Diagnosis and Management of Infantile Hemangioma David H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Inflated Foley Catheters to Prevent Early Empty Pelvis Complications Following Pelvic Exenteration
ANTICANCER RESEARCH 35: 5543-5546 (2015) Use of Inflated Foley Catheters to Prevent Early Empty Pelvis Complications Following Pelvic Exenteration NICOLAE BACALBASA1, DANA TOMESCU2 and IRINA BALESCU3 1Carol Davila University of Medicine and Pharmacy, Bucharest, Romania; 2Fundeni Clinical Institute, Department of Anaethesia and Critical Care III, Bucharest, Romania; 3Ponderas Hospital, Bucharest, Romania Abstract. For most patients with bulky pelvic tumors, neoadjuvant chemo-irradiation is performed in order to pelvic exenteration remains the only curative option. diminish the local invasion and to transform the patient into Although initially reported as a palliative procedure, a candidate for a less extended resection. However, there nowadays it is rather performed with curative intent. Once are cases in which local invasion persists after neoadjuvant the resectional phase is ended, a large defect will remain at treatment and in which pelvic exenteration is needed. Since the level of the pelvic diaphragm, predisposing to severe Brunschwig reported it for the first time in 1948, this complications which are generically included under the surgical procedure has become the golden-standard for name of empty pelvis syndrome. It has been widely patients with locally invasive pelvic malignancies (3). demonstrated that this type of complication is associated Although the resectional phase has remained practically with severe mortality, even if the patient is free of any pelvic unchanged, the reconstructive phase has undergone multiple recurrence. We present the case of a 56-year-old patient improvements in order to improve the patient quality of submitted to total pelvic exenteration for locally invasive life. However, there are still cases in which a reconstruction previously chemo-irradiated cervical cancer who presented is not possible at the time of resection; in all such cases, a six months after surgery with a severe enteroperineal fistula. -

Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man
CASE REPORT Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man LT Sarah Broski Gendernalik, DO, MC (FS), USN LT James D. Gendernalik, DO, MC (FS), USN A 26-year-old previously healthy man presented with a 6-mm violaceous papule that had a surrounding 1.5-cm annular, nonblanching, erythematous halo on the right-sided flank. The man reported the lesion had been recurring for 4 to 5 years, flaring every 4 to 5 months and then slowly disap - pearing until the cycle recurred. Targetoid hemosiderotic hemangioma was clinically diagnosed. The lesion was removed by means of elliptical excision and the condition resolved. The authors discuss the clinical appearance, his - tology, and etiology of targetoid hemosiderotic heman - giomas. J Am Osteopath Assoc . 2011;111(2);117-118 argetoid hemosiderotic hemangiomas (THHs) are a com - Tmonly misdiagnosed presentation encountered in the primary care setting. In the present case report, we aim to pro - Figure. A 6-mm violaceous papule with a surrounding 1.5-cm annular, nonblanching, erythematous halo in a 26-year-old man. vide general practitioners with an understanding of the clin - ical appearance, pathology, and prognosis of THH. Report of Case A 26-year-old previously healthy man presented to our primary around it and itched and burned each time it developed. The care clinic with a 6-mm violaceous papule with a surrounding lesion faded completely to normal-appearing skin between 1.5-cm annular, nonblanching, erythematous halo on the right- episodes, without evidence of a papule or postinflammatory sided flank ( Figure ). The patient stated that the lesion had hyperpigmentation. -

Hemangiosarcoma Philip J
Ettinger & Feldman – Textbook of Veterinary Internal Medicine Client Information Sheet Hemangiosarcoma Philip J. Bergman What is hemangiosarcoma? Hemangiosarcoma (HSA; angiosarcoma or malignant hemangioendothelioma) is an extremely aggressive tumor of blood vessel origin. Because blood vessels are present throughout the body, virtually any site in the body can have HSA. HSA occurs most frequently in dogs (approximately 2% of all tumors) and the most common site is the spleen. However, additional common sites include the heart, liver, muscle, lung skin, bones, kidney, brain, abdomen, and oral cavity. In three large canine splenic disease studies encompassing approximately 2000 dogs, a “rule of two thirds” was found suggesting that approximately two thirds of dogs with a splenic mass have a cancer (therefore one third are not malignant) and two thirds of the malignant tumors of the spleen are HSA. HSA is a disease generally of older dogs and cats with an average onset of 9 to 10 years; however, there are reports of extremely young dogs and cats with this disease (5 to 6 months to a few years of age). German shepherd dogs are most commonly diagnosed with HSA; however, other large breed dogs such as golden retrievers and Labrador retrievers may also be overrepresented. In cats, the most common breed is the domestic shorthair. The cause of HSA in dogs and cats is presently unknown. Exposures to toxins such as chemicals, insecticides, and radiation have been reported in humans to be associated with HSA. Ultraviolet light exposure from the sun may be a potential cause of HSA in dogs, as HSAs of the skin are commonly seen in dogs with light hair and poor pigmentation (e.g., Salukis, Whippets, and white Bulldogs). -

Detail Report
Supplemental Update Report CR Number: 2012319113 Implementation Date: 16-Jan-19 Related CR: 2012319113 MedDRA Change Requested Add a new SMQ Final Disposition Final Placement Code # Proposed SMQ Infusion related reactions Rejected After Suspension MSSO The proposal to add a new SMQ Infusion related reactions is not approved after suspension. The ICH Advisory Panel did approve this SMQ topic to go into the development phase and it Comment: underwent testing in three databases (two regulatory authorities and one company). However, there were numerous challenges encountered in testing and the consensus decision of the CIOMS SMQ Implementation Working Group was that the topic could not be developed to go into production as an SMQ. Most notably, in contrast to other SMQs, this query could not be tested using negative control compounds because it was not possible to identify suitable compounds administered via infusion that were not associated with some type of reaction. In addition, there is no internationally agreed definition of an infusion related reaction and the range of potential reactions associated with the large variety of compounds given by infusion is very broad and heterogenous. Testing was conducted on a set of around 500 terms, the majority of which was already included in Anaphylactic reaction (SMQ), Angioedema (SMQ), and Hypersensitivity (SMQ). It proved difficult to identify potential cases of infusion related reactions in post-marketing databases where the temporal relationship of the event to the infusion is typically not available. In clinical trial databases where this information is more easily available, users are encouraged to provide more specificity about the event, e.g., by reporting “Anaphylactic reaction” when it is known that this event is temporally associated with the infusion. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Tumors and Tumor-Like Lesions of Blood Vessels 16 F.Ramon
16_DeSchepper_Tumors_and 15.09.2005 13:27 Uhr Seite 263 Chapter Tumors and Tumor-like Lesions of Blood Vessels 16 F.Ramon Contents 42]. There are two major classification schemes for vas- cular tumors. That of Enzinger et al. [12] relies on 16.1 Introduction . 263 pathological criteria and includes clinical and radiolog- 16.2 Definition and Classification . 264 ical features when appropriate. On the other hand, the 16.2.1 Benign Vascular Tumors . 264 classification of Mulliken and Glowacki [42] is based on 16.2.1.1 Classification of Mulliken . 264 endothelial growth characteristics and distinguishes 16.2.1.2 Classification of Enzinger . 264 16.2.1.3 WHO Classification . 265 hemangiomas from vascular malformations. The latter 16.2.2 Vascular Tumors of Borderline classification shows good correlation with the clinical or Intermediate Malignancy . 265 picture and imaging findings. 16.2.3 Malignant Vascular Tumors . 265 Hemangiomas are characterized by a phase of prolif- 16.2.4 Glomus Tumor . 266 eration and a stationary period, followed by involution. 16.2.5 Hemangiopericytoma . 266 Vascular malformations are no real tumors and can be 16.3 Incidence and Clinical Behavior . 266 divided into low- or high-flow lesions [65]. 16.3.1 Benign Vascular Tumors . 266 Cutaneous and subcutaneous lesions are usually 16.3.2 Angiomatous Syndromes . 267 easily diagnosed and present no significant diagnostic 16.3.3 Hemangioendothelioma . 267 problems. On the other hand, hemangiomas or vascular 16.3.4 Angiosarcomas . 268 16.3.5 Glomus Tumor . 268 malformations that arise in deep soft tissue must be dif- 16.3.6 Hemangiopericytoma . -
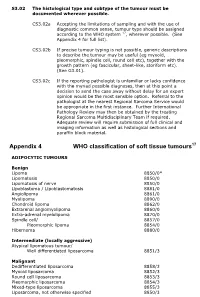
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

CPSC 2011 Annual Report to the President and Congress
2011 2011 ANNUAL REPORT TO THE PRESIDENT AND CONGRESS United States Consumer Product Safety Commission United States Consumer Product Safety Commission Chairman Inez Tenenbaum Vice Chairman Commissioner Robert Adler Nancy Nord Commissioner Anne Northup Report to the President and Congress Pursuant to Section 209 of the Consumer Product Safety Improvement Act of 2008 The United States Consumer Product Safety Commission (CPSC) is submitting this report to the President, Congress, and the public, as required under section 27(j) (15 U.S.C. 2076(j)) of the Consumer Product Safety Act (CPSA), as amended by the Consumer Product Safety Improvement Act of 2008 (CPSIA). The content of this report is specified in the CPSA and the CPSIA. The report describes many of the activities performed to protect the public from hazardous consumer products. Readers may also be interested in the CPSC’s 2011 Performance and Accountability Report, required by the Government Performance and Results Act. All reports are available on the CPSC’s website at: www.cpsc.gov. The CPSC (or the Commission), established by Congress in 1972, is the federal regulatory body tasked with protecting children and families from unreasonable risks of injuries associated with consumer products. In 2010, the Commission launched a comprehensive strategic planning initiative to update its existing strategic plan and help align agency priorities to meet the challenges of the twenty-first century. For example, globalization and technological advances have increased the range of products on the market, as well as the challenges involved in overseeing and regulating thousands of product types that can be assembled across multiple countries. -

Kaposiform Hemangioendothelioma with Kasabach-Merritt Syndrome Mistaken for Child Abuse in a Newborn
Kaposiform Hemangioendothelioma With Kasabach-Merritt Syndrome Mistaken for Child Abuse in a Newborn Amanda A. Cyrulnik, MD; Manju C. Dawkins, MD; Gert J. Smalberger, MD; Scott Young, MD; Ranon E. Mann, MD; Mark I. Jacobson, MD; Adam J. Friedman, MD Practice Points Vascular tumors in dermatology may mimic child abuse. Even when all signs favor abuse, a nonresolving lesion should alarm clinicians to consider an alter- nate diagnosis. Kasabach-Merritt syndrome is a serious and potentially life-threatening condition that requires prompt evaluation. Kaposiform hemangioendotheliomaCUTIS is a rare vas- elevated D-dimer levels, confirming a diagnosis of cular neoplasm of childhood that may have an Kasabach-Merritt syndrome (KMS). alarming and potentially misleading clinical pre- Cutis. 2014;93:E17-E20. sentation. Awareness of this entity is important to provide appropriate and immediate medical care. Case Report We report the case of a 24-day-old female new- A 24-day-old female newborn presented to a hospi- born who presented with a large bruiselike lesion tal with a large bruiselike lesion on the left leg. A on theDo left leg. A diagnosis ofNot cellulitis suspected diagnosis Copy of cellulitis suspected to be secondary to to be secondary to child abuse was made and the child abuse was made and the patient subsequently patient subsequently was placed in foster care; was placed in foster care; however, the lesion did not however, the lesion did not resolve after treatment resolve after treatment and relocation. At 69 days of and relocation. On reevaluation at our institution, age, the patient was readmitted, now to our hospi- physical examination revealed a round, 34-cm, tal, after the lesion persisted and had progressively violaceous, indurated, fixed, nonblanching, non- expanded. -

Infantile Hemangiomas
Infantile Hemangiomas Denise Metry, M.D. Q1. Hemangioma development is most closely associated with: A. Trauma during delivery B. In-utero hypoxia C. Geography D. Maternal smoking E. Maternal ingestion of strawberries Q1. Hemangioma development is most closely associated with: A. Trauma during delivery B. In-utero hypoxia C. Geography D. Maternal smoking E. Maternal ingestion of strawberries Q2. On average, the majority of hemangioma involution is complete by what age? A. 2 years B. 4 years C. 7 years D. 10 years E. They never involute Q2. On average, the majority of hemangioma involution is complete by what age? A. 2 years B. 4 years C. 7 years D. 10 years E. Never Hemangioma Growth/Involution • 80% of growth occurs in first 3-4 months • 80% of involution occurs by kindergarten Question 3 Q3. The best treatment option for this infant is… A. Nothing B. Topical timolol C. Oral propranolol D. Laser E. Surgery Q3. The best treatment option for this infant is… A. Nothing B. Topical timolol C. Oral propranolol D. Laser E. Surgery Timolol 0.5% gel-forming solution Best candidate: Superficial, relatively flat hemangioma Cosmetically sensitive location Infant < 3 months of age Apply 1 drop BID-TID up to 12 months of age Risk of toxicity appears low Monitoring not generally required Oral Propranolol • Non-selective beta-blocker • MOA? • Baseline maternal and infant history, heart rate • 20 mg/5 ml solution. Start at 0.5 mg/kg/day ÷ tid or bid and increase by 25% every 4 days to 2 mg/kg/day • Generally well-tolerated but hypoglycemia real risk • Continued until 12 to 18 months of age Question 4 Q4. -

Cavernous Hemangioma of the Gallbladder: a Case Report
pISSN 2384-1095 iMRI 2019;23:264-269 https://doi.org/10.13104/imri.2019.23.3.264 eISSN 2384-1109 Cavernous Hemangioma of the Gallbladder: a Case Report Jae Hwi Park1, Jeong Sub Lee1, Guk Myung Choi1, Bong Soo Kim1, Seung Hyoung Kim1, JeongJae Kim1, Doo Ri Kim1, Chang Lim Hyun2, Kyu Hee Her3 1Department of Radiology, Jeju National University Hospital, Jeju National University School of Magnetic resonance imaging Medicine, Jeju, Korea 2Department of Pathology, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea 3Department of Surgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea Case Report Cavernous hemangioma of the gallbladder is an extremely rare benign tumor. The tumor has only a few cases being reported in literature. However, to the best of our knowledge, no reports focusing on the MRI findings of cavernous hemangioma of the Received: April 23, 2019 gallbladder have been published. This study reports a case of gallbladder hemangioma Revised: June 10, 2019 with pathologic and radiologic reviews, including MRI findings. Accepted: July 2, 2019 Correspondence to: Keywords: Cavernous hemangioma; Gallbladder; Magnetic resonance imaging Jeong Sub Lee, M.D. Department of Radiology, Jeju National University Hospital, Jeju National University School of Medicine, 15 Aran 13-gil, INTRODUCTION Jeju-si, Jeju-do 63241, Korea. Tel. +82-64-717-1371 Cavernous hemangioma of the gallbladder is an extremely rare benign tumor (1). Fax. +82-64-717-1370 Hemangioma occurs in several organs, including the liver, brain, lungs and skeletal E-mail: [email protected] muscle. It is the most common benign tumor in the liver, in which cavernous hemangioma represents the majority of tumors (2, 3). -

Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital
ﺑﺴﻢ اﷲ اﻟﺮﺣﻤﻦ اﻟﺮﺣﻴﻢ Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital A thesis submitted in the partial fulfillment of the degree of clinical MD in pediatrics and child health University of Khartoum By DR. AMNA ABDEL KHALIG MOHAMED ATTAR MBBS University of Khartoum Supervisor PROF. SALAH AHMED IBRAHIM MD, FRCP, FRCPCH Department of Pediatrics and Child Health University of Khartoum University of Khartoum The Graduate College Medical and Health Studies Board 2008 Dedication I dedicate my study to the Department of Pediatrics University of Khartoum hoping to be a true addition to neonatal care practice in Sudan. i Acknowledgment I would like to express my gratitude to my supervisor Prof. Salah Ahmed Ibrahim, Professor of Peadiatric and Child Health, who encouraged me throughout the study and provided me with advice and support. I am also grateful to Dr. Osman Suleiman Al-Khalifa, the Dermatologist for his support at the start of the study. Special thanks to the staff at Omdurman Maternity Hospital for their support. I am also grateful to all mothers and newborns without their participation and cooperation this study could not be possible. Love and appreciation to my family for their support, drive and kindness. ii Table of contents Dedication i Acknowledgement ii Table of contents iii English Abstract vii Arabic abstract ix List of abbreviations xi List of tables xiii List of figures xiv Chapter One: Introduction & Literature Review 1.1 The skin of NB 1 1.2 Traumatic lesions 5 1.3 Desquamation 8 1.4 Lanugo hair 9 1.5