Staffing Levels NY Nursing Homes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 )
NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 ) County Nursing Home Address Phone # Hours of Operation Location of Drop‐off 780 Albany Shaker Rd., Thursdays Albany County Nursing Home 518-869-2231 Receiving Department Albany Albany, 12111 8 AM- Noon 180 Washington Ave. Ext., Daughters Of Sarah Nursing Center 518-456-7831 8 AM-4 PM Reception desk in lobby Albany Albany, 12203 Reception Main Campus - 40 Autumn Drive, Sharps received in an Eddy Village Green at Beverwyck 518-482-8774 8 AM-8 PM Slingerlands, 12159 appropriate sealed puncture Albany proof container Guilderland Center Rehabilitation 428 Route 146, Guilderland, 518-861-5141 10 AM-1 PM Lobby Albany and Extended Care Facility 12085 Our Lady Of Hope Residence-little 1 Jeanne Jugan Lane, Wednesday 518-785-4551 Lobby Albany Sisters Of The Poor Latham, 12110 9-11AM 2 Mercycare Lane, Monday thru Friday Main Lobby at Reception Our Lady Of Mercy Life Center 518-464-8100 Albany Guilderland, 12084 9:00AM -3:00PM Desk 27 Hackett Blvd., Monday-Friday St Margarets Center 518-591-3300 Reception Desk Albany Albany, 12208 8:00 AM-4 PM St Peter's Nursing and Rehabilitation 301 Hackett Blvd., Monday-Friday 518-525-7600 Reception Desk Albany Center Albany, 12208 10:00 AM-3 PM Teresian House Nursing Home Co 200 Washington Ave Ext., Front Entrance, Infrom 518-456-2000 8 AM-3 PM Albany Inc Albany 12203 Switchboard Operator Monday-Friday 140 West Main St., Cuba Memorial Hospital Inc Snf 585-968-2000 8 AM-4 PM Hospital Lobby Cuba 14727 Allegany Highland Park Rehabilitation -

A Guide to Innovative, Quality Long Term Care Options in New York
A Guide to Innovative, Quality e Long Term Care c Options in New York r u o S e r 555 WEST 57TH STREET a NEW YORK, NY 10019 212.258.5330 P 212.258.5331 F WWW.CCLC.ORG C CareSource A Guide to Innovative, Quality Long Term Care Options in New York CCLC Staff Contacts: About CCLC The Continuing Care Leadership Coalition (CCLC) is a membership Scott C. Amrhein 212.506.5409 and advocacy organization representing more than 100 of the President nation’s most innovative and comprehensive not-for-profit and public long term care organizations in the New York metropolitan Roxanne G.Tena-Nelson 212.506.5412 area and beyond. CCLC’s establishment in 2003 as an affiliate of the Vice President Greater New York Hospital Association (GNYHA) highlights the growing importance of continuing care services in today’s health Desmond D’Sa 212.506.5458 care marketplace. Associate Vice President of Finance and Reimbursement CCLC’s purpose is to shape, through advocacy, research, and education, Kelly L. Donohue an environment that supports the delivery of, and access to, contin- Director of Communications 212.506.5424 uing care services of the highest quality and to provide State and national leadership in advancing effective continuing care policies Jenifer H. Fergusson and practices through the collective experience, vision, and effort Events Planner 212.506.5426 of our members. LaSheandra Hunter 212.506.5429 The members of CCLC provide mission-driven services across the Operations Assistant continuum of care to people of all ages throughout the New York metropolitan area and beyond. -

A New Look at Our History: Part I
1 1 MOUNT SINAI QUEENS 0 2 r e b m e v o inside N A New Look at Our History: Part I In this issue of Inside Queens, we tell the story of our Hospital’s very beginnings up through the 1930s. We will continue the story from the postwar years to the present in the December issue. Up until 2010, the accepted thinking was that our history dated to 1910. Based on that date, we thought we reached our centennial as a hospital. In fact, research shows that Mount Sinai Queens can trace its history back almost 120 years to 1892, when Astoria was hailed as “one of New York’s fairest suburbs,” a magnet for the wealthy and successful. It was nearly 20 years earlier than we first thought, in 1892, that the Hospital was founded by a group of Astoria philanthropists, led by Mrs. Frank E. Hagemeyer and included Mrs. Blackwell, Riker and Rapelye—a who’s who of the elite in northwestern Queens. The original Astoria Hospital opened in a former private residence leased by William Steinway of the Steinway piano family, and was CONTINUED ON PAGE 2 The original hospital, today’s Annex Look Focus On: Emergency Department inside Whether patients walk in or arrive by ambulance, the Emergency Department (ED) sees a wide range Joining the Medical Staff: of emergency cases—stroke, cardiac, broken bones, Melissa S. Lee, MD infections, asthma and those needing stitches, the Take a Bow list is long. “What we do hasn’t changed over the years,” says Deborah Dean, MD, Acting Interim Great American Smokeout Director, shown here to the right, second from the September Employee of right. -

Hospital Postcard Collection
Center for Hospital and Healthcare Administration History Hospital Postcard Collection The postcard collection is comprised of over 2,500 postcards depicting primarily U.S. hospitals and medical centers. The collection provides a visual record of a variety of hospitals, sanitoriums, and other related buildings. The postcard collection dates from 1902. The attached description and inventory are available to aid researchers using the collection. The postcard collection is part of the Center for Hospital and Healthcare Administration History, sponsored jointly by the American Hospital Association and American College of Healthcare Executives, and is available for on-site use in the AHA Resource Center. Hospital Postcard Collection Description of the Collection The collection is arranged alphabetically by state, then by city, then by name of institution. Descriptive information has been taken verbatim from the postcards themselves. Any inconsistencies in format can be attributed to this fact. Postcards for an institution that have date information come before postcards for the same institution that are undated. A number in parentheses to the right of a hospital's name indicates the number of postcards for that hospital. If no number is indicated, then there is one postcard for that hospital. Each postcard has been placed in an archival sleeve. On each sleeve is an assigned number, in order for the postcards to remain in correct sequence (for example, Alabama postcards are labeled and numbered AL-1, AL-2, AL-3, etc.). STATE City Hospital ALABAMA Alexander City Russell Hospital Anniston Fort McClellan Post Hospital [2] Birmingham Baptist Hospital Crippled Children’s Clinic and Hospital Hillman Hospital Jefferson Hospital [3] - 1943, 1944 St. -

Top Doctors Queens 2020 11 19 Yp.Indd
NOVEMBER 12, 2020 • TOP DOCTORS IN QUEENS 5 14 CASTLE CONNOLLY TOP DOCTORS IN QUEENS • NOVEMBER 19, 2020 FOR BREAKING NEWS VISIT WWW.QNS.COM top doctors 2020 Forest Hills, NY 11375 Forest Hills, NY 11375 3916 Prince Street Suite 152 Mojgan N Neman-Kuighadush, (718) 544-6633 (718) 268-6120 Flushing, NY 11354 MD Long Island Jewish Medical Center Montefiore Moses Campus (718) 353-7701 Kew Gardens Medical New York Eye and Ear Infirmary of 8361 Abingdon Road Ellen I Edgar, MD Ian Chan, MD Mount Sinai Kew Gardens, NY 11415 Complete Neurological Care 38-08 Union Street, Suite 5D (718) 441-8666 112-47 Queens Boulevard, Suite 206 Flushing, NY 11354 Flushing Hospital Medical Forest Hills, NY 11375 (212) 941-2188 Otolaryngology Center (718) 544-4200 Myles Mittleman, MD Montefiore Moses Campus Allen J Fishman, MD 58-47 Francis Lewis Boulevard Benetta Yee, MD Fishman Center for Total Eye Care Bayside, NY 11364 ProHEALTH Forest Hills Pediatrics Jade Y Hon, MD 92-29 Queens Boulevard, Suite 2-I (718) 225-5400 108-48 70th Road 14105 Northern Blvd Rego Park, NY 11374 NewYork-Presbyterian Queens Forest Hills, NY 11375 Ste 1G (718) 261-7007 (718) 263-2072 Flushing, NY 11354 Flushing Hospital Medical Center Gary M Snyder, MD Long Island Jewish Medical (718) 888-9989 Ear, Nose & Throat Associates of NY Center Mount Sinai Hospital Cono M Grasso, MD 36-29 Bell Boulevard Floor 2 - Suite Comprehensive Ophthalmology 202 Demetrios A Karides, MD 83-05 Grand Avenue Bayside, NY 11361 Physical Medicine & Rehabilitation 23-09 31st Street, Suite 5 Elmhurst, NY 11373 -

Grapevine Summer 2019
THE ALUMNI MAGAZINE OF NYU SCHOOL OF MEDICINE SPRING/SUMMER 2019 High Tech High Touch School of Medicine Alumni Bring Innovation to Care, and Care to Innovation HENRY FELDMAN ’01 (RES. ’04), FACP, FHM DC 07/12/2019 PHOTO: JULIANA THOMAS THOMAS JULIANA PHOTO: Alumni giving helped us achieve this A Historic landmark; now your philanthropy is essential for sustaining our full-tuition Medical scholarship initiative in perpetuity. Help us continue to dramatically Breakthrough: reduce medical student debt, so future doctors can pursue their true passions. Free Tuition! For more information, contact Diana Robertson at 212-404-3510 NYU School of Medicine is or [email protected] now offering full-tuition Make an online donation at scholarships to all of its nyulangone.org/give/scholarships current and future students in the MD degree program. DC 07/12/2019 DEAN’S MESSAGE Dreaming Big Technology and innovation have long been core priorities of our institution. Early in my tenure, we invested in Epic, our electronic health records platform; this important— and, as it turned out, prescient—decision became the foundation for many innovative approaches to clinical care. In fact, innovation is at the forefront of everything we do. For example, our newest sites deeply programs, projects, and approaches worthy of integrate the power of technology in order such extraordinary tools and facilities. So I’m to transform how we deliver patient care, proud to present stories of some of our alumni perform research, and educate our outstanding who are doing just that: using technology, School of Medicine students. The Helen L. -
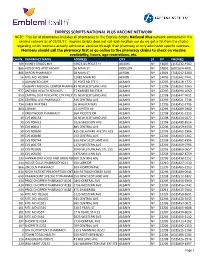
Express Scripts National Plus Vaccine Network
EXPRESS SCRIPTS NATIONAL PLUS VACCINE NETWORK NOTE: This list of pharmacies includes all pharmacies in the Express Scripts National Plus network contracted in the vaccine network as of 02/01/17. Express Scripts does not call each location nor do we get a list from the chains regarding which locations actually administer vaccines through their pharmacy or only administer specific vaccines. Members should call the pharmacy first or go online to the pharmacy chains to check on vaccine availability, hours, age restrictions, etc. CHAIN PHARMACY NAME ADDRESS CITY ST ZIP PHONE() 109 KINNEY DRUGS #04 10923 US ROUTE 11 ADAMS NY 13605 (315)232-4562 866 ADDISON'S APOTHECARY 36 MAIN ST ADDISON NY 14801 (607)504-4091 866 AKRON PHARMACY 58 MAIN ST AKRON NY 14001 (716)542-6300 56 RITE AID #10804 12983 MAIN RD AKRON NY 14001 (716)542-9761 0 ADVANCED CARE 25 POST RD STE 5 ALBANY NY 12205 (518)218-1772 0 ALBANY MEDICAL CENTER PHARMACY43 NEW SCOTLAND AVE ALBANY NY 12208 (518)262-3263 977 ANTHEM HEALTH SERVICES 57 KARNER RD STE B ALBANY NY 12205 (518)690-1060 953 CAPITAL DIST PSYCHTRC CTR PHCY 75 NEW SCOTLAND AVE ALBANY NY 12208 (518)447-9611 626 CENTRAL AVE PHARMACY 346 CENTRAL AVE ALBANY NY 12206 (518)621-7748 754 CHEM RX #7042 16 WALKER WAY ALBANY NY 12205 (518)452-7795 863 CORAM 12 JUPITER LN ALBANY NY 12205 (518)689-2900 0 CRESTWOOD PHARMACY 26A PICOTTE DR ALBANY NY 12208 (518)435-2315 39 CVS #00134 16 NEW SCOTLAND AVE ALBANY NY 12208 (518)434-0677 39 CVS #00413 1026 MADISON AVE ALBANY NY 12208 (518)489-8516 39 CVS #00417 885 CENTRAL AVE ALBANY NY 12206 -

Download All Timelines
Historical Timeline of the Department of Medicine NewYork-Presbyterian Hospital/Weill Cornell Medical Center Prior to 1932 1932-1939 1940-1949 1950-1959 1960-1969 1970-1979 1980-1989 1990-2007 Date Event 1791 General History New York Hospital, chartered in 1771, opens at its first location on Broadway between Duane and Worth Streets. The Departments of Medicine and Surgery provide the patient care. 1892 Division History: Infectious Diseases New York Hospital hires Dr. Albert Stanard, a specialist in contagious diseases. 1898 General History: Cornell University Medical College is established. The Department of Medicine provides medical students with basic clinical medical training. In addition, medical specialties are taught in the following special departments: Dermatology and Nervous Diseases (later called Neurology). W. Gilman Thompson is the first chairman. 1908 Division History: Pulmonary Care New York Hospital establishes a tuberculosis department in its Outpatient Department at its second location on West 15th and 16th Streets between Fifth and Sixth Avenues. 1908 Division History: Neurology New York Hospital hires Dr. J. Ramsey Hunt, a specialist in neurology. 1909 Research Highlight: Allergy and Immunology Drs. Robert Cooke and Arthur Coca begin their allergy research with an emphasis on hay fever and anaphylaxis at Cornell University Medical College under the Department of Experimental Therapeutics. Around 1918, their laboratory is placed under the Department of Bacteriology and Immunology. 1911- Division History: Second (Cornell) Medical Division 1967 Cornell University Medical College begins an affiliation with Bellevue Hospital to operate the Second (Cornell) Medical Division. This affiliation continues at the medical center. 1912 Division History: Cardiology New York Hospital opens an evening heart clinic. -

NYU Hospitals Center
NYU Hospitals Center Community Health Needs Assessment and Community Service Plan 2017-2019 Adopted June 2016 Copies of this document can be downloaded from the NYU Langone Medical Center website at: http://www.nyulangone.org/our-story/community-health-needs-assessment-service-plan and http://www.lutheranhealthcare.org/Main/CommunityServicePlan.aspx. For questions and comments, please contact Sue A. Kaplan, JD, Research Associate Professor, Department of Population Health, NYU Langone at: [email protected] or Kathleen Hopkins, Vice President for Community Programs, NYU Lutheran at: [email protected]. 1 Table of Contents Section Pages Overview 1-2 COMMUNITY HEALTH NEEDS ASSESSMENT 3-17 I. Hospitals Center’s Mission Statement 3-4 II. Definition and Brief Description of Communities Served 4-10 The Lower East Side and Chinatown 4-7 Sunset Park 7-10 Red Hook 10 III. Public Participation 10-11 IV. Assessment and Selection of Public Health Priorities 11-17 A. Priority Area: Preventing Chronic Disease 11-14 Preventing and addressing obesity 11-13 Reducing tobacco use 13-14 B. Priority Area: Promoting Healthy Women, Infants and Children 14-15 Supporting families through parenting, early childhood, and teen pregnancy 14-15 prevention programs C. Community needs not addressed and why 15 D. Information gaps that limit NYUHC’s ability to assess the community’s health 16 needs E. Existing facilities and resources 16-17 COMMUNITY SERVICE PLAN/IMPLEMENTATION STRATEGY 17-41 New York State and City public health priorities 17 Addressing health -

Who Shall Take Care of Our Sick? Bernadette Mccauley
Who Shall Take Care of Our Sick? Bernadette McCauley Published by Johns Hopkins University Press McCauley, Bernadette. Who Shall Take Care of Our Sick? Roman Catholic Sisters and the Development of Catholic Hospitals in New York City. Johns Hopkins University Press, 2005. Project MUSE. doi:10.1353/book.62237. https://muse.jhu.edu/. For additional information about this book https://muse.jhu.edu/book/62237 [ Access provided at 1 Oct 2021 03:58 GMT with no institutional affiliation ] This work is licensed under a Creative Commons Attribution 4.0 International License. Who Shall Take Care of Our Sick? Medicine, Science, and Religion in Historical Context Ronald L. Numbers, Consulting Editor Who Shall Take Care of Our Sick? Roman Catholic Sisters and the Development of Catholic Hospitals in New York City Bernadette McCauley The Johns Hopkins University Press baltimore © 2005 The Johns Hopkins University Press All rights reserved. Published 2005 Printed in the United States of America on acid-free paper 2 4 6 8 9 7 5 3 1 The Johns Hopkins University Press 2715 North Charles Street Baltimore, Maryland 21218-4363 www.press.jhu.edu Library of Congress Cataloging-in-Publication Data McCauley, Bernadette. Who shall take care of our sick? : Roman Catholic sisters and the development of Catholic hospitals in New York City / Bernadette McCauley. p. cm. — (Medicine, science, and religion in historical context) Includes bibliographical references and index. ISBN 0-8018-8216-8 (hardcover : alk. paper) 1. Catholic hospitals—New York (State)—New York—History. I. Title. II. Series. RA975.C37M38 2005 362.11Ј097471—dc22 2005000735 A catalog record for this book is available from the British Library. -
Report Resumes
REPORT RESUMES ED 012 983 'EC 000 244 MENTAL HEALTH DIRECTORY, 1966. BY- YOLLES, STANLEY F. AND OTHERS PUBLIC HEALTH SERVICE, BETHESDA, MD. REPORT NUMBER PI-IS-PUB-1517 PUB DATE 66 FORS PRICE MF-$1.00HC-$8.88 222F. DESCRIPTORS- *DIRECTORIES, *MENTAL HEALTH PROGRAMS, MENTAL HEALTH, NATIONAL CLEARINGHOUSE FOR MENTAL HEALTH INFORMATION THE DIRECTORY IS INTENDED AS A,REFERENCE GUIDE TO MENTAL HEALTH PROGRAMS AND SERVICES THROUGHOUT THE UNITED STATES. IT IS ORGANIZED INTO A FEDERAL SECTION AND A STATE AND COMMUNITY SECTION, EACH OF WHICH IS PRECEDED BY AN INTRODUCTORY STATEMENT CONCERNING THE LISTINGS IN THAT SECTION. ADDRESSES AND SHORT DESCRIPTIONS OF THE MAJOR MENTAL HEALTH PROGRAMS ARE GIVEN FOR OVER 2,000 OUTPATIENT PSYCHIATRIC CLINICS ANC DAY-NIGHT SERVICES IN EACH OF THE STATES. LISTINGS ARE ALPHABETICAL BY STATE, BY CITIES WITHIN THE STATES, AND BY , FACILITIES. PRIVATE MENTAL HOSPITALS, VETERANS ADMINISTRATION HOSPITALS, AND GENERAL HOSPITALS WITH PSYCHIATRIC SERVICES ARE NOT INCLUDED IN THE DIRECTORY. IN ADDITION, THERE IS A LISTING OF MENTAL HEALTH ASSOCIATIONS AND OF OTHER SOURCES OF MENTAL HEALTH INFORMATION. THIS DOCUMENT WAS PUBLISHED BY THE U.S. GOVERNMENT PRINTING OFFICE, WASHINGTON, D.C. $0.60. (RS) . %. NATIONAL CLEARINGHOUSE FOR MENTAL HEALTH INFORMATION 1 -1, w r. 4 , ..-,:;'- U.S..IDEPARTMENVOF___ HEALTH, k5UCA_ -_,' ii. f-ELFARE Public Health Service P .r- 4 The National Clearinghouse for Mental Healthinformation is thescientific and professional informationcenter of the NationalInstitute of MentalHealth - a - DNAL CLEARINGHOUSE FOR MENTAL HEALTH INFORMATION Mental Health Directory 1966 Includes National Institute of Mental Health State Departments Dealing with Mental Health and Mental Retardation State Hospitals for the Mentally Ill and Mentally Retarded Outpatient Psychiatric Clinics and Day-Night Services Mental Health Associations and Other Sources of Mental Health Information U.S. -
Where to Find Medical Records for Closed Hospitals in New York State
Where to Find Medical Records for Closed Hospitals in New York State This document is a list of the last known contacts for storage of hospital medical records in New York State. While every attempt is made to update this list, records may have been relocated, discarded or destroyed in accordance with retention requirements. Note that if there is no location information listed, the Department does not have any information available regarding the location of the records for the facility. Updates to the information on this list may be submitted by selecting “General Inquiries” from the Subject drop down box in the following link: https://apps.health.ny.gov/surveyd8/email-hospdtc#no-back - For information about locating records from psychiatric hospitals, please see the FAQs from the NYS Office of Mental Health at the following link: https://www.omh.ny.gov/omhweb/faq/ - For information on closed hospitals in New York City the following links may be helpful: - https://en.wikipedia.org/wiki/List_of_hospitals_in_New_York_City - http://newyork.resiliencesystem.org/sites/default/files/closed_hospitals.txt Medical Records for Closed Private Practitioners For information about locating medical records from closed private practitioners, you may contact the Office of Professional Medical Conduct at the following link: https://www.health.ny.gov/professionals/doctors/conduct/ https://www.health.ny.gov/professionals/doctors/conduct/contact.htm New York State Education Law 6530.32, available at the link below, establishes the requirements for retention of records: https://www.health.ny.gov/professionals/office-based_surgery/law/6530.htm Unless otherwise provided by law, all patient records must be retained for at least six years.