Tumors and Tumor-Like Lesions of Blood Vessels 16 F.Ramon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man
CASE REPORT Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man LT Sarah Broski Gendernalik, DO, MC (FS), USN LT James D. Gendernalik, DO, MC (FS), USN A 26-year-old previously healthy man presented with a 6-mm violaceous papule that had a surrounding 1.5-cm annular, nonblanching, erythematous halo on the right-sided flank. The man reported the lesion had been recurring for 4 to 5 years, flaring every 4 to 5 months and then slowly disap - pearing until the cycle recurred. Targetoid hemosiderotic hemangioma was clinically diagnosed. The lesion was removed by means of elliptical excision and the condition resolved. The authors discuss the clinical appearance, his - tology, and etiology of targetoid hemosiderotic heman - giomas. J Am Osteopath Assoc . 2011;111(2);117-118 argetoid hemosiderotic hemangiomas (THHs) are a com - Tmonly misdiagnosed presentation encountered in the primary care setting. In the present case report, we aim to pro - Figure. A 6-mm violaceous papule with a surrounding 1.5-cm annular, nonblanching, erythematous halo in a 26-year-old man. vide general practitioners with an understanding of the clin - ical appearance, pathology, and prognosis of THH. Report of Case A 26-year-old previously healthy man presented to our primary around it and itched and burned each time it developed. The care clinic with a 6-mm violaceous papule with a surrounding lesion faded completely to normal-appearing skin between 1.5-cm annular, nonblanching, erythematous halo on the right- episodes, without evidence of a papule or postinflammatory sided flank ( Figure ). The patient stated that the lesion had hyperpigmentation. -

Hemangiosarcoma Philip J
Ettinger & Feldman – Textbook of Veterinary Internal Medicine Client Information Sheet Hemangiosarcoma Philip J. Bergman What is hemangiosarcoma? Hemangiosarcoma (HSA; angiosarcoma or malignant hemangioendothelioma) is an extremely aggressive tumor of blood vessel origin. Because blood vessels are present throughout the body, virtually any site in the body can have HSA. HSA occurs most frequently in dogs (approximately 2% of all tumors) and the most common site is the spleen. However, additional common sites include the heart, liver, muscle, lung skin, bones, kidney, brain, abdomen, and oral cavity. In three large canine splenic disease studies encompassing approximately 2000 dogs, a “rule of two thirds” was found suggesting that approximately two thirds of dogs with a splenic mass have a cancer (therefore one third are not malignant) and two thirds of the malignant tumors of the spleen are HSA. HSA is a disease generally of older dogs and cats with an average onset of 9 to 10 years; however, there are reports of extremely young dogs and cats with this disease (5 to 6 months to a few years of age). German shepherd dogs are most commonly diagnosed with HSA; however, other large breed dogs such as golden retrievers and Labrador retrievers may also be overrepresented. In cats, the most common breed is the domestic shorthair. The cause of HSA in dogs and cats is presently unknown. Exposures to toxins such as chemicals, insecticides, and radiation have been reported in humans to be associated with HSA. Ultraviolet light exposure from the sun may be a potential cause of HSA in dogs, as HSAs of the skin are commonly seen in dogs with light hair and poor pigmentation (e.g., Salukis, Whippets, and white Bulldogs). -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Dermatology DDX Deck, 2Nd Edition 65
63. Herpes simplex (cold sores, fever blisters) PREMALIGNANT AND MALIGNANT NON- 64. Varicella (chicken pox) MELANOMA SKIN TUMORS Dermatology DDX Deck, 2nd Edition 65. Herpes zoster (shingles) 126. Basal cell carcinoma 66. Hand, foot, and mouth disease 127. Actinic keratosis TOPICAL THERAPY 128. Squamous cell carcinoma 1. Basic principles of treatment FUNGAL INFECTIONS 129. Bowen disease 2. Topical corticosteroids 67. Candidiasis (moniliasis) 130. Leukoplakia 68. Candidal balanitis 131. Cutaneous T-cell lymphoma ECZEMA 69. Candidiasis (diaper dermatitis) 132. Paget disease of the breast 3. Acute eczematous inflammation 70. Candidiasis of large skin folds (candidal 133. Extramammary Paget disease 4. Rhus dermatitis (poison ivy, poison oak, intertrigo) 134. Cutaneous metastasis poison sumac) 71. Tinea versicolor 5. Subacute eczematous inflammation 72. Tinea of the nails NEVI AND MALIGNANT MELANOMA 6. Chronic eczematous inflammation 73. Angular cheilitis 135. Nevi, melanocytic nevi, moles 7. Lichen simplex chronicus 74. Cutaneous fungal infections (tinea) 136. Atypical mole syndrome (dysplastic nevus 8. Hand eczema 75. Tinea of the foot syndrome) 9. Asteatotic eczema 76. Tinea of the groin 137. Malignant melanoma, lentigo maligna 10. Chapped, fissured feet 77. Tinea of the body 138. Melanoma mimics 11. Allergic contact dermatitis 78. Tinea of the hand 139. Congenital melanocytic nevi 12. Irritant contact dermatitis 79. Tinea incognito 13. Fingertip eczema 80. Tinea of the scalp VASCULAR TUMORS AND MALFORMATIONS 14. Keratolysis exfoliativa 81. Tinea of the beard 140. Hemangiomas of infancy 15. Nummular eczema 141. Vascular malformations 16. Pompholyx EXANTHEMS AND DRUG REACTIONS 142. Cherry angioma 17. Prurigo nodularis 82. Non-specific viral rash 143. Angiokeratoma 18. Stasis dermatitis 83. -

Cutaneous Angiosarcoma: Report of Three Different and Typical Cases Admitted in a Unique Dermatology Clinic*
CASE REPORT 235 s Cutaneous angiosarcoma: report of three different and typical cases admitted in a unique dermatology clinic* Aline Neves Freitas Cabral1 Rafael Henrique Rocha1 Ana Cristina Vervloet do Amaral1 Karina Bittencourt Medeiros2 Paulo Sérgio Emerich Nogueira1 Lucia Martins Diniz3 DOI: http://dx.doi.org/10.1590/abd1806-4841.20175326 Abstract: Angiosarcoma is a rare and aggressive tumor with high rates of metastasis and relapse. It shows a particular predi- lection for the skin and superficial soft tissues. We report three distinct and typical cases of angiosarcoma that were diagnosed in a single dermatology clinic over the course of less than a year: i) Angiosarcoma in lower limb affected by chronic lymph- edema, featuring Stewart-Treves syndrome; ii) a case of the most common type of angiosarcoma loated in the scalp and face of elderly man and; iii) a skin Angiosarcoma in previously irradiated breast. All lesions presented characteristic histopathological findings: irregular vascular proliferation that dissects the collagen bundles with atypical endothelial nuclei projection toward the lumen. Keywords: Hemangiosarcoma; Lymphangiosarcoma; Lymphedema; Non-Filarial Lymphedema; Sarcoma INTRODUCTION Angiosarcoma (AS) is a rare and aggressive neoplasm, that fibers, formed by endothelium with atypical nuclei, prominent to- originates from endothelial cells of lymphatic and blood vessels. It ac- ward the lumen; The tumoral lesion exhibited cohesive epithelioid counts for 5% of malignant skin tumors and less than 1% of all sarco- masses of atypical, large, rounded cells with acidophilic cytoplasm mas. It is notable for having a predilection for the skin and superficial and frequent mitotic figures. (Figure 2). Immunohistochemical anal- soft tissues. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -
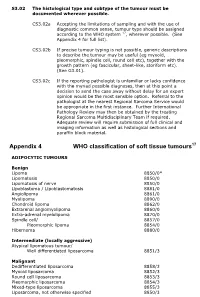
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Lymphangioma Circumscriptum of the Vulva- a Case Series Dermatology Section
DOI: 10.7860/JCDR/2021/47435.14553 Case Series Lymphangioma Circumscriptum of the Vulva- A Case Series Dermatology Section RASHMI S MAHAJAN1, YOGESH S MARFATIA2, ATMAKALYANI R SHAH3, KISHAN R NINAMA4 ABSTRACT Vulval dermatoses pose a diagnostic and therapeutic challenge for the dermatologists. Lymphangioma Circumscriptum (LC) is a form of lymphangioma affecting the skin and subcutaneous tissues that is characterised by benign dilation of lymphatic channels. This uncommon condition is known to occur over the chest, mouth, axilla, tongue, and rarely in the vulva. In this series, authors present three cases of LC of vulva in women between the age group of 45 to 60 years with late-onset fluid-filled lesions over the vulva. The first case had history of hysterectomy prior to onset of lesions, the second case had a spontaneous onset of lesions while the third was a suspected case of pelvic tuberculosis with secondary lymphangioma. Keywords: Lymphangiectasia, Vulvar, Vulval epithelium INTRODUCTION Disorders of vulval epithelium are a confusing spectrum of disorders. They are broadly classified as-1) Inflammatory, 2) Ulcerative and Bullous, 3) Infections, 4) Benign tumours and 5) Malignancies. It is essential to know the exact aetiology to plan successful therapy. LC is a benign lymphatic malformation characterised by dilation of lymphatic vessels in the skin and subcutaneous tissue with lesions erupting locally as isolated or grouped translucid, thin-walled vesicles filled with a clear liquid [1]. These pathological lymphatic malformations have no communication with the normal lymphatics [2]. The precise cause of LC is not established. It could be congenital or acquired as a result of damage to the lymphatic vessels secondary to various aetiologies. -

Solitary Noninfiltrating Angiolipoma on the Finger, an Unusual Localization
Volume 25 Number 2| February 2019| Dermatology Online Journal || Case Presentation 24(2): 8 Solitary noninfiltrating angiolipoma on the finger, an unusual localization. 1 1 1 2 3 Muge Gore Karaali , Asude Kara Polat , Ayse Esra Koku Aksu , Cem Leblebici , Mehmet Salih Gurel Affiliations: Department of Dermatology, Health and Science University Istanbul Training and Research Hospital, Istanbul, Turkey, 2Department of Pathology, Health and Science University Istanbul Training and Research Hospital, Istanbul, Turkey, 3Department of Dermatology, Medeniyet University, Göztepe Training and Research Hospital, Istanbul, Turkey Corresponding Author: Muge Gore Karaali MD, Istanbul Training and Research Hospital, Department of Dermatology, PK: 34098, Istanbul, Turkey, Tel: 90 530 3093328, Fax: 90 212 6320060, Email: [email protected] [2, 3]. A presumptive diagnosis may be via Abstract ultrasonography and/or magnetic resonance Angiolipoma, a subtype of lipoma, is a benign imaging (MRI), [4]. Its definitive diagnosis may be adypocytic soft tissue tumor composed of mature made by clinical examination. Histologically, one adipose tissue and small vascular proliferations. This observes an encapsulated tumor (noninfiltrative) entity makes up 5–17% of all lipomas. The diagnosis and rarely an infiltrative form [5]. The most common is made by clinical and pathological examination, treatment option for this tumor is surgical excision. ultrasonography, and/or magnetic resonance Recurrence has been reported for infiltrating type of imaging (MRI). It is generally an encapsulated tumor (noninfiltrative), but rarely has an infiltrative form. angiolipomas. Noninfiltrating forms generally do not Angiolipoma mostly occurs on the trunk and recur after excision [3]. The forearm is the most extremities with male predominance. The forearm is frequent localization for angiolipomas [1]. -

Toxicological Profile for Glyphosate Were
A f Toxicological Profile for Glyphosate August 2020 GLYPHOSATE II DISCLAIMER Use of trade names is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry, the Public Health Service, or the U.S. Department of Health and Human Services. GLYPHOSATE III FOREWORD This toxicological profile is prepared in accordance with guidelines developed by the Agency for Toxic Substances and Disease Registry (ATSDR) and the Environmental Protection Agency (EPA). The original guidelines were published in the Federal Register on April 17, 1987. Each profile will be revised and republished as necessary. The ATSDR toxicological profile succinctly characterizes the toxicologic and adverse health effects information for these toxic substances described therein. Each peer-reviewed profile identifies and reviews the key literature that describes a substance's toxicologic properties. Other pertinent literature is also presented, but is described in less detail than the key studies. The profile is not intended to be an exhaustive document; however, more comprehensive sources of specialty information are referenced. The focus of the profiles is on health and toxicologic information; therefore, each toxicological profile begins with a relevance to public health discussion which would allow a public health professional to make a real-time determination of whether the presence of a particular substance in the environment poses a potential threat to human health. The adequacy of information to determine a substance's -

Cavernous Hemangioma of the Gallbladder: a Case Report
pISSN 2384-1095 iMRI 2019;23:264-269 https://doi.org/10.13104/imri.2019.23.3.264 eISSN 2384-1109 Cavernous Hemangioma of the Gallbladder: a Case Report Jae Hwi Park1, Jeong Sub Lee1, Guk Myung Choi1, Bong Soo Kim1, Seung Hyoung Kim1, JeongJae Kim1, Doo Ri Kim1, Chang Lim Hyun2, Kyu Hee Her3 1Department of Radiology, Jeju National University Hospital, Jeju National University School of Magnetic resonance imaging Medicine, Jeju, Korea 2Department of Pathology, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea 3Department of Surgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea Case Report Cavernous hemangioma of the gallbladder is an extremely rare benign tumor. The tumor has only a few cases being reported in literature. However, to the best of our knowledge, no reports focusing on the MRI findings of cavernous hemangioma of the Received: April 23, 2019 gallbladder have been published. This study reports a case of gallbladder hemangioma Revised: June 10, 2019 with pathologic and radiologic reviews, including MRI findings. Accepted: July 2, 2019 Correspondence to: Keywords: Cavernous hemangioma; Gallbladder; Magnetic resonance imaging Jeong Sub Lee, M.D. Department of Radiology, Jeju National University Hospital, Jeju National University School of Medicine, 15 Aran 13-gil, INTRODUCTION Jeju-si, Jeju-do 63241, Korea. Tel. +82-64-717-1371 Cavernous hemangioma of the gallbladder is an extremely rare benign tumor (1). Fax. +82-64-717-1370 Hemangioma occurs in several organs, including the liver, brain, lungs and skeletal E-mail: [email protected] muscle. It is the most common benign tumor in the liver, in which cavernous hemangioma represents the majority of tumors (2, 3). -

Glomus Tumor in the Floor of the Mouth: a Case Report and Review of the Literature Haixiao Zou1,2, Li Song1, Mengqi Jia2,3, Li Wang4 and Yanfang Sun2,3*
Zou et al. World Journal of Surgical Oncology (2018) 16:201 https://doi.org/10.1186/s12957-018-1503-6 CASEREPORT Open Access Glomus tumor in the floor of the mouth: a case report and review of the literature Haixiao Zou1,2, Li Song1, Mengqi Jia2,3, Li Wang4 and Yanfang Sun2,3* Abstract Background: Glomus tumors are rare benign neoplasms that usually occur in the upper and lower extremities. Oral cavity involvement is exceptionally rare, with only a few cases reported to date. Case presentation: A 24-year-old woman with complaints of swelling in the left floor of her mouth for 6 months was referred to our institution. Her swallowing function was slightly affected; however, she did not have pain or tongue paralysis. Enhanced computed tomography revealed a 2.8 × 1.8 × 2.1 cm-sized well-defined, solid, heterogeneous nodule above the mylohyoid muscle. The mandible appeared to be uninvolved. The patient underwent surgery via an intraoral approach; histopathological examination revealed a glomus tumor. The patient has had no evidence of recurrence over 4 years of follow-up. Conclusions: Glomus tumors should be considered when patients present with painless nodules in the floor of the mouth. Keywords: Glomus tumor, Floor of mouth, Oral surgery Background Case presentation Theglomusbodyisaspecialarteriovenousanasto- A 24-year-old woman with a 6-month history of swelling mosisandfunctionsinthermalregulation.Glomustu- in the left floor of her mouth was referred to our institu- mors are rare, benign, mesenchymal tumors that tion. Although she experienced slight difficulty in swal- originate from modified smooth muscle cells of the lowing, she did not experience pain or tongue paralysis.