27 Thoracentesis (Perform) 213
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
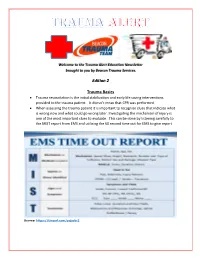
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Acr–Scbt-Mr–Spr–Str Practice Parameter for the Performance of Thoracic Computed Tomography (Ct)
p The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2018 (Resolution 7)* ACR–SCBT-MR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF THORACIC COMPUTED TOMOGRAPHY (CT) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Coding Billing
CodingCoding&Billing FEBRUARY 2020 Quarterly Editor’s Letter Welcome to the February issue of the ATS Coding and Billing Quarterly. There are several important updates about the final Medicare rules for 2020 that will be important for pulmonary, critical care and sleep providers. Additionally, there is discussion of E/M documentation rules that will be coming in 2021 that practices might need some time to prepare for, and as always, we will answer coding, billing and regulatory compliance questions submitted from ATS members. If you are looking for a more interactive way to learn about the 2020 Medicare final rules, there is a webinar on the ATS website that covers key parts of the Medicare final rules. But before we get to all this important information, I have a request for your help. EDITOR ATS Needs Your Help – Recent Invoices for Bronchoscopes and PFT Lab ALAN L. PLUMMER, MD Spirometers ATS RUC Advisor TheA TS is looking for invoices for recently purchased bronchoscopes and ADVISORY BOARD MEMBERS: PFT lab spirometer. These invoices will be used by theA TS to present practice KEVIN KOVITZ, MD expense cost equipment to CMS to help establish appropriate reimbursement Chair, ATS Clinical Practice Committee rates for physician services using this equipment. KATINA NICOLACAKIS, MD Member, ATS Clinical Practice Committee • Invoices should not include education or service contract as those ATS Alternate RUC Advisorr are overhead and cannot be considered by CMS for this portion of the STEPHEN P. HOFFMANN, MD Member, ATS Clinical Practice Committee formula and payment rates. ATS CPT Advisor • Invoices can be up to five years old. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Thoracentesis
The new england journal of medicine videos in clinical medicine Thoracentesis Todd W. Thomsen, M.D., Jennifer DeLaPena, M.D., and Gary S. Setnik, M.D. INDICATIONS From the Department of Emergency Medi- Thoracentesis is a valuable diagnostic procedure in a patient with pleural effusion cine, Mount Auburn Hospital, Cambridge, of unknown causation. Analysis of the pleural fluid will allow its categorization as MA (T.W.T., G.S.S.); the Department of Emergency Medicine, Beth Israel Deacon- either a transudate (a product of unbalanced hydrostatic forces) or an exudate (a ess Medical Center, Boston (J.D.); and the product of increased capillary permeability or lymphatic obstruction) (Table 1). If Division of Emergency Medicine, Harvard the effusion seems to have an obvious source (e.g., in an afebrile patient with con- Medical School, Boston (T.W.T., J.D., G.S.S.). Address reprint requests to Dr. Thomsen gestive heart failure and bilateral pleural effusions), diagnostic thoracentesis may at the Department of Emergency Medi- be deferred while the underlying process is treated. The need for the procedure cine, Mount Auburn Hospital, 330 Mount should be reconsidered if there is no appropriate response to therapy.1 Auburn St., Cambridge, MA 02238, or at [email protected]. Thoracentesis, as a therapeutic procedure, may dramatically reduce respiratory distress in patients presenting with large effusions. N Engl J Med 2006;355:e16. Copyright © 2006 Massachusetts Medical Society. CONTRAINDICATIONS There are limited data on the safety of thoracentesis -
Update in Anaesthesia
Update in Anaesthesia Pulmonary Function Tests and Assessment for Lung Resection David Portch*, Bruce McCormick *Correspondence Email: [email protected] INTRODUCTION Summary respectively. There are 2400 lobectomies and 500 The aim of this article is to describe the tests available This article describes the for the assessment of patients presenting for lung pneumonectomies performed in the UK each year, steps taken to evaluate resection. The individual tests are explained and we with in-hospital mortality 2-4% for lobectomy and patients’ fitness for lung 4 describe how patients may progress through a series of 6-8% for pneumonectomy. resection surgery. Examples tests to identify those amenable to lung resection. Lung resection is most frequently performed to treat are used to demonstrate interpretation of these tests. Pulmonary function testing is a vital part of the non-small cell lung cancer. This major surgery places It is vital to use these tests in assessment process for thoracic surgery. However, large metabolic demands on patients, increasing conjunction with a thorough for other types of surgery there is no evidence postoperative oxygen consumption by up to 50%. history and examination that spirometry is more effective than history and Patients presenting for lung resection are often high in order to achieve an examination in predicting postoperative pulmonary risk due to a combination of their age (median age accurate assessment of each complications in patients with known chronic lung is 70 years)5 and co-morbidities. Since non-surgical patient’s level of function. conditions. Furthermore specific spirometric values mortality approaches 100%, a thorough assessment of Much of this assessment (e.g. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Annex 2. List of Procedure Case Rates (Revision 2.0)
ANNEX 2. LIST OF PROCEDURE CASE RATES (REVISION 2.0) FIRST CASE RATE RVS CODE DESCRIPTION Health Care Case Rate Professional Fee Institution Fee Integumentary System Skin, Subcutaneous and Accessory Structures Incision and Drainage Incision and drainage of abscess (e.g., carbuncle, suppurative hidradenitis, 10060 3,640 840 2,800 cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia) 10080 Incision and drainage of pilonidal cyst 3,640 840 2,800 10120 Incision and removal of foreign body, subcutaneous tissues 3,640 840 2,800 10140 Incision and drainage of hematoma, seroma, or fluid collection 3,640 840 2,800 10160 Puncture aspiration of abscess, hematoma, bulla, or cyst 3,640 840 2,800 10180 Incision and drainage, complex, postoperative wound infection 5,560 1,260 4,300 Excision - Debridement 11000 Debridement of extensive eczematous or infected skin 10,540 5,040 5,500 Debridement including removal of foreign material associated w/ open 11010 10,540 5,040 5,500 fracture(s) and/or dislocation(s); skin and subcutaneous tissues Debridement including removal of foreign material associated w/ open 11011 fracture(s) and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, 11,980 5,880 6,100 and muscle Debridement including removal of foreign material associated w/ open 11012 fracture(s) and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, 12,120 6,720 5,400 muscle, and bone 11040 Debridement; skin, partial thickness 3,640 840 2,800 11041 Debridement; skin, full thickness 3,640 840 2,800 11042 Debridement; skin, and -

ANMC Specialty Clinic Services
Cardiology Dermatology Diabetes Endocrinology Ear, Nose and Throat (ENT) Gastroenterology General Medicine General Surgery HIV/Early Intervention Services Infectious Disease Liver Clinic Neurology Neurosurgery/Comprehensive Pain Management Oncology Ophthalmology Orthopedics Orthopedics – Back and Spine Podiatry Pulmonology Rheumatology Urology Cardiology • Cardiology • Adult transthoracic echocardiography • Ambulatory electrocardiology monitor interpretation • Cardioversion, electrical, elective • Central line placement and venous angiography • ECG interpretation, including signal average ECG • Infusion and management of Gp IIb/IIIa agents and thrombolytic agents and antithrombotic agents • Insertion and management of central venous catheters, pulmonary artery catheters, and arterial lines • Insertion and management of automatic implantable cardiac defibrillators • Insertion of permanent pacemaker, including single/dual chamber and biventricular • Interpretation of results of noninvasive testing relevant to arrhythmia diagnoses and treatment • Hemodynamic monitoring with balloon flotation devices • Non-invasive hemodynamic monitoring • Perform history and physical exam • Pericardiocentesis • Placement of temporary transvenous pacemaker • Pacemaker programming/reprogramming and interrogation • Stress echocardiography (exercise and pharmacologic stress) • Tilt table testing • Transcutaneous external pacemaker placement • Transthoracic 2D echocardiography, Doppler, and color flow Dermatology • Chemical face peels • Cryosurgery • Diagnosis -

Core Curriculum for Surgical Technology Sixth Edition
Core Curriculum for Surgical Technology Sixth Edition Core Curriculum 6.indd 1 11/17/10 11:51 PM TABLE OF CONTENTS I. Healthcare sciences A. Anatomy and physiology 7 B. Pharmacology and anesthesia 37 C. Medical terminology 49 D. Microbiology 63 E. Pathophysiology 71 II. Technological sciences A. Electricity 85 B. Information technology 86 C. Robotics 88 III. Patient care concepts A. Biopsychosocial needs of the patient 91 B. Death and dying 92 IV. Surgical technology A. Preoperative 1. Non-sterile a. Attire 97 b. Preoperative physical preparation of the patient 98 c. tneitaP noitacifitnedi 99 d. Transportation 100 e. Review of the chart 101 f. Surgical consent 102 g. refsnarT 104 h. Positioning 105 i. Urinary catheterization 106 j. Skin preparation 108 k. Equipment 110 l. Instrumentation 112 2. Sterile a. Asepsis and sterile technique 113 b. Hand hygiene and surgical scrub 115 c. Gowning and gloving 116 d. Surgical counts 117 e. Draping 118 B. Intraoperative: Sterile 1. Specimen care 119 2. Abdominal incisions 121 3. Hemostasis 122 4. Exposure 123 5. Catheters and drains 124 6. Wound closure 128 7. Surgical dressings 137 8. Wound healing 140 1 c. Light regulation d. Photoreceptors e. Macula lutea f. Fovea centralis g. Optic disc h. Brain pathways C. Ear 1. Anatomy a. External ear (1) Auricle (pinna) (2) Tragus b. Middle ear (1) Ossicles (a) Malleus (b) Incus (c) Stapes (2) Oval window (3) Round window (4) Mastoid sinus (5) Eustachian tube c. Internal ear (1) Labyrinth (2) Cochlea 2. Physiology of hearing a. Sound wave reception b. Bone conduction c.