological data accrued from a century of experimentation and generated a genome-scale enzyme-inhibition network. Enzyme inhibition is often driven by essential metabolites, affects the majority of biochemical processes, and is executed by a structured network whose topological organization is reflecting chemical similarities that exist between metabolites. Most inhibitory interactions are competitive, emerge in the close neighbourhood of the inhibited enzymes, and result from structural similarities between substrate and inhibitors. Structural constraints also explain one-third of allosteric inhibitors, a finding rationalized by crystallographic analysis of allosterically inhibited L-lactate dehydrogenase. Our findings suggest that the primary cause of metabolic enzyme inhibition is not the evolution of regulatory metabolite–enzyme interactions, but a finite structural diversity prevalent within the metabolome. In eukaryotes, compartmentalization minimizes inevitable enzyme inhibition and alleviates constraints that self-inhibition places on metabolism. 1 Department of Biochemistry and Cambridge Systems Biology Centre, University of Cambridge, 80 Tennis Court Road, Cambridge CB2 1GA, UK. 2 Division of Biomedical Sciences, Warwick Medical School, University of Warwick, Gibbet Hill Road, Coventry CV4 7AL, UK. 3 Department of Food Science and Technology, Instituto Nacional de Ciencias Me´dicas y Nutricio´n Salvador Zubira´n, Vasco de Quiroga 15, Tlalpan, 14080 Mexico City, Mexico. -

The Prevalence of MADH4 and BMPR1A Mutations in Juvenile Polyposis and Absence of BMPR2, BMPR1B, and ACVR1 Mutations
484 ORIGINAL ARTICLE J Med Genet: first published as 10.1136/jmg.2004.018598 on 2 July 2004. Downloaded from The prevalence of MADH4 and BMPR1A mutations in juvenile polyposis and absence of BMPR2, BMPR1B, and ACVR1 mutations J R Howe, M G Sayed, A F Ahmed, J Ringold, J Larsen-Haidle, A Merg, F A Mitros, C A Vaccaro, G M Petersen, F M Giardiello, S T Tinley, L A Aaltonen, H T Lynch ............................................................................................................................... J Med Genet 2004;41:484–491. doi: 10.1136/jmg.2004.018598 Background: Juvenile polyposis (JP) is an autosomal dominant syndrome predisposing to colorectal and gastric cancer. We have identified mutations in two genes causing JP, MADH4 and bone morphogenetic protein receptor 1A (BMPR1A): both are involved in bone morphogenetic protein (BMP) mediated signalling and are members of the TGF-b superfamily. This study determined the prevalence of mutations See end of article for in MADH4 and BMPR1A, as well as three other BMP/activin pathway candidate genes in a large number authors’ affiliations ....................... of JP patients. Methods: DNA was extracted from the blood of JP patients and used for PCR amplification of each exon of Correspondence to: these five genes, using primers flanking each intron–exon boundary. Mutations were determined by Dr J R Howe, Department of Surgery, 4644 JCP, comparison to wild type sequences using sequence analysis software. A total of 77 JP cases were University of Iowa College sequenced for mutations in the MADH4, BMPR1A, BMPR1B, BMPR2, and/or ACVR1 (activin A receptor) of Medicine, 200 Hawkins genes. The latter three genes were analysed when MADH4 and BMPR1A sequencing found no mutations. -

942.Full.Pdf
Original Article Opposite Effect of JAK2 on Insulin-Dependent Activation of Mitogen-Activated Protein Kinases and Akt in Muscle Cells Possible Target to Ameliorate Insulin Resistance Ana C.P. Thirone, Lellean JeBailey, Philip J. Bilan, and Amira Klip Many cytokines increase their receptor affinity for Janus kinases (JAKs). Activated JAK binds to signal transducers and activators of transcription, insulin receptor substrates olypeptides such as erythropoietin, prolactin, (IRSs), and Shc. Intriguingly, insulin acting through its leptin, angiotensin, growth hormone, most inter- own receptor kinase also activates JAK2. However, the leukins, and interferon-␥ bind to receptors that impact of such activation on insulin action remains un- Plack intrinsic kinase activity, recruiting and acti- known. To determine the contribution of JAK2 to insulin vating cytoplasmic tyrosine kinases of the Janus family signaling, we transfected L6 myotubes with siRNA against (JAK) consisting of JAK1, JAK2, JAK3, and Tyk2 (1–3). JAK2 (siJAK2), reducing JAK2 protein expression by 75%. Activated JAK phosphorylates tyrosine residues within Insulin-dependent phosphorylation of IRS1/2 and Shc was not affected by siJAK2, but insulin-induced phosphoryla- itself and the associated receptor forming high-affinity tion of the mitogen-activated protein kinases (MAPKs) binding sites for a variety of signaling proteins containing Src homology 2 and other phosphotyrosine-binding do- extracellular signal–related kinase, p38, and Jun NH2- terminal kinase and their respective upstream kinases mains, including signal transducers and activators of tran- MKK1/2, MKK3/6, and MKK4/7 was significantly lowered scription, insulin receptor substrates (IRSs), and the when JAK2 was depleted, correlating with a significant adaptor protein Shc (1–4). -

Stimulating the Expression of Sphingosine Kinase 1 (Sphk1) Is Bene�Cial to Reduce Acrylamide-Induced Nerve Cell Damage
Stimulating the Expression of Sphingosine Kinase 1 (SphK1) is Benecial to Reduce Acrylamide-Induced Nerve Cell Damage Yong-Hui Wu ( [email protected] ) Harbin Medical University https://orcid.org/0000-0002-4838-2947 Sheng-Yuan Wang Harbin Medical University Xiao-Li Wang Harbin Medical University Rui Xin Harbin Medical University Ye Xin Harbin Medical University Rui Wang Harbin Medical University Kun Ma Harbin Medical University Cui-Ping Yu Harbin Medical University Dan Zhang Harbin Medical University Xiao-Rong Zhou Harbin Medical University Wei-Wei Ma Harbin Medical University Chao Wang Harbin Medical University Research Keywords: Acrylamide, SphKl, Neurotoxicity, Apoptosis, MAPK pathway Posted Date: September 28th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-80914/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Stimulating the expression of sphingosine kinase 1 (SphK1) is beneficial to reduce acrylamide-induced nerve cell damage Sheng-Yuan Wang1, Xiao-Li Wang1, Rui Xin1, Ye Xin1, Rui Wang1, Kun Ma2, Cui-Ping Yu1, Dan Zhang1, Xiao-Rong Zhou1, Wei-Wei Ma3, Chao Wang4, Yong-Hui Wu1* 1 Department of Occupational Health, Public Health College, Harbin Medical University, Harbin, P. R. 2 Department of Hygienic Toxicology, Public Health College, Harbin Medical University, Harbin, P. R. 3 Harbin Railway Center for Disease Control and Prevention, Harbin, P. R. 4 Health Commission of Heilongjiang Province. * Address correspondence to this author at: The Department of Occupational Health, Public Health College, Harbin Medical University, 157 Baojian Road, Nan gang District, Harbin, People’s Republic of China 150086. Phone: +86-451-8750-2827, Fax: +86-451-8750-2827, E-mail: [email protected]. -

JAK Inhibitors for Treatment of Psoriasis: Focus on Selective TYK2 Inhibitors
Drugs https://doi.org/10.1007/s40265-020-01261-8 CURRENT OPINION JAK Inhibitors for Treatment of Psoriasis: Focus on Selective TYK2 Inhibitors Miguel Nogueira1 · Luis Puig2 · Tiago Torres1,3 © Springer Nature Switzerland AG 2020 Abstract Despite advances in the treatment of psoriasis, there is an unmet need for efective and safe oral treatments. The Janus Kinase– Signal Transducer and Activator of Transcription (JAK–STAT) pathway plays a signifcant role in intracellular signalling of cytokines of numerous cellular processes, important in both normal and pathological states of immune-mediated infamma- tory diseases. Particularly in psoriasis, where the interleukin (IL)-23/IL-17 axis is currently considered the crucial pathogenic pathway, blocking the JAK–STAT pathway with small molecules would be expected to be clinically efective. However, relative non-specifcity and low therapeutic index of the available JAK inhibitors have delayed their integration into the therapeutic armamentarium of psoriasis. Current research appears to be focused on Tyrosine kinase 2 (TYK2), the frst described member of the JAK family. Data from the Phase II trial of BMS-986165—a selective TYK2 inhibitor—in psoriasis have been published and clinical results are encouraging, with a large Phase III programme ongoing. Further, the selective TYK2 inhibitor PF-06826647 is being tested in moderate-to-severe psoriasis in a Phase II clinical trial. Brepocitinib, a potent TYK2/JAK1 inhibitor, is also being evaluated, as both oral and topical treatment. Results of studies with TYK2 inhibitors will be important in assessing the clinical efcacy and safety of these drugs and their place in the therapeutic armamentarium of psoriasis.