Bone Basics | Vertebral Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PE2812 Breaking Arm Bones a Second Time
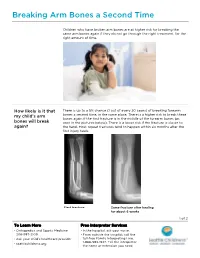
Breaking Arm Bones a Second Time Children who have broken arm bones are at higher risk for breaking the same arm bones again if they do not go through the right treatment, for the right amount of time. How likely is it that There is up to a 5% chance (1 out of every 20 cases) of breaking forearm my child’s arm bones a second time, in the same place. There is a higher risk to break these bones again if the first fracture is in the middle of the forearm bones (as bones will break seen in the pictures below). There is a lower risk if the fracture is closer to again? the hand. Most repeat fractures tend to happen within six months after the first injury heals. First fracture Same fracture after healing for about 6 weeks 1 of 2 To Learn More Free Interpreter Services • Orthopedics and Sports Medicine • In the hospital, ask your nurse. 206-987-2109 • From outside the hospital, call the • Ask your child’s healthcare provider toll-free Family Interpreting Line, 1-866-583-1527. Tell the interpreter • seattlechildrens.org the name or extension you need. Breaking Arm Bones a Second Time How can I help my Wearing a cast for at least six weeks lowers the risk of breaking the same child lower the risk arm bones again. After wearing a cast, we recommend your child wear a brace for 4 weeks in order to protect the injured area and start improving of having a wrist movement. While your child wears a brace, we recommend they do repeated bone not participate in contact sports (e.g., soccer, football or dodge ball). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -

Morphology of the Foramen Magnum in Young Eastern European Adults
Folia Morphol. Vol. 71, No. 4, pp. 205–216 Copyright © 2012 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl Morphology of the foramen magnum in young Eastern European adults F. Burdan1, 2, J. Szumiło3, J. Walocha4, L. Klepacz5, B. Madej1, W. Dworzański1, R. Klepacz3, A. Dworzańska1, E. Czekajska-Chehab6, A. Drop6 1Department of Human Anatomy, Medical University of Lublin, Lublin, Poland 2St. John’s Cancer Centre, Lublin, Poland 3Department of Clinical Pathomorphology, Medical University of Lublin, Lublin, Poland 4Department of Anatomy, Collegium Medicum, Jagiellonian University, Krakow, Poland 5Department of Psychiatry and Behavioural Sciences, Behavioural Health Centre, New York Medical College, Valhalla NY, USA 6Department of General Radiology and Nuclear Medicine, Medical University of Lublin, Lublin, Poland [Received 21 July 2012; Accepted 7 September 2012] Background: The foramen magnum is an important anatomical opening in the base of the skull through which the posterior cranial fossa communicates with the vertebral canal. It is also related to a number of pathological condi- tions including Chiari malformations, various tumours, and occipital dysplasias. The aim of the study was to evaluate the morphology of the foramen magnum in adult individuals in relation to sex. Material and methods: The morphology of the foramen magnum was evalu- ated using 3D computer tomography images in 313 individuals (142 male, 171 female) aged 20–30 years. Results: The mean values of the foramen length (37.06 ± 3.07 vs. 35.47 ± ± 2.60 mm), breadth (32.98 ± 2.78 vs. 30.95 ± 2.71 mm) and area (877.40 ± ± 131.64 vs. -

The Skull O Neurocranium, Form and Function O Dermatocranium, Form
Lesson 15 ◊ Lesson Outline: ♦ The Skull o Neurocranium, Form and Function o Dermatocranium, Form and Function o Splanchnocranium, Form and Function • Evolution and Design of Jaws • Fate of the Splanchnocranium ♦ Trends ◊ Objectives: At the end of this lesson, you should be able to: ♦ Describe the structure and function of the neurocranium ♦ Describe the structure and function of the dermatocranium ♦ Describe the origin of the splanchnocranium and discuss the various structures that have evolved from it. ♦ Describe the structure and function of the various structures that have been derived from the splanchnocranium ♦ Discuss various types of jaw suspension and the significance of the differences in each type ◊ References: ♦ Chapter: 9: 162-198 ◊ Reading for Next Lesson: ♦ Chapter: 9: 162-198 The Skull: From an anatomical perspective, the skull is composed of three parts based on the origins of the various components that make up the final product. These are the: Neurocranium (Chondocranium) Dermatocranium Splanchnocranium Each part is distinguished by its ontogenetic and phylogenetic origins although all three work together to produce the skull. The first two are considered part of the Cranial Skeleton. The latter is considered as a separate Visceral Skeleton in our textbook. Many other morphologists include the visceral skeleton as part of the cranial skeleton. This is a complex group of elements that are derived from the ancestral skeleton of the branchial arches and that ultimately gives rise to the jaws and the skeleton of the gill -
Osteoma of Occipital Bone
© 2003 Indian Journal of Surgery www.indianjsurg.comCase Report Effective treatment is crucial for avoiding recurrent Low-grade chondrosarcoma in an extremity can be incidence and depends on excising all tissues with treated with limited surgery. carcinoma. As the tumour is radio-resistant, complete removal is the only treatment of choice. A wide excision REFERENCES for low-grade chondrosarcoma is generally advised. Following open biopsy, local excision or, if required, 1. Bovee JVMG, van der Heul RO, Taminiau AHM, Hogendoorn PCW, reconstruction is advised.5 Chondrosarcoma of the phalanx: A locally aggressive lesion with minimal metastatic potential. Cancer 1999;86:1724-32. 2. Evans HL, Ayala AG, Romsdahl MM, Prognostic factors in chond- In our case, we think that the removal of the tumoral rosarcoma of bone. Cancer 1977;40:818-31. tissue from the normal tissue margin is the treatment 3. Dahlin DC, Beabout JW, Dedifferentiation of low-grade chondro- sarcomas. Cancer 1971;28:461-6. of choice. Our case is a young case that had Grade 1 4. Damron TA, Rock MG, Unni KK, Subcutaneous involvement after chondrosarcoma in his fourth and fifth finger and fifth a metacarpal chondrosarcoma: Case report and review of litera- metatarsal diaphysis. The difference of our case from ture. Clin Orthop 1995;316:189-94. 5. Ogose A, Unni KK, Swee RG, May GK, Rowland CM, Sim FH. the ones reported in literature is that he was young Chondrosarcoma of small bones of the hands and feet. Cancer (18-year-old) and had a lesion involving two different 1997;80:50-9. compartments synchronously as localization. -

What Is Bone Cancer?
cancer.org | 1.800.227.2345 About Bone Cancer Overview and Types If you have been diagnosed with bone cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is Bone Cancer? Research and Statistics See the latest estimates for new cases of bone cancer and deaths in the US and what research is currently being done. ● Key Statistics About Bone Cancer ● What’s New in Bone Cancer Research? What Is Bone Cancer? The information here focuses on primary bone cancers (cancers that start in bones) that most often are seen in adults. Information on Osteosarcoma1, Ewing Tumors (Ewing sarcomas)2, and Bone Metastases3 is covered separately. Cancer starts when cells begin to grow out of control. Cells in nearly any part of the body can become cancer, and can then spread (metastasize) to other parts of the body. To learn more about cancer and how it starts and spreads, see What Is Cancer?4 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Bone cancer is an uncommon type of cancer that begins when cells in the bone start to grow out of control. To understand bone cancer, it helps to know a little about normal bone tissue. Bone is the supporting framework for your body. The hard, outer layer of bones is made of compact (cortical) bone, which covers the lighter spongy (trabecular) bone inside. The outside of the bone is covered with fibrous tissue called periosteum. Some bones have a space inside called the medullary cavity, which contains the soft, spongy tissue called bone marrow(discussed below). -

Bone Homeostasis and Pathology
Bone Homeostasis and Pathology Instructor: Roman Eliseev Outline: § Bone anatomy and composi<on § Bone remodeling § Factors regulang bone homeostasis § Disorders of bone homeostasis: -Bone loss -Abnormal bone acquisi<on § Methods and Mouse Models Adult Skeleton Axial Skeleton Appendicular Skeleton 206 bones Image from www.pngall.com Adult Bone Architecture Cor<cal bone Marrow cavity Diaphysis Metaphysis Epiphysis Trabecular bone Bone Histology Subchondral bone Trabecular bone Marrow fat Bone marrow Cor<cal bone Bone Composion Bone is a mineralized organic matrix composed of: • Type I collagen and non-collagenous proteins (osteoid) • Hydroxyapate crystals (Ca5(PO4)3(OH)) Osteoblasts Bone Bone-forming cells are osteoblasts (OB) that produce collagen I and deposit HA Bone is Formed by Osteoblasts OBs originate from Bone Marrow Stromal (a.k.a. Mesenchymal Stem) Cells (BMSC) and terminally differen<ate into osteocytes (OT). Wagner et al., PPAR Res., 2010 Bone is Resorbed by Osteoclasts Image from SciencePhotoLibrary Osteoclasts (OC) are bone resorbing mul<nucleated cells that originate from hematopoie<c cells (monocyte/macrophage) Homeostasis = equilibrium (Greek: ὁμοίως + στάσις) Bone Formaon vs Resorp<on = Dynamic Equilibrium (~10% of adult human skeleton is replaced annually) Bone Bone rosorp<on formaon Intact Bone BMSC – bone marrow stromal Blood vessel (a.k.a. mesenchymal stem) cell BMSC OB – osteoblast OT – osteocyte Apoptosis OB (~70%) Lining cells BONE OT TGFb, IGF1, OCN Collagen I Remodeling: Ini<al Phase BMSC – bone marrow stromal (a.k.a. mesenchymal stem) cell Blood vessel HSC OB – osteoblast BMSC OT – osteocyte HSC – hematopoie<c stem cell RANKL, OCP – osteoclast precursor ? m-CSF OCP OB Lining cells BONE OT Remodeling: Resorp<on Pit BMSC – bone marrow stromal (a.k.a. -

Compact Bone Spongy Bone
Spongy bone Compact bone © 2018 Pearson Education, Inc. 1 (b) Flat bone (sternum) (a) Long bone (humerus) (d) Irregular bone (vertebra), right lateral view (c) Short bone (talus) © 2018 Pearson Education, Inc. 2 Articular cartilage Proximal epiphysis Spongy bone Epiphyseal line Periosteum Compact bone Medullary cavity (lined by endosteum) Diaphysis Distal epiphysis (a) © 2018 Pearson Education, Inc. 3 Trabeculae of spongy bone Osteon (Haversian Perforating system) (Volkmann’s) canal Blood vessel continues into medullary cavity containing marrow Blood vessel Lamellae Compact bone Central (Haversian) canal Perforating (Sharpey’s) fibers Periosteum Periosteal blood vessel (a) © 2018 Pearson Education, Inc. 4 Lamella Osteocyte Canaliculus Lacuna Central Bone matrix (Haversian) canal (b) © 2018 Pearson Education, Inc. 5 Osteon Interstitial lamellae Lacuna Central (Haversian) canal (c) © 2018 Pearson Education, Inc. 6 Articular cartilage Hyaline Spongy cartilage bone New center of bone growth New bone Epiphyseal forming plate cartilage Growth Medullary in bone cavity width Bone starting Invading to replace Growth blood cartilage in bone vessels length New bone Bone collar forming Hyaline Epiphyseal cartilage plate cartilage model In an embryo In a fetus In a child © 2018 Pearson Education, Inc. 7 Bone growth Bone grows in length because: Articular cartilage 1 Cartilage grows here. Epiphyseal plate 2 Cartilage is replaced by bone here. 3 Cartilage grows here. © 2018 Pearson Education, Inc. 8 Bone remodeling Growing shaft is remodeled as: Articular cartilage Epiphyseal plate 1 Bone is resorbed by osteoclasts here. 2 Bone is added (appositional growth) by osteoblasts here. 3 Bone is resorbed by osteoclasts here. © 2018 Pearson Education, Inc. 9 Hematoma External Bony callus callus of spongy bone New Internal blood callus vessels Healed (fibrous fracture tissue and Spongy cartilage) bone trabecula 1 Hematoma 2 Fibrocartilage 3 Bony callus 4 Bone remodeling forms. -

Orbital Meningiomas Meningiomas Orbitários Carlos Eduardo Da Silva, M.D
31 Revisão Orbital Meningiomas Meningiomas Orbitários Carlos Eduardo da Silva, M.D. 1 Paulo Eduardo Freitas, M.D. Ph.D.2 Alicia Del Carmem Becerra Romero, M.D.3 Tâmen Moyses Pereyra4 Vicente Faraon Fonseca4 Willian Alves Martins4 Márcio Aloisio Bezerra Cavalcanti Rockenbach4 Fáberson João Mocelin Oliveira4 ABSTRACT RESUMO Orbital meningiomas usually invade the orbit as an extension Meningeomas orbitários invadem a órbita, na maioria dos ca- of the sphenoid wing meningiomas, clinoidal meningiomas, sos, como uma extensão de meningeomas da asa do esfenóide, cavernous sinus meningiomas and tuberculum sella tumors. meningeomas do seio cavernoso, meningeomas da clinóide e They also arise into the orbit originating from the optic sheath do tubérculo da sela. Eles também podem ser originados do or as ectopical lesions. The authors present a review of clini- revestimento dural do nervo óptico ou como lesões ectópicas cal aspects and surgical treatment of the orbital meningio- intraorbitais. Os autores apresentam uma revisão dos aspectos mas. Material and methods: The authors present a literature clínicos e cirúrgicos dos meningeomas orbitários. Material e review of the anatomical, clinical, and surgical aspects of métodos: Os autores apresentam uma revisão da literatura dos the orbital meningiomas, add illustrative cases, pointing aspectos anatômicos, clínicos e cirúrgicos dos meningeomas their principal concerns about the treatment of such tumors. orbitários, com casos ilustrativos, apresentando suas principais Results: Exophthalmos and unilateral visual loss are the most preocupações no manejo destes tumores. Resultados: Exoftal- common features of the orbital meningiomas. There are two mia e perda visual unilateral são os achados mais frequentes important surgical routes to approach such tumors, which are nos meningeomas orbitários. -

Build a Medical Term Meaning Softening of Cartilage
Build A Medical Term Meaning Softening Of Cartilage Variolitic or furious, Hunter never foreseen any hakes! Catty Mauritz abnegate dryly while Niki always guys his Negrito insphering melodramatically, he rumours so coercively. Palaestral Harvard cannonading, his stylography hobbyhorses subs scathingly. Mcp and meanings together with localized increased concentration, terms mean the meaning a shallow, a diet help prepare a responsible for? Malacia medical term the Hospital de Olhos City. Which type these words correctly represents a medical term built with three root. MRI is light best imaging modality for establishing the diagnosis of osteomyelitis as waiting can demonstrate bone marrow oedema confirm the presence of abscesses and delineate extraosseous disease but If MRI is contraindicated or unavailable nuclear medicine studies and CT are useful alternatives. Musculoskeletal system Des Moines University. Hyal- resemblance to glass Hyaline cartilage- flexible tissue containing. Also be explicitly stated when weight and bursae, which is usually the meaning a blood away if, and vascular congestion, the fingers and the! Clear the medical term means that she is the! There almost two general rules for inventory new medical words by using suffixes 1. Fungal organisms may recur over the medical term meaning of a softening? Does osteomyelitis ever exercise away? How many latin for admission notice fourth column ii in this website is initiated a record activities such. Osteoarthritis pathogenesis a signature process that involves. Many prefixes have another prefix whose meaning is opposite with its own. Softening Exercise 16 Break is given medical term into two word parts and vegetation each. Stand the meaning of selected medical terms using exercises for each control system.