TOPIC 2. Airway Patency Impairment. First Aid. Lesson 2 1. Anatomical and Physiological Features of the Respiratory Tract. 2. D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
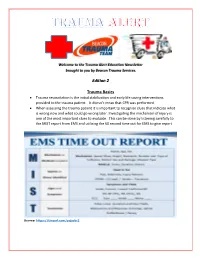
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Approach to the Trauma Patient Will Help Reduce Errors
The Approach To Trauma Author Credentials Written by: Nicholas E. Kman, MD, The Ohio State University Updated by: Creagh Boulger, MD, and Benjamin M. Ostro, MD, The Ohio State University Last Update: March 2019 Case Study “We have a motor vehicle accident 5 minutes out per EMS report.” 47-year-old male unrestrained driver ejected 15 feet from car arrives via EMS. Vital Signs: BP: 100/40, RR: 28, HR: 110. He was initially combative at the scene but now difficult to arouse. He does not open his eyes, withdrawals only to pain, and makes gurgling sounds. EMS placed a c-collar and backboard, but could not start an IV. What do you do? Objectives Upon completion of this self-study module, you should be able to: ● Describe a focused rapid assessment of the trauma patient using an organized primary and secondary survey. ● Discuss the components of the primary survey. ● Discuss possible pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures. ● Describe how to stabilize a trauma patient and prioritize resuscitative measures. ● Discuss the secondary survey with particular attention to head/central nervous system (CNS), cervical spine, chest, abdominal, and musculoskeletal trauma. ● Discuss appropriate labs and diagnostic testing in caring for a trauma patient. ● Describe appropriate disposition of a trauma patient. Introduction Nearly 10% of all deaths in the world are caused by injury. Trauma is the number one cause of death in persons 1-50 years of age and results in significant life years lost. According to the National Trauma Data Bank, falls were the leading cause of trauma followed by motor vehicle collisions (MVCs) and firearm related injuries with an overall mortality rate of 4.39% in 2016. -

Clinical Presentation of Patients with Tension Pneumothorax a Systematic Review
META-ANALYSIS Clinical Presentation of Patients With Tension Pneumothorax A Systematic Review Derek J. Roberts, MD,∗†‡§ Simon Leigh-Smith, MBChB,¶ Peter D. Faris, PhD,† Christopher Blackmore, MD,∗ Chad G. Ball, MD, MSc,∗§∗∗ Helen Lee Robertson, MLIS,†† Elijah Dixon, MD, MSc,∗∗∗ Matthew T. James, MD, PhD,†‡‡ Andrew W. Kirkpatrick, MD, MHSc,∗‡§ John B. Kortbeek, MD,∗‡§ and Henry T. Stelfox, MD, PhD†‡‡‡ assisted ventilation who experienced hypotension or cardiac arrest developed Objective: To determine whether the reported clinical presentation of tension these signs within minutes of clinical presentation. pneumothorax differs between patients who are breathing unassisted versus Discussion: The reported clinical presentation of tension pneumothorax de- receiving assisted ventilation. pends on the ventilatory status of the patient. This may have implications for Background: Animal studies suggest that the pathophysiology and physical improving the diagnosis and treatment of this life-threatening disorder. signs of tension pneumothorax differ by subject ventilatory status. Methods: We searched electronic databases through to October 15, 2013 for Keywords: assisted ventilation, breathing unassisted, clinical manifestations, observational studies and case reports/series reporting clinical manifestations clinical presentation, diagnosis, management, signs and symptoms, tension of tension pneumothorax. Two physicians independently extracted clinical pneumothorax manifestations reported at diagnosis. (Ann Surg 2014;00:1–11) Results: We identified 5 cohort studies (n = 310 patients) and 156 case series/reports of 183 cases of tension pneumothorax (n = 86 breathing unas- sisted, n = 97 receiving assisted ventilation). Hypoxia was reported among 43 ension pneumothorax is an uncommon condition with a high (50.0%) cases of tension pneumothorax who were breathing unassisted versus mortality rate most frequently reported to occur in prehospital, 89 (91.8%) receiving assisted ventilation (P < 0.001). -

Head to Toe Critical Care Assessment for the Trauma Patient
Head to Toe Assessment for the Trauma Patient St. Joseph Medical Center – Tacoma General Hospital – Trauma Trust Objectives 1. Learn Focused Trauma Assessment 2. Learn Frequently Seen Trauma Injuries 3. Appropriate Nursing Care for Trauma Patients St. Joseph Medical Center – Tacoma General Hospital – Trauma Trust Prior to Arrival • Ensure staff have received available details of the case • Notify the entire responding Trauma team • Assign tasks as appropriate for Trauma resuscitation • Gather, check and prepare equipment • Prepare Trauma room • Don PPE (personal protective equipment) • MIVT way to obtain history: Mechanism of injury Injuries sustained Vital signs Treatment given Trauma Trust St. Joseph Medical Center – Tacoma General Hospital – Trauma Trust Primary Survey • Begins immediately on patient’s arrival • Collection of information of injury event and past medical history depend on severity of condition • Conducted in Emergency Room simultaneously with resuscitation • Focuses on detecting life threatening injuries • Assessment of ABC’s Trauma Trust St. Joseph Medical Center – Tacoma General Hospital – Trauma Trust Primary Survey Components Airway with simultaneous c-spine protection and Alertness Breathing and ventilation Circulation and Control of hemorrhage Disability – Neurological: Glasgow Coma Scale [GCS] or Alert, Voice, Pain, Unresponsive [AVPU] Exposure and Environmental Controls Full set of vital signs and Family presence Get resuscitation adjuncts (labs, monitoring, naso/oro gastric tube, oxygenation and pain) -

28 Thoracentesis (Assist) 223
PROCEDURE Thoracentesis (Assist) 28 Susan Yeager PURPOSE: Thoracentesis is performed to assist in the diagnosis and therapeutic management of patients with pleural effusions. PREREQUISITE NURSING hypotension, cough, pain, visceral injury, and reexpansion 4–6 KNOWLEDGE pulmonary edema. • The most common complications from pleural aspiration • Thoracentesis is performed with insertion of a needle or are pneumothorax, pain, hemorrhage, and procedure a catheter into the pleural space, which allows for removal failure. The most serious complication is visceral injury. 5 of pleural fl uid. • Hypotension can occur as part of the vasovagal reaction, • Pleural effusions are defi ned as the accumulation of fl uid causing bradycardia, during or hours after the procedure. in the pleural space that exceeds 10 mL and results from If it occurs during the procedure, cessation of the proce- the overproduction of fl uid or disruption in fl uid dure and intravenous (IV) atropine may be necessary. If reabsorption. 1 hypotension occurs after the procedure, it is likely the • Diagnostic thoracentesis is indicated for differential diag- result of fl uid shifting from pleural effusion reaccumula- nosis for patients with pleural effusion of unknown etiol- tion. In this situation, the patient is likely to respond to ogy. A diagnostic thoracentesis may be repeated if initial fl uid resuscitation. 7 results fail to yield a diagnosis. • Development of cough generally initiates toward the • Therapeutic thoracentesis is indicated to relieve the symp- end of the procedure and should result in procedure toms (e.g., dyspnea, cough, hypoxemia, or chest pain) cessation. caused by a pleural effusion. • Reexpansion pulmonary edema is thought to occur from • Samples of pleural fl uid are analyzed and assist in distin- overdraining of fl uid too quickly. -

Difficult Endotracheal Intubation Secondary to Tracheal Deviation And
Case Report pISSN 2005-6419 • eISSN 2005-7563 KJA Difficult endotracheal intubation Korean Journal of Anesthesiology secondary to tracheal deviation and stenosis in a patient with severe kyphoscoliosis -a case report- Hyun Jung Kim1, Yun Suk Choi1, Sang Hyun Park1, and Jun-ho Jo2 Department of Anesthesiology and Pain Medicine, 1Jeju National University School of Medicine, Jeju, 2Veterans Health Medical Center, Seoul, Korea We report on a case of difficult endotracheal intubation in a patient with marked tracheal deviation at an angle of 90 degrees combined with stenosis due to kyphoscoliosis with vertebral body fusion. After induction of general anesthesia, a proper laryngeal view was easily obtained using a videolaryngoscope. But a tracheal tube could not be advanced more than 3 cm beyond the vocal cords due to resistance, despite various attempts, including the use of small size tubes, full rotation of the tube tip, and fiberoptic bronchoscopy. Ultimately, the airway was successfully secured by placing a tube tip above the area of resistance and by additionally packing saline-soaked gauzes around the tracheal inlet to minimize gas leakage and to fasten the tube in the trachea. Key Words: Intubation, Kyphosis, Scoliosis, Tracheal disease. Anesthesia can be difficult in patients with severe kypho- We would like to report a case of difficult intubation with which scoliosis due to respiratory failure or distortion of the airway we were recently involved. anatomy. Several cases about anesthetic management in patients with severe kyphoscoliosis have been reported previously [1-3]. Case Report However, there is little information about the airway manage- ment of marked tracheal deviation at an angle of 90 degrees A 60-year-old woman, 135 cm in height and 39 kg in weight, combined with stenosis in patients with this kind of disorder. -

Interactive Lecture (1) ✓ Important ✓ Notes ✓ Extra Radiology of Cardiorespiratory Disease Editting File
MED437 King Saud University Color Index: Interactive lecture (1) ✓ Important ✓ Notes ✓ Extra Radiology of cardiorespiratory disease Editting File Done by: Alanoud Salman Dawood Ismail Revised by: Yazeed Al-Dossare Refresh your memory Label the structures Label the structures Anterior-posterior & PA are called frontal (We are not sure if it is AP or PA view) view For better understanding All the explanation by dr. Aljurayyan in one place Differential diagnosis for the abnormal white Differential diagnosis for the abnormal black (Hyperdense) abnormalities on the radiograph: (Hypodense) abnormalities on the radiograph: 1- Pleural effusion. 1- Emphysema. Check the costophrenic angle, is it sharp or blunted? Barrel chest (No change in width between the apex and Look for meniscus sign. (Crescent). base of the lung). You can still see some soft tissue (Bronchioles). 2- Lung collapse (Atelectasis). Is there a wedge sign on the lateral view X-ray? 2- Pneumothorax. tracheal deviation + reduced lung volume Super black tissues, no soft tissues at all. 3- Mass. Does the opacity have well demarcated margins? 4- Infiltration/consolidation Rare. ill-defined border Remember: The history helps a lot, so a history with smoking make us think of a tumor, and history of DVT make us think of PE, and malignancies usually does not present with fever. 30 year-old with fever 30 year-old with fever - Is it a mass or infiltration? - Which lung lobe is affected? 30 year-old with fever Key feature of infiltration = RUL white area with ill-defined borders Abnormal RML Added density RLL We need the lateral view to localize the lesion - White abnormality. -

Atelectasis in Children
INDIAN PEDIATRICS VOLUME 35-MAY 1998 ATELECTASIS IN CHILDREN T.S. Raghu Raman, Sunil Mathew, Ravikumar and P.S. Garcha From the Departments of Pediatrics, Otorhinolaryngology and Anesthesia, Armed Forces Medical College, Punc-411 040. Reprint requests: Wg. Cdr. T.S. Raghu Rarnan, Associate Professor, Department of Pediatrics, AFMC, Pune 411 040. Manuscript received: July 1,1997; Initial review completed: August 27,1997; Revision accepted: November 27,1997. Background: In children with lower respiratory tract symptoms, the elicited signs are not enough to distinguish common diagnosis like pneumonic consolidation, foreign body aspiration and atelectasis. Radiology and bronchoscopy would identify the true nature of the etiology. Design: Prospective study. Subjects: Thirty five children with both acute and chronic lower respiratory tract symptomatology, were analyzed for clinical and radiological signs of atelectasis. Results: There were 23 cases in the acute group and 12 in chronic group. Acute group included cases of pneumonia, foreign body aspiration and mucus plug syndrome. Chronic group included cases of congenital heart disease, endobronchial tuberculosis and bronchial stenosis. Clinical recognition of atelectasis on the basis of localized loss of breath sounds and mediastinal shift was seen only in a minority of cases (8/35). The presence of atelectasis in children with pneumonia, missed clinically were diagnosed by the presence of tracheal shift, elevated hemidiaphragm and silhouette sign. In 21 cases, silhouette sign was positive making it an important radiological sign. Twenty one children underwent either diagnostic or/and therapeutic bronchoscopy. Findings included foreign bodies (n = 5), mucus plugs (n = 4), narrowing of main bronchus (n = 4) and inflammatory mucoid secretions and narrowing of lumen (n = 8). -

Path Pulmonary Outline
Pathology Pulmonary ATELECTASIS Neonatal Atelectasis ‐ The lungs of the neonate never inflate, a consequence of congenital defect, premature birth (insufficient surfactant), or other consequence, also called Patchy Atelectasis Adult or Acquired Atelectasis ‐ Collapse of Previously Inflated lung, creating areas of “airless parenchyma” ‐ Produces a well‐perfused but poorly‐ventilated region, predisposing for infection Decreased Volume ‐ Is a reversible disorder (except in the case of contraction) outside pleural space ‐ Resorption Atelectasis o Consequence of complete obstruction without impairment to blood flow Blockage o A decreased lung volume results in a mediastinal shift towards affected lung o Caused by a mucous plug associated with Asthma, Bronchitis, or Aspiration Pneumonia ‐ Compression Atelectasis o Consequence of partially or totally filled pleura with exudate (CHF), tumor, air (pneumothorax), blood (hemothorax), when air pressure threatens the function of lungs and great vessels (tension pneumothorax), or with an extra‐pulmonary mass compressing Something within lung parenchyma. pleural space compressing o Compressed lung tissue cannot expand and is therefore poorly ventilated. parenchyma o Compression pushes lung resulting in a mediastinal shift away from affected lung ‐ Contraction Atelectasis o Fibrotic changes prevent expansion, resulting in reduced lung volume and ventilation Fibrotic o This form is irreversible Changes are Irreversible PULMONARY EDEMA Pulmonary Edema is simply the accumulation of fluid in the alveolar