Head to Toe Critical Care Assessment for the Trauma Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spinal Cord Injury and Traumatic Brain Injury Research Grant Program Report 2020
This document is made available electronically by the Minnesota Legislative Reference Library as part of an ongoing digital archiving project. http://www.leg.state.mn.us/lrl/lrl.asp Spinal Cord Injury and Traumatic Brain Injury Research Grant Program Report January 15, 2020 Author About the Minnesota Office of Higher Education Alaina DeSalvo The Minnesota Office of Higher Education is a Competitive Grants Administrator cabinet-level state agency providing students with Tel: 651-259-3988 financial aid programs and information to help [email protected] them gain access to postsecondary education. The agency also serves as the state’s clearinghouse for data, research and analysis on postsecondary enrollment, financial aid, finance and trends. The Minnesota State Grant Program is the largest financial aid program administered by the Office of Higher Education, awarding up to $207 million in need-based grants to Minnesota residents attending eligible colleges, universities and career schools in Minnesota. The agency oversees other state scholarship programs, tuition reciprocity programs, a student loan program, Minnesota’s 529 College Savings Plan, licensing and early college awareness programs for youth. Minnesota Office of Higher Education 1450 Energy Park Drive, Suite 350 Saint Paul, MN 55108-5227 Tel: 651.642.0567 or 800.657.3866 TTY Relay: 800.627.3529 Fax: 651.642.0675 Email: [email protected] Table of Contents Introduction 1 Spinal Cord Injury and Traumatic Brain Injury Advisory Council 1 FY 2020 Proposal Solicitation Schedule -

Internal Bleeding
Internal bleeding What is internal bleeding? It is a leakage of blood from the blood vessels of the surrounding tissues because of an injury affect the vessels and lead to rupture. Internal bleeding occurs inside the body cavities such as the head, chest, abdomen, or eye, and it is difficult to detect, because the leaked blood cannot be seen, and the person may not feel its occurrence till the symptoms associated with that bleeding start to appear. Note: It should be noted that people who take anticoagulant drugs are more likely to have this bleeding than others. What are symptoms of abdominal internal bleeding? There are many symptoms developed by the patients of internal bleeding in the abdomen or chest as below: • Feeling of pain in the abdomen. • Shortness of breath. • Feeling of chest pain. • Dizziness upon standing. • Bruises around the navel or on both sides of the abdomen. • Nausea, Vomiting. • Blood in urine. • Dark color stool. What are the symptoms of abdominal internal bleeding? Sometimes, internal bleeding may lead to loss of large amounts of blood, and in this case, the patient will have many symptoms, as below: • Accelerated heart beats • Low blood pressure • Skin sweating • General weakness • Feeling lethargic or feeling sleepy When should I go to seek medical care? Internal bleeding is very dangerous and life threatening and you should visit the doctor when experience one of the following cases:: ✓ After exposure to a severe injury, to ensure that there is no internal bleeding. ✓ Feeling severe pain in the abdomen ✓ Feeling acute shortness of breath ✓ feeling dizzy ✓ Seeing a change in vision Note: When these symptoms are noticed, you should go immediately to medical care or you must call the emergency services to avoid death. -
The European Guideline on Management Of
Rossaint et al. Critical Care (2016) 20:100 DOI 10.1186/s13054-016-1265-x RESEARCH Open Access The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition Rolf Rossaint1, Bertil Bouillon2, Vladimir Cerny3,4,5,6, Timothy J. Coats7, Jacques Duranteau8, Enrique Fernández-Mondéjar9, Daniela Filipescu10, Beverley J. Hunt11, Radko Komadina12, Giuseppe Nardi13, Edmund A. M. Neugebauer14, Yves Ozier15, Louis Riddez16, Arthur Schultz17, Jean-Louis Vincent18 and Donat R. Spahn19* Abstract Background: Severe trauma continues to represent a global public health issue and mortality and morbidity in trauma patients remains substantial. A number of initiatives have aimed to provide guidance on the management of trauma patients. This document focuses on the management of major bleeding and coagulopathy following trauma and encourages adaptation of the guiding principles to each local situation and implementation within each institution. Methods: The pan-European, multidisciplinary Task Force for Advanced Bleeding Care in Trauma was founded in 2004 and included representatives of six relevant European professional societies. The group used a structured, evidence-based consensus approach to address scientific queries that served as the basis for each recommendation and supporting rationale. Expert opinion and current clinical practice were also considered, particularly in areas in which randomised clinical trials have not or cannot be performed. Existing recommendations were reconsidered and revised based on new scientific evidence and observed shifts in clinical practice; new recommendations were formulated to reflect current clinical concerns and areas in which new research data have been generated. This guideline represents the fourth edition of a document first published in 2007 and updated in 2010 and 2013. -
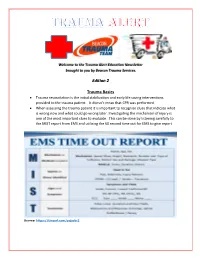
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

Traumatic Brain Injury
REPORT TO CONGRESS Traumatic Brain Injury In the United States: Epidemiology and Rehabilitation Submitted by the Centers for Disease Control and Prevention National Center for Injury Prevention and Control Division of Unintentional Injury Prevention The Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation is a publication of the Centers for Disease Control and Prevention (CDC), in collaboration with the National Institutes of Health (NIH). Centers for Disease Control and Prevention National Center for Injury Prevention and Control Thomas R. Frieden, MD, MPH Director, Centers for Disease Control and Prevention Debra Houry, MD, MPH Director, National Center for Injury Prevention and Control Grant Baldwin, PhD, MPH Director, Division of Unintentional Injury Prevention The inclusion of individuals, programs, or organizations in this report does not constitute endorsement by the Federal government of the United States or the Department of Health and Human Services (DHHS). Suggested Citation: Centers for Disease Control and Prevention. (2015). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention. Atlanta, GA. Executive Summary . 1 Introduction. 2 Classification . 2 Public Health Impact . 2 TBI Health Effects . 3 Effectiveness of TBI Outcome Measures . 3 Contents Factors Influencing Outcomes . 4 Effectiveness of TBI Rehabilitation . 4 Cognitive Rehabilitation . 5 Physical Rehabilitation . 5 Recommendations . 6 Conclusion . 9 Background . 11 Introduction . 12 Purpose . 12 Method . 13 Section I: Epidemiology and Consequences of TBI in the United States . 15 Definition of TBI . 15 Characteristics of TBI . 16 Injury Severity Classification of TBI . 17 Health and Other Effects of TBI . -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Symptomatic Intracranial Hemorrhage (Sich) and Activase® (Alteplase) Treatment: Data from Pivotal Clinical Trials and Real-World Analyses
Symptomatic intracranial hemorrhage (sICH) and Activase® (alteplase) treatment: Data from pivotal clinical trials and real-world analyses Indication Activase (alteplase) is indicated for the treatment of acute ischemic stroke. Exclude intracranial hemorrhage as the primary cause of stroke signs and symptoms prior to initiation of treatment. Initiate treatment as soon as possible but within 3 hours after symptom onset. Important Safety Information Contraindications Do not administer Activase to treat acute ischemic stroke in the following situations in which the risk of bleeding is greater than the potential benefit: current intracranial hemorrhage (ICH); subarachnoid hemorrhage; active internal bleeding; recent (within 3 months) intracranial or intraspinal surgery or serious head trauma; presence of intracranial conditions that may increase the risk of bleeding (e.g., some neoplasms, arteriovenous malformations, or aneurysms); bleeding diathesis; and current severe uncontrolled hypertension. Please see select Important Safety Information throughout and the attached full Prescribing Information. Data from parts 1 and 2 of the pivotal NINDS trial NINDS was a 2-part randomized trial of Activase® (alteplase) vs placebo for the treatment of acute ischemic stroke. Part 1 (n=291) assessed changes in neurological deficits 24 hours after the onset of stroke. Part 2 (n=333) assessed if treatment with Activase resulted in clinical benefit at 3 months, defined as minimal or no disability using 4 stroke assessments.1 In part 1, median baseline NIHSS score was 14 (min: 1; max: 37) for Activase- and 14 (min: 1; max: 32) for placebo-treated patients. In part 2, median baseline NIHSS score was 14 (min: 2; max: 37) for Activase- and 15 (min: 2; max: 33) for placebo-treated patients. -

NIH Public Access Author Manuscript J Neuropathol Exp Neurol
NIH Public Access Author Manuscript J Neuropathol Exp Neurol. Author manuscript; available in PMC 2010 September 24. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Neuropathol Exp Neurol. 2009 July ; 68(7): 709±735. doi:10.1097/NEN.0b013e3181a9d503. Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy following Repetitive Head Injury Ann C. McKee, MD1,2,3,4, Robert C. Cantu, MD3,5,6,7, Christopher J. Nowinski, AB3,5, E. Tessa Hedley-Whyte, MD8, Brandon E. Gavett, PhD1, Andrew E. Budson, MD1,4, Veronica E. Santini, MD1, Hyo-Soon Lee, MD1, Caroline A. Kubilus1,3, and Robert A. Stern, PhD1,3 1 Department of Neurology, Boston University School of Medicine, Boston, Massachusetts 2 Department of Pathology, Boston University School of Medicine, Boston, Massachusetts 3 Center for the Study of Traumatic Encephalopathy, Boston University School of Medicine, Boston, Massachusetts 4 Geriatric Research Education Clinical Center, Bedford Veterans Administration Medical Center, Bedford, Massachusetts 5 Sports Legacy Institute, Waltham, MA 6 Department of Neurosurgery, Boston University School of Medicine, Boston, Massachusetts 7 Department of Neurosurgery, Emerson Hospital, Concord, MA 8 CS Kubik Laboratory for Neuropathology, Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts Abstract Since the 1920s, it has been known that the repetitive brain trauma associated with boxing may produce a progressive neurological deterioration, originally termed “dementia pugilistica” and more recently, chronic traumatic encephalopathy (CTE). We review the 47 cases of neuropathologically verified CTE recorded in the literature and document the detailed findings of CTE in 3 professional athletes: one football player and 2 boxers. -

Patient Assessment?
EMERGENCY MEDICAL TECHNICIAN ‐ BASIC What is Patient Assessment? Why is Patient Assessment important? MECTA EMS Learning Assistant 2 What are the phases of patient assessment? Review of Dispatch Information Scene Survey Initial Assessment Focused History and Physical Exam Detailed Physical Exam Ongoing Assessment Communication Documentation MECTA EMS Learning Assistant 3 Why is the order of Patient Assessment important? Why is it necessary to develop a method of assessment and use that method on all patients? MECTA EMS Learning Assistant 4 SCENE SIZE‐UP INITIAL ASSESSMENT Trauma FOCUSED HISTORY & FOCUSED HISTORY & PHYSICAL EXAM PHYSICAL EXAM Patient Patient DETAILED DETAILED PHYSICAL EXAM PHYSICAL EXAM Medical ON‐GOING ASSESSMENT MECTA EMS Learning Assistant 5 Begin with receipt of call Location Incident Injured/Injuries MECTA EMS Learning Assistant 6 Continue En Route Further info from dispatcher Observe ▪ Smoke? ▪ Fire? ▪ High line wires? ▪ Railroads? ▪ Water? ▪ Industry? ▪ Other Public Safety units? MECTA EMS Learning Assistant 7 Upon Arrival Observe ▪ Overall scene ▪ Location of victim(s) ▪ Possible Mechanisms of Injury MECTA EMS Learning Assistant 8 Upon Arrival Observe ▪ Hazards ▪ Crowds ▪ HazMat ▪ Electricity ▪ Gas ▪ Fire ▪ Glass ▪ Jagged metal ▪ Stability of environment ▪ Traffic ▪ Environment MECTA EMS Learning Assistant 9 Ensure Safety ▪ Yourself ▪ Partner ▪ Other rescuers/Bystanders ▪ Patient MECTA EMS Learning Assistant 10 Call for assistance ▪ Other EMS Units ▪ Law Enforcement ▪ Fire Department ▪ -
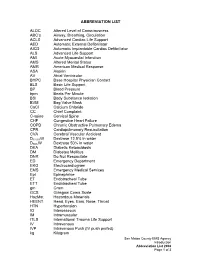
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt.