MR Imaging of Soft-Tissue Vascular Lesions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Tumors and Tumor-Like Lesions of Blood Vessels 16 F.Ramon
16_DeSchepper_Tumors_and 15.09.2005 13:27 Uhr Seite 263 Chapter Tumors and Tumor-like Lesions of Blood Vessels 16 F.Ramon Contents 42]. There are two major classification schemes for vas- cular tumors. That of Enzinger et al. [12] relies on 16.1 Introduction . 263 pathological criteria and includes clinical and radiolog- 16.2 Definition and Classification . 264 ical features when appropriate. On the other hand, the 16.2.1 Benign Vascular Tumors . 264 classification of Mulliken and Glowacki [42] is based on 16.2.1.1 Classification of Mulliken . 264 endothelial growth characteristics and distinguishes 16.2.1.2 Classification of Enzinger . 264 16.2.1.3 WHO Classification . 265 hemangiomas from vascular malformations. The latter 16.2.2 Vascular Tumors of Borderline classification shows good correlation with the clinical or Intermediate Malignancy . 265 picture and imaging findings. 16.2.3 Malignant Vascular Tumors . 265 Hemangiomas are characterized by a phase of prolif- 16.2.4 Glomus Tumor . 266 eration and a stationary period, followed by involution. 16.2.5 Hemangiopericytoma . 266 Vascular malformations are no real tumors and can be 16.3 Incidence and Clinical Behavior . 266 divided into low- or high-flow lesions [65]. 16.3.1 Benign Vascular Tumors . 266 Cutaneous and subcutaneous lesions are usually 16.3.2 Angiomatous Syndromes . 267 easily diagnosed and present no significant diagnostic 16.3.3 Hemangioendothelioma . 267 problems. On the other hand, hemangiomas or vascular 16.3.4 Angiosarcomas . 268 16.3.5 Glomus Tumor . 268 malformations that arise in deep soft tissue must be dif- 16.3.6 Hemangiopericytoma . -
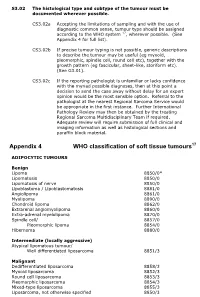
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Solitary Noninfiltrating Angiolipoma on the Finger, an Unusual Localization
Volume 25 Number 2| February 2019| Dermatology Online Journal || Case Presentation 24(2): 8 Solitary noninfiltrating angiolipoma on the finger, an unusual localization. 1 1 1 2 3 Muge Gore Karaali , Asude Kara Polat , Ayse Esra Koku Aksu , Cem Leblebici , Mehmet Salih Gurel Affiliations: Department of Dermatology, Health and Science University Istanbul Training and Research Hospital, Istanbul, Turkey, 2Department of Pathology, Health and Science University Istanbul Training and Research Hospital, Istanbul, Turkey, 3Department of Dermatology, Medeniyet University, Göztepe Training and Research Hospital, Istanbul, Turkey Corresponding Author: Muge Gore Karaali MD, Istanbul Training and Research Hospital, Department of Dermatology, PK: 34098, Istanbul, Turkey, Tel: 90 530 3093328, Fax: 90 212 6320060, Email: [email protected] [2, 3]. A presumptive diagnosis may be via Abstract ultrasonography and/or magnetic resonance Angiolipoma, a subtype of lipoma, is a benign imaging (MRI), [4]. Its definitive diagnosis may be adypocytic soft tissue tumor composed of mature made by clinical examination. Histologically, one adipose tissue and small vascular proliferations. This observes an encapsulated tumor (noninfiltrative) entity makes up 5–17% of all lipomas. The diagnosis and rarely an infiltrative form [5]. The most common is made by clinical and pathological examination, treatment option for this tumor is surgical excision. ultrasonography, and/or magnetic resonance Recurrence has been reported for infiltrating type of imaging (MRI). It is generally an encapsulated tumor (noninfiltrative), but rarely has an infiltrative form. angiolipomas. Noninfiltrating forms generally do not Angiolipoma mostly occurs on the trunk and recur after excision [3]. The forearm is the most extremities with male predominance. The forearm is frequent localization for angiolipomas [1]. -

Benign Hemangiomas
TUMORS OF BLOOD VESSELS CHARLES F. GESCHICKTER, M.D. (From tke Surgical Palkological Laboratory, Department of Surgery, Johns Hopkins Hospital and University) AND LOUISA E. KEASBEY, M.D. (Lancaster Gcaeral Hospital, Lancuster, Pennsylvania) Tumors of the blood vessels are perhaps as common as any form of neoplasm occurring in the human body. The greatest number of these lesions are benign angiomas of the body surfaces, small elevated red areas which remain without symptoms throughout life and are not subjected to treatment. Larger tumors of this type which undergb active growth after birth or which are situated about the face or oral cavity, where they constitute cosmetic defects, are more often the object of surgical removal. The majority of the vascular tumors clinically or pathologically studied fall into this latter group. Benign angiomas of similar pathologic nature occur in all of the internal viscera but are most common in the liver, where they are disclosed usually at autopsy. Angiomas of the bone, muscle, and the central nervous system are of less common occurrence, but, because of the symptoms produced, a higher percentage are available for study. Malignant lesions of the blood vessels are far more rare than was formerly supposed. An occasional angioma may metastasize following trauma or after repeated recurrences, but less than 1per cent of benign angiomas subjected to treatment fall into this group. I Primarily ma- lignant tumors of the vascular system-angiosarcomas-are equally rare. The pathological criteria for these growths have never been ade- quately established, and there is no general agreement as to this par- ticular form of tumor. -

Subcutaneous Cavernous and Capillary Hemangiomas of the Breast: Radiologic-Pathological Correlation1 유방의 피하지방층에 발생한 해면 혈관종과 모세 혈관종:영상 및 병리 소견의 비교1
Case Report pISSN 1738-2637 / eISSN 2288-2928 J Korean Soc Radiol 2013;69(6):475-479 http://dx.doi.org/10.3348/jksr.2013.69.6.475 Subcutaneous Cavernous and Capillary Hemangiomas of the Breast: Radiologic-Pathological Correlation1 유방의 피하지방층에 발생한 해면 혈관종과 모세 혈관종:영상 및 병리 소견의 비교1 Hyoung Nam Lee, MD1, Shin Young Kim, MD1, Hyung Hwan Kim, MD1, Hyun-Deuk Cho, MD2 Departments of 1Radiology, 2Pathology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea Vascular tumors of the breast are uncommon and include hemangioma, angiolipo- ma, and angiosarcoma. Among breast hemangiomas, capillary hemangiomas are Received June 28, 2013; Accepted October 16, 2013 relatively rare in contrast to cavernous hemangiomas. We report two rare cases of Corresponding author: Shin Young Kim, MD Department of Radiology, Soonchunhyang University cavernous and capillary hemangiomas of the breast by mammography, sonography, Cheonan Hospital, 31 Suncheonhyang 6-gil, and positron emission tomography/computed tomography. Dongnam-gu, Cheonan 330-721, Korea. Tel. 82-41-570-3515 Fax. 82-41-579-9026 E-mail: [email protected] Index terms Breast This is an Open Access article distributed under the terms Hemangioma of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) Mammography which permits unrestricted non-commercial use, distri- Sonography bution, and reproduction in any medium, provided the Positron Emission Tomography/CT original work is properly cited. INTRODUCTION CASE REPORT Benign hemangiomas of the breast are rare. The mammo- Case 1 graphic and sonographic appearance of breast hemangiomas An 80-year-old woman had a 6-month history of a palpable have been described in several reports (1-4) but only a few re- mass in the left breast. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Monoclonal Antibody D2-40, a New Marker of Lymphatic Endothelium, Reacts with Kaposi’S Sarcoma and a Subset of Angiosarcomas Harriette J
Monoclonal Antibody D2-40, a New Marker of Lymphatic Endothelium, Reacts with Kaposi’s Sarcoma and a Subset of Angiosarcomas Harriette J. Kahn, M.D., Denis Bailey, M.D., Alexander Marks, M.D. Department of Pathology, Women’s College Campus, Sunnybrook and Women’s College Health Sciences Centre (HJK, AM); Department of Pathology (DB), University Health Network, Banting; and Best Department of Medical Research (AM), University of Toronto, Toronto, Canada omas, in which staining was absent. We conclude that There is controversy over the histogenesis of Kaposi’s D2-40 is a new selective marker of lymphatic endo- sarcoma (KS) from lymphatic or blood vessel endo- thelium in normal tissues and vascular lesions and is thelium. D2-40 is a novel monoclonal antibody to an valuable for studying benign and malignant vascular Mr 40,000 O-linked sialoglycoprotein that reacts with disorders in routinely processed tissue specimens. a fixation-resistant epitope on lymphatic endothe- lium. We sought to establish the selectivity of D2-40 KEY WORDS: Kaposi’s sarcoma, Lymphatic endo- for lymphatic endothelium in normal tissues and thelium, Monoclonal antibody, Vascular lesions. compare its reactivity with the expression of the Mod Pathol 2002;15(4):434–440 widely used vascular endothelial marker CD31 in a series of 62 formalin-fixed and paraffin-embedded Kaposi’s sarcoma (KS) is a vascular proliferative vascular lesions including KS. In normal tissues, disorder with four epidemiological forms: classic, D2-40 stained the endothelium of lymphatic channels African endemic, iatrogenic transplant related, and but not of blood vessels, including arteries and capil- epidemic acute immune deficiency syndrome laries defined by reactivity with the blood vessel endo- (AIDS) related (1). -

Table of Contents
CONTENTS 1. Specimen evaluation 1 Specimen Type. 1 Clinical History. 1 Radiologic Correlation . 1 Special Studies . 1 Immunohistochemistry . 2 Electron Microscopy. 2 Genetics. 3 Recognizing Non-Soft Tissue Tumors. 3 Grading and Prognostication of Sarcomas. 3 Management of Specimen and Reporting. 4 2. Nonmalignant Fibroblastic and Myofibroblastic Tumors and Tumor-Like Lesions . 7 Nodular Fasciitis . 7 Proliferative Fasciitis and Myositis . 12 Ischemic Fasciitis . 18 Fibroma of Tendon Sheath. 21 Nuchal-Type Fibroma . 24 Gardner-Associated Fibroma. 27 Desmoplastic Fibroblastoma. 27 Elastofibroma. 34 Pleomorphic Fibroma of Skin. 39 Intranodal (Palisaded) Myofibroblastoma. 39 Other Fibroma Variants and Fibrous Proliferations . 44 Calcifying Fibrous (Pseudo)Tumor . 47 Juvenile Hyaline Fibromatosis. 52 Fibromatosis Colli. 54 Infantile Digital Fibroma/Fibromatosis. 58 Calcifying Aponeurotic Fibroma. 63 Fibrous Hamartoma of Infancy . 65 Myofibroma/Myofibromatosis . 69 Palmar/Plantar Fibromatosis. 80 Lipofibromatosis. 85 Diffuse Infantile Fibromatosis. 90 Desmoid-Type Fibromatosis . 92 Benign Fibrous Histiocytoma (Dermatofibroma). 98 xi Tumors of the Soft Tissues Non-neural Granular Cell Tumor. 104 Neurothekeoma . 104 Plexiform Fibrohistiocytic Tumor. 110 Superficial Acral Fibromyxoma . 113 Superficial Angiomyxoma (Cutaneous Myxoma). 118 Intramuscular Myxoma. 125 Juxta-articular Myxoma. 128 Aggressive Angiomyxoma . 128 Angiomyofibroblastoma. 135 Cellular Angiofibroma. 136 3. Fibroblastic/Myofibroblastic Neoplasms with Variable Biologic Potential. -

Contents SECTION 1 Fibrohistiocytic Tumors 1 Classification Of
Contents SECTION 1 Fibrohistiocytic Tumors 1 Classification of Fibrohistiocytic Tumors 2 Dermatofibroma 3 Juvenile Xanthogranuloma 4 Solitary Reticulohistiocytoma and Multicentric Reticulohistiocytosis 5 Acrochordons and Pendulous Fibromas 6 Cutaneous Solitary Fibrous Tumor 7 Sclerotic Fibroma (Storiform Collagenoma) 8 Plaque-Like CD34-Positive Dermal Fibroma (Medallion-Like Dermal Dendrocyte Hamartoma) 9 Desmoplastic Fibroblastoma (Collagenous Fibroma) 10 Pleomorphic Fibroma of the Skin 11 Fibroma of Tendon Sheath 12 Giant Cell Tumor of Tendon Sheath 13 Cutaneous Myxoma 14 Superficial Acral Fibromyxoma 15 Cellular Digital Fibroma 16 Nuchal Fibroma and Gardner Syndrome–Associated Fibroma 17 Cerebriform Collagenoma Associated with Proteus Syndrome 18 Elastofibroma 19 Nodular Fasciitis, Proliferative Fasciitis, and Ischemic Fasciitis 20 Fibromatosis 21 Juvenile Hyaline Fibromatosis 22 Fibrous Hamartoma of Infancy 23 Calcifying Aponeurotic Fibroma 24 Dermatofibrosarcoma Protuberans 25 Angiomatoid Fibrous Histiocytoma 26 Plexiform Fibrohistiocytic Tumor 27 Soft Tissue Giant Cell Tumor of Low Malignant Potential 28 Inflammatory Myofibroblastic Tumor 29 Inflammatory Myxohyaline Tumor of Distal Extremities 30 Atypical Fibroxanthoma 31 Malignant Fibrous Histiocytoma 32 Fibrosarcoma 33 Epithelioid Sarcoma 34 Synovial Sarcoma 35 Alveolar Soft Part Sarcoma SECTION 2 Myofibroblastic and Muscle Tumors 36 Myofibroblasts, Muscle Cells, and Classification of Skin Proliferations with Myofibroblastic and Muscle Differentiation 37 Infantile Myofibromatosis -

Infiltrative Angiolipoma of the Neck
INFILTRATIVE ANGIOLIPOMA OF THE NECK ABDUL-LATIF HAMDAN*, LAURICE MAHFOUD**, HANI RIFAI**, CHARBEL RAMEH**, NABIL FULEIHAN* Introduction Lipomas are the most common mesenchymal tumors of the body. They can occur in any soft tissue ranging from subcutaneous fat to the parosteal areas adjacent to bone. They are usually asymptomatic masses easily diagnosed on radiological imaging1. Angiolipoma is a variant of lipoma with proliferation of its vascular component. These tumors occur on the trunk and extremities of young adults with the forearm being the most common site of involvement. Documented sites of occurrence in the head and neck region include cheek, palate, neck, jaw, nose, eyelid, parotid, tongue, paranasal sinuses and parapharynx. Only 4 cases have been described in the neck, with 75% of these being infiltrative2. We would like to present the fifth case of infiltrative angiolipoma of the neck. Case presentation A 23y old male patient, previously healthy, presented with a four month history of a slowly growing, painless neck mass that was not associated with skin changes, fever, recent infection or trauma. No history of contact with patients with tuberculosis. Physical examination revealed a well circumscribed soft left postero-lateral neck mass, 5 × 5 cm, non tender and non pulsatile. Patient had normal muscle power in his upper extremities and normal pulses. A fine needle aspiration revealed an acellular specimen. Magnetic resonance imaging of the head and neck showed a heterogeneous 5 × 4 × 4 cm, well-circumscribed mass with a prominent vascular component, underneath the trapezius and longus colli muscles. The mass enhanced on T1 and T2 weighted images. -

Diagnosis and Management of Infantile Hemangioma David H
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care Diagnosis and Management of Infantile Hemangioma David H. Darrow, MD, DDS, Arin K. Greene, MD, Anthony J. Mancini, MD, Amy J. Nopper, MD, the SECTION ON DERMATOLOGY, SECTION ON OTOLARYNGOLOGY–HEAD AND NECK SURGERY, and SECTION ON PLASTIC SURGERY abstract Infantile hemangiomas (IHs) are the most common tumors of childhood. Unlike other tumors, they have the unique ability to involute after proliferation, often leading primary care providers to assume they will resolve without intervention or consequence. Unfortunately, a subset of IHs rapidly develop complications, resulting in pain, functional impairment, or permanent disfigurement. As a result, the primary clinician has the task of determining which lesions require early consultation with a specialist. Although several recent reviews have been published, this clinical report is the first based on input from individuals representing the many specialties involved in the treatment of IH. Its purpose is to update the pediatric community regarding recent discoveries in IH pathogenesis, treatment, and clinical associations and This document is copyrighted and is property of the American to provide a basis for clinical decision-making in the management of IH. Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication. NOMENCLATURE Clinical reports from the American Academy of Pediatrics benefit from The nomenclature and classification of vascular tumors and expertise and resources of liaisons and internal (American Academy malformations have evolved from clinical descriptions (“strawberry of Pediatrics) and external reviewers.