The Differential Diagnosis of the Breathless Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
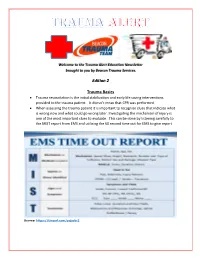
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

Bacterial Tracheitis and the Child with Inspiratory Stridor
Bacterial Tracheitis and the Child With Inspiratory Stridor Thomas Jevon, MD, and Robert L. Blake, Jr, MD Columbia, Missouri Traditionally the presence of inspiratory stridor The child was admitted to the hospital with a and upper respiratory tract disease in a child has presumptive diagnosis of croup and was treated led the primary care physician to consider croup, with mist, hydration, and racemic epinephrine. epiglottitis, and foreign body aspiration in the Initially he improved slightly, but approximately differential diagnosis. The following case demon eight hours after admission he was in marked res strates the importance of considering another piratory distress and had a fever of 39.4° C. At this condition, bacterial tracheitis, in the child with time he had a brief seizure. After this episode his upper airway distress. arterial blood gases on room air were P02 3 8 mmHg and PC02 45 mm Hg, and pH 7.38. Direct laryngos copy was performed, revealing copious purulent Case Report secretions below the chords. This material was A 30-month-old boy with a history of atopic removed by suction, and an endotracheal tube was dermatitis and recurrent otitis media, currently re placed. He was treated with oxygen, frequent suc ceiving trimethoprim-sulfamethoxazole, presented tioning, and intravenous nafcillin and chloramphen to the emergency room late at night with a one-day icol. Culture of the purulent tracheal secretions history of low-grade fever and cough and a three- subsequently grew alpha and gamma streptococci hour history of inspiratory stridor. He was in mod and Hemophilus influenzae resistant to ampicillin. erate to severe respiratory distress with a respira Blood cultures were negative. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Chest Pain and Non-Respiratory Symptoms in Acute Asthma
Postgrad Med J 2000;76:413–414 413 Chest pain and non-respiratory symptoms in Postgrad Med J: first published as 10.1136/pmj.76.897.413 on 1 July 2000. Downloaded from acute asthma W M Edmondstone Abstract textbooks. Occasionally the combination of The frequency and characteristics of chest dyspnoea and chest pain results in diagnostic pain and non-respiratory symptoms were confusion. This study was prompted by the investigated in patients admitted with observation that a number of patients admitted acute asthma. One hundred patients with with asthmatic chest pain had been suspected a mean admission peak flow rate of 38% of having cardiac ischaemia, pleurisy, pericardi- normal or predicted were interviewed tis, or pulmonary embolism. It had also been using a questionnaire. Chest pain oc- observed that many patients admitted with curred in 76% and was characteristically a asthma complained of a range of non- dull ache or sharp, stabbing pain in the respiratory symptoms, something which has sternal/parasternal or subcostal areas, been noted previously in children1 and in adult worsened by coughing, deep inspiration, asthmatics in outpatients.2 The aim of this or movement and improved by sitting study was to examine the frequency and char- upright. It was rated at or greater than acteristics of chest pain and other symptoms in 5/10 in severity by 67% of the patients. A patients admitted with acute asthma. wide variety of upper respiratory and sys- temic symptoms were described both Patients and methods before and during the attack. One hundred patients (66 females, mean (SD) Non-respiratory symptoms occur com- age 45.0 (19.7) years) admitted with acute monly in the prodrome before asthma asthma were studied. -
Guidelines for Prevention of Healthcare Associated Lower
State of Kuwait Ministry of Health Infection Control Directorate Guidelines for Prevention of Healt Care Associated LRTI Aug. 2006 1 I- Introduction Respiratory tract infections are extremely common health-care associated infections. Lower respiratory tract infection incorporates a spectrum of disease from acute bronchitis to pneumonia. Several factors (age, underlying disease, environment) influence mortality, morbidity and also microbial aetiology especially with the most frequently identified antibiotic resistance of respiratory pathogens. Of the lower respiratory tract infections, pneumonia remains the most common infection seen among hospitalized patients. It is defined as a lower respiratory tract infection occurring > 48 hrs of admission to a hospital or nursing home in a patient who was not incubating the infection on admission. It is the second most common health-care associated infection worldwide after urinary tract infection accounting for 13-18% of all health-care associated infections. Health-care associated pneumonia tends to be more serious because defense mechanisms against infection are often impaired , and the kind of infecting organisms are more dangerous than those generally encountered in the community. It is commonly caused by pathogens that need aggressive diagnostic approach with prompt recognition and urgent treatment to reduce morbidity and mortality; often the strains causing health-care associated pneumonia are multiple. It is complicate up to 1% of all hospitalizations. Critically ill patients who require mechanical ventilation are especially vulnerable to develop ventilator associated pneumonia (VAP). Because of its tremendous risk in the last two decades, most of the research on hospital associated pneumonia has been focused on VAP. As treatment, prognosis and outcome of VAP may differ significantly from other forms of hospital acquired pneumonia, it will be discussed extensively. -

Upper and Lower Respiratory Tract Infections Dr
Upper and Lower Respiratory Tract Infections Dr. Shannon MacPhee IWK Emergency Department April 4, 2014 Declaration of Disclosure • I have no actual or potential conflict of interest in relation to this program. • I also assume responsibility for ensuring the scientific validity, objectivity, and completeness of the content of my presentation. Objectives Stridor Community acquired pneumonia Pathogenesis Clinical presentation and medical workup Treatment Complications: Pleural effusion Bronchiolitis Croup • 15% of all pediatric emergency visits in North America • Abrupt onset • Night • 8% admission rate Croup Laryngotracheobronchitis 6 months to 6 years Parainfluenza (75%) Hoarse voice, Inspiratory stridor, Barky cough Croup radiograph Biennial variation in croup Croup scores No matter which system is used, the presence of retractions and stridor at rest are the two most critical clinical features. Croup treatment Humidified air (not mist!) Dexamethasone Dose and population Budesonide not recommended $$$ Inhaled epinephrine Discharge after 1.5‐3 hours of observation in ER if completely stable Mild croup RCT O.6 mg/kg Follow up on Days 1,2,3,7,21 Detailed analysis of costs for the “payer” (ED visit, Physician billing, med cost) Cost for family (parking, lost work, ambulance service, lost productivity) Average societal cost of $92 versus $72 (Dex versus placeb0) Return visits reduced by more than 50% with dexamethasone arm Dex initial effects within 30 minutes Croup Disposition 1.5‐3 hours post epinephrine Disposition should -

Studies on Influenza in the Pandemic of 1957-1958. Ii. Pulmonary Complications of Influenza
STUDIES ON INFLUENZA IN THE PANDEMIC OF 1957-1958. II. PULMONARY COMPLICATIONS OF INFLUENZA Donald B. Louria, … , Edwin D. Kilbourne, David E. Rogers J Clin Invest. 1959;38(1):213-265. https://doi.org/10.1172/JCI103791. Research Article Find the latest version: https://jci.me/103791/pdf STUDIES ON INFLUENZA IN THE PANDEMIC OF 1957-1958. II. PULMONARY COMPLICATIONS OF INFLUENZA * t By DONALD B. LOURIAt HERBERT L. BLUMENFELDt JOHN T. ELLIS, EDWIN D. KILBOURNE, AND DAVID E. ROGERS (From the Departments of Medicine, Pathology, and Public Health and Preventive Medicine, The New York Hospital-Cornell Medical Center, New York, N. Y.) (Submitted for publication July 10, 1958; accepted August 7, 1958) Influenza presents a paradox. To the clinician edge of influenza derived from modern virologic practicing medicine in 1918, influenza was a fear- studies of the epidemic (interpandemic) disease some disease attended by frequent and often fatal must be applied with caution to the 1918-19 pan- pulmonary complications. To the student of in- demic. In the new pandemic in 1957, certain old terpandemic influenza in the last quarter century, questions remained unanswered: the disease is an acute, temporarily incapacitating 1. What is the etiologic agent of pandemic in- infection of the upper respiratory tract which is fluenza? benign except on the rare occasion when bacterial 2. Is the pandemic disease more severe than the pneumonia supervenes. This contrast in the mani- interpandemic form or only more widespread? festations of influenza has led to speculation that 3. Is bacterial pneumonia the major cause of the disease of 1918 was either a different disease fatalities in pandemic influenza; if so, may fatali- entity or caused by an agent of greater virulence ties be prevented by modem antimicrobials? than influenza viruses now encountered. -

TOPIC 2. Airway Patency Impairment. First Aid. Lesson 2 1. Anatomical and Physiological Features of the Respiratory Tract. 2. D
TOPIC 2. Airway patency impairment. First aid. Lesson 2 1. Anatomical and physiological features of the respiratory tract. 2. Definition, causes, types, signs of airway obstruction. 3. Management of airway obstruction. Peculiarities of a foreign body removal from the respiratory tract of a pregnant woman, obese, infants. 4. Technique of ensuring airway patency (head tilt; jaw thrust; insertion of the nasopharyngeal and oropharyngeal airways). 5. Techniques of ventilation (mouth to mouth, mouth to nose, mouth to face mask, Bag-Valve ventilation). 6. Acute respiratory disorders in combat. Pneumothorax: types, signs and symptoms, first aid. Q4. Assessment of the airway patency of the victim. Technique of ensuring airway patency (head tilt; jaw thrust; insertion of the nasopharyngeal and oropharyngeal airways). Assessment of the upper airway of the victim usually requires positioning the individual supine on a flat, firm surface with the arms along the sides of the body. Unless trauma can be definitely excluded, any movement of the victim should consider the possibility of a spine injury. As the patient is placed supine, stabilize the cervical spine by maintaining the head, neck, and trunk in a straight line. If the neck is not already straight, then it should be moved as little as possible to establish the airway. If the patient cannot be placed supine, the jaw thrust maneuver can be applied with the rescuer at the victim’s side. Common causes of airway obstruction in an unconscious patient are occlusion of the oropharynx by the tongue and laxity of the epiglottis. With loss of muscle tone, the tongue or the epiglottis can be forced back into the oropharynx upon inspiration. -

Management of Wheeze and Cough in Infants and Pre-Schoo L Children In
nPersonal opinio lManagement of wheeze and cough in infants and pre-schoo echildren in primary car Pauln Stephenso nIntroductio is, well established in adults 2thoughs there remain somer controversy about its diagnosis in children eve Managementa of wheeze and cough in children is sinceh Spelman's uncontrolled study of children wit commonm problem in primary care. In this paper I ai nchronic cough successfully treated according to a tod provide a few useful management tools with regar .asthma protocol 3gWithout the ability to perform lun toe diagnosis, the role of a trial of treatment, and th functione tests in pre-school children, care must b rationalee for referral. For an in-depth review see th takent to exclude other diagnoses. A persisten article. in this journal two years ago by Bush 1 eproductiv coughc may be due solely to chroni catarrhe with postnasal drip, but early referral may b sPresentation of Symptom needed. A persistent dry cough,n worse at night and o exercise,s and without evidence of other diagnose Ity is always worth asking parents what they mean b warrants. a trial of asthma treatment thed term 'wheeze' or 'cough'. The high-pitche musicaln noise of a wheeze usually on expiratio Thef younger the child, the longer the list o shouldy not be confused with the sound of inspirator differentialo diagnoses and the more one has t sstridor. The sound of airflow through secretions i econsider possibilities other than 'asthma'. Thes ddifferent again, and parents may describe their chil linclude upper airways disease, congenital structura 'vomiting'g when, in fact, the child has been coughin diseasel of the bronchi, bronchial or trachea severely and bringing up phlegm or mucus. -

A Case of Pseudomembranous Tracheitis Caused by Mycoplasma Pneumoniae in an Immunocompetent Patient
205 Case Report Page 1 of 7 A case of pseudomembranous tracheitis caused by Mycoplasma pneumoniae in an immunocompetent patient Yong Hoon Lee, Hyewon Seo, Seung Ick Cha, Chang Ho Kim, Jaehee Lee Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Republic of Korea Correspondence to: Jaehee Lee. Department of Internal Medicine, School of Medicine, Kyungpook National University, 680 Gukchaebosang-ro, Jung-gu, 700-842, Daegu, Republic of Korea. Email: [email protected]. Abstract: Pseudomembranous tracheitis (PMT) is a rare condition characterized by pseudomembrane formation in the tracheobronchial tree that may be associated with infectious and noninfectious processes. However, PMT attributed to Mycoplasma pneumoniae (M. pneumoniae), a common atypical respiratory infectious pathogen, has not been reported till date. Here, we report about a 29-year-old woman with complaints of severe persistent cough and radiographic deterioration despite antibiotics administration for pneumonia at an outside facility. She was finally diagnosed as having PMT with bilateral diffuse bronchiolitis caused by M. pneumoniae infection. The diagnosis was made based on a bronchoscopic finding of a pseudomembrane that partially covered the membranous portion of the upper and middle trachea, a positive polymerase chain reaction (PCR) test with bronchial aspirate, and a positive serological test for M. pneumoniae without detection of any other causative pathogen through an extensive workup. Her symptoms and radiographic findings improved in response to moxifloxacin and corticosteroid treatment. This case is a rare presentation of M. pneumoniae infection complicating PMT in a young adult without any known risk factors. Keywords: Tracheitis; bronchiolitis; Mycoplasma pneumoniae (M. pneumoniae) Submitted Dec 12, 2018.