Path Pulmonary Outline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Edition 2 Trauma Basics
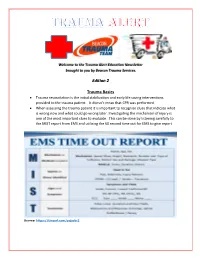
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

USMLE – What's It
Purpose of this handout Congratulations on making it to Year 2 of medical school! You are that much closer to having your Doctor of Medicine degree. If you want to PRACTICE medicine, however, you have to be licensed, and in order to be licensed you must first pass all four United States Medical Licensing Exams. This book is intended as a starting point in your preparation for getting past the first hurdle, Step 1. It contains study tips, suggestions, resources, and advice. Please remember, however, that no single approach to studying is right for everyone. USMLE – What is it for? In order to become a licensed physician in the United States, individuals must pass a series of examinations conducted by the National Board of Medical Examiners (NBME). These examinations are the United States Medical Licensing Examinations, or USMLE. Currently there are four separate exams which must be passed in order to be eligible for medical licensure: Step 1, usually taken after the completion of the second year of medical school; Step 2 Clinical Knowledge (CK), this is usually taken by December 31st of Year 4 Step 2 Clinical Skills (CS), this is usually be taken by December 31st of Year 4 Step 3, typically taken during the first (intern) year of post graduate training. Requirements other than passing all of the above mentioned steps for licensure in each state are set by each state’s medical licensing board. For example, each state board determines the maximum number of times that a person may take each Step exam and still remain eligible for licensure. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

The Nature of Storage Iron in Idiopathic Hemochromatosis and in Hemosiderosis
THE NATURE OF STORAGE IRON IN IDIOPATHIC HEMOCHROMATOSIS AND IN HEMOSIDEROSIS ELECTRON OPTICAL, CHEMICAL, AND SEROLOGIC STUDIES ON ISOLATED HEMOSIDERIN GRANULES* BY GOETZ W. RICHTER, M.D. (From the Department of Pathology, Cornell University Medical College, New York) PLATES 47 TO 51 (Received for publication, April 21, 1960) Although ferritin has long been recognized as an important iron storage compound and as an intermediary in normal iron metabolism, its role in idiopathic hemochromatosis and in secondary hemosiderosis is still unkuown. Diverse means have been employed to gain more knowledge on the pathway of iron in these conditions, and numerous publications attest the difficulties inherent in trying to distinguish between normal and abnormal storage of iron in cells of various sorts. Histochemical studies have provided evidence that inorganic compounds of iron stored in cells as hemosiderin are combined with an organic carrier substance that contains variable quantities of protein, lipid, and carbohydrate (1, 2). Results of chemical analyses led Ludewig to emphasize the heterogeneity of hemosiderin granules (3); his findings have provided qualitative and quantitative data on the carbohydrate, lipid, protein, and iron content of various hemosiderin preparations. The term "hemosiderin" has been used rather loosely; generally it refers to granules that are visible in the light micro- scope, brown when unstained, and give a positive Prussian blue test. Iron that gives a positive Prussian blue test with potassium ferrocyanide without the previous application of oxidizing agents must be in the trivalent (ferric) state. This is true of the bulk of iron in hemosiderin granules; it is also true of the iron hydroxide present in ferritin (4, 5, 7). -

Visualization of Microbleeds with Optical Histology in Mouse Model of Cerebral Amyloid Angiopathy
Microvascular Research 105 (2016) 109–113 Contents lists available at ScienceDirect Microvascular Research journal homepage: www.elsevier.com/locate/ymvre Visualization of microbleeds with optical histology in mouse model of cerebral amyloid angiopathy Patrick Lo a,b, Christian Crouzet a,b, Vitaly Vasilevko c,1,BernardChoia,b,d,⁎,1 a Beckman Laser Institute and Medical Clinic, University of California, Irvine, 1002 Health Sciences Road East, Irvine, CA 92612, USA b Department of Biomedical Engineering, University of California, Irvine, 3120 Natural Sciences II, Irvine, CA 92697, USA c Institute for Memory Impairments and Neurological Disorders, University of California, Irvine, 1207 Gillespie NRF, Irvine, CA 92697-4540, USA d Edwards Lifesciences Center for Advanced Cardiovascular Technology, University of California, Irvine, 2400 Engineering Hall, Irvine, CA 92697, USA article info abstract Article history: Cerebral amyloid angiopathy (CAA) is a neurovascular disease that is strongly associated with an increase in the Received 14 May 2015 number and size of spontaneous microbleeds. Conventional methods of magnetic resonance imaging for detec- Revised 3 February 2016 tion of microbleeds, and positron emission tomography with Pittsburgh Compound B imaging for amyloid Accepted 4 February 2016 deposits, can separately demonstrate the presence of microbleeds and CAA in affected brains in vivo;however, Available online 10 February 2016 there still is a critical need for strong evidence that shows involvement of CAA in microbleed formation. Here, we show in a Tg2576 mouse model of Alzheimer's disease, that the combination of histochemical staining and Keywords: Intracerebral hemorrhage an optical clearing method called optical histology, enables simultaneous, co-registered three-dimensional visu- DiI alization of cerebral microvasculature, microbleeds, and amyloid deposits. -

Brain Metastasis from Unknown Primary Tumour: Moving from Old Retrospective Studies to Clinical Trials on Targeted Agents
cancers Review Brain Metastasis from Unknown Primary Tumour: Moving from Old Retrospective Studies to Clinical Trials on Targeted Agents Roberta Balestrino 1,* , Roberta Rudà 2,3 and Riccardo Soffietti 3 1 Department of Neuroscience, University of Turin, Via Cherasco 15, 10121 Turin, Italy 2 Department of Neurology, Castelfranco Veneto/Treviso Hospital, Via dei Carpani, 16/Z, 31033 Castelfranco Veneto, Italy; [email protected] 3 Department of Neuro-Oncology, University of Turin, Via Cherasco 15, 10121 Turin, Italy; riccardo.soffi[email protected] * Correspondence: [email protected] Received: 13 October 2020; Accepted: 9 November 2020; Published: 12 November 2020 Simple Summary: Brain metastases (BMs) are the most common intracranial tumours in adults and occur up to 3–10 times more frequently than primary brain tumours. In up to 15% of patients with BM, the primary tumour cannot be identified. These cases are known as BM of cancer of unknown primary (CUP) (BM-CUP). The understanding of BM-CUP, despite its relative frequency and unfavourable outcome, is still incomplete and clear indications on management are missing. The aim of this review is to summarize current evidence on the diagnosis and treatment of BM-CUP. Abstract: Brain metastases (BMs) are the most common intracranial tumours in adults and occur up to 3–10 times more frequently than primary brain tumours. BMs may be the cause of the neurological presenting symptoms in patients with otherwise previously undiagnosed cancer. In up to 15% of patients with BMs, the primary tumour cannot be identified. These cases are known as BM of cancer of unknown primary (CUP) (BM-CUP). -

Distribution of Bronchial Gland Measurements in a Jamaican Population
Thorax: first published as 10.1136/thx.24.5.619 on 1 September 1969. Downloaded from Thorax (1969), 24, 619. Distribution of bronchial gland measurements in a Jamaican population J. A. HAYES1 From the Pathology Department, University of the West Indies, Mona, Kingston 7, Jamaica Measurements of the gland thickness and Reid index have been made on bronchi obtained at necropsy on 53 male and 52 female Jamaicans. The mean values for the Reid index and mucous gland thickness obtained were 0-314 and 0O192 mm. for males, and 0-302 and 0l170 mm. for females respectively. No significant increase in value was seen with age, although the data suggest this trend. The results have been compared with data published from Montreal and the same overall Gaussian distribution is seen. This supports the suggestion that the gland measurements in non-bronchitic and bronchitic subjects do- not fall into two distinct groups but are part of a continuous distribution. The similarity of the two studies is also of interest as the populations are drawn from two distinct environments, one from a non-industrialized tropical island, the other from a large city in the northern hemisphere. Bronchial mucous gland enlargement is usually The existing evidence, therefore, indicates that associated with the consistent production of atmospheric pollution is connected with enlarge- copyright. mucoid sputum in chronic bronchitis (Reid, 1958). ment of bronchial mucous glands. It was suggested that this mucosal change could Clinical chronic bronchitis is encountered in be recognized by an increase in the ratio of Jamaica, apparently in the absence of atmospheric mucous gland thickness to thickness of the pollution (Walshe and Hayes, 1967). -

Gas Exchange and Respiratory Function
LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 484 Aptara Gas Exchange and 5 Respiratory Function Applying Concepts From NANDA, NIC, • Case Study and NOC A Patient With Impaired Cough Reflex Mrs. Lewis, age 77 years, is admitted to the hospital for left lower lobe pneumonia. Her vital signs are: Temp 100.6°F; HR 90 and regular; B/P: 142/74; Resp. 28. She has a weak cough, diminished breath sounds over the lower left lung field, and coarse rhonchi over the midtracheal area. She can expectorate some sputum, which is thick and grayish green. She has a history of stroke. Secondary to the stroke she has impaired gag and cough reflexes and mild weakness of her left side. She is allowed food and fluids because she can swallow safely if she uses the chin-tuck maneuver. Visit thePoint to view a concept map that illustrates the relationships that exist between the nursing diagnoses, interventions, and outcomes for the patient’s clinical problems. LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 485 Aptara Nursing Classifications and Languages NANDA NIC NOC NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES INEFFECTIVE AIRWAY CLEARANCE— RESPIRATORY MONITORING— Return to functional baseline sta- Inability to clear secretions or ob- Collection and analysis of patient tus, stabilization of, or structions from the respiratory data to ensure airway patency improvement in: tract to maintain a clear airway and adequate gas exchange RESPIRATORY STATUS: AIRWAY PATENCY—Extent to which the tracheobronchial passages remain open IMPAIRED GAS -

Chest Auscultation: Presence/Absence and Equality of Normal/Abnormal and Adventitious Breath Sounds and Heart Sounds A
Northwest Community EMS System Continuing Education: January 2012 RESPIRATORY ASSESSMENT Independent Study Materials Connie J. Mattera, M.S., R.N., EMT-P COGNITIVE OBJECTIVES Upon completion of the class, independent study materials and post-test question bank, each participant will independently do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Integrate complex knowledge of pulmonary anatomy, physiology, & pathophysiology to sequence the steps of an organized physical exam using four maneuvers of assessment (inspection, palpation, percussion, and auscultation) and appropriate technique for patients of all ages. (National EMS Education Standards) 2. Integrate assessment findings in pts who present w/ respiratory distress to form an accurate field impression. This includes developing a list of differential diagnoses using higher order thinking and critical reasoning. (National EMS Education Standards) 3. Describe the signs and symptoms of compromised ventilations/inadequate gas exchange. 4. Recognize the three immediate life-threatening thoracic injuries that must be detected and resuscitated during the “B” portion of the primary assessment. 5. Explain the difference between pulse oximetry and capnography monitoring and the type of information that can be obtained from each of them. 6. Compare and contrast those patients who need supplemental oxygen and those that would be harmed by hyperoxia, giving an explanation of the risks associated with each. 7. Select the correct oxygen delivery device and liter flow to support ventilations and oxygenation in a patient with ventilatory distress, impaired gas exchange or ineffective breathing patterns including those patients who benefit from CPAP. 8. Explain the components to obtain when assessing a patient history using SAMPLE and OPQRST.