Profiles in Quality and Patient Safety 2019 | 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![NYSNA Pension Plan New Participant Information • (877) RN BENEFITS [762-3633] • Rnbenefits.Org](https://docslib.b-cdn.net/cover/2994/nysna-pension-plan-new-participant-information-877-rn-benefits-762-3633-rnbenefits-org-242994.webp)
NYSNA Pension Plan New Participant Information • (877) RN BENEFITS [762-3633] • Rnbenefits.Org
NYSNA Pension Plan New Participant Information • (877) RN BENEFITS [762-3633] • rnbenefits.org Defined benefit plan • Once a participant has completed five years of credited service, that participant will be VESTED and upon retirement will receive a monthly pension benefit for the rest of his/her life. Employer makes all contributions • RN contributes nothing Portable between more than 30 participating facilities in the New York City area (see back) How the pension benefit is calculated • Mathematical formula that recognizes earnings (base salary and experience differential only) and years of credited service • Based on the highest final average earnings for any five complete calendar years during the last 10 years of covered employment immediately before termination 3 retirement options to choose from For more detailed information on these options, please refer to your Welcome to the Pension Plan folder Normal retirement starting at age 65 Early retirement (unreduced) Must retire from active covered employment between the ages of 60 and 64 and have at least 20 years of credited service Early retirement Must retire between the ages of 55 and 64 (reduced by 1/2% for each month that early retirement precedes normal retirement at age 65) The information contained herein should not be viewed as a substitute for the Plan document, the most recent Summary Plan Description, and any relevant Summary of Material Modifications. In case of discrepancies or contradictions, the language and terms of the Plan document, the SPD, and SMMs shall prevail. 9/2020 Deferred Vested Benefit • Available to participants who are vested and leave the Plan prior to being eligible for retirement reductions • Payable at Normal Retirement age 65 with no reductions or between age 55 and 64 with early retirement reductions The Preretirement Survivor Benefit • If a vested participant dies before she/he retires • If married, the spouse is automatically the beneficiary. -

NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 )
NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 ) County Nursing Home Address Phone # Hours of Operation Location of Drop‐off 780 Albany Shaker Rd., Thursdays Albany County Nursing Home 518-869-2231 Receiving Department Albany Albany, 12111 8 AM- Noon 180 Washington Ave. Ext., Daughters Of Sarah Nursing Center 518-456-7831 8 AM-4 PM Reception desk in lobby Albany Albany, 12203 Reception Main Campus - 40 Autumn Drive, Sharps received in an Eddy Village Green at Beverwyck 518-482-8774 8 AM-8 PM Slingerlands, 12159 appropriate sealed puncture Albany proof container Guilderland Center Rehabilitation 428 Route 146, Guilderland, 518-861-5141 10 AM-1 PM Lobby Albany and Extended Care Facility 12085 Our Lady Of Hope Residence-little 1 Jeanne Jugan Lane, Wednesday 518-785-4551 Lobby Albany Sisters Of The Poor Latham, 12110 9-11AM 2 Mercycare Lane, Monday thru Friday Main Lobby at Reception Our Lady Of Mercy Life Center 518-464-8100 Albany Guilderland, 12084 9:00AM -3:00PM Desk 27 Hackett Blvd., Monday-Friday St Margarets Center 518-591-3300 Reception Desk Albany Albany, 12208 8:00 AM-4 PM St Peter's Nursing and Rehabilitation 301 Hackett Blvd., Monday-Friday 518-525-7600 Reception Desk Albany Center Albany, 12208 10:00 AM-3 PM Teresian House Nursing Home Co 200 Washington Ave Ext., Front Entrance, Infrom 518-456-2000 8 AM-3 PM Albany Inc Albany 12203 Switchboard Operator Monday-Friday 140 West Main St., Cuba Memorial Hospital Inc Snf 585-968-2000 8 AM-4 PM Hospital Lobby Cuba 14727 Allegany Highland Park Rehabilitation -

Non-Preferred Facilities You Will Pay More at These Hospitals
Non-preferred Facilities You will pay more at these hospitals. The copay for planned inpatient admissions is $1,000. The copay for outpatient hospital care is $250. NewYork-Presbyterian Health System NewYork-Presbyterian Allen Hospital NewYork-Presbyterian Lower Manhattan NewYork-Presbyterian Och Spine Hospital Hospital NewYork-Presbyterian / Weill Cornell NewYork-Presbyterian Morgan Stanley Medical Center Children's Hospital NewYork-Presbyterian / Columbia University Gracie Square Hospital Medical Center Payne Whitney Clinic NewYork-Presbyterian David H. Koch Center Columbia Doctors New York Presbyterian NewYork-Presbyterian Komansky Children's Imaging Hospital Weill Cornell Imaging at New York The Rogosin Institute (Manhattan locations) Presbyterian And all Manhattan outpatient facilities owned or affiliated with NewYork-Presbyterian Health System Northwell Health Cohen Children's Medical Center North Shore University Hospital Crouse Hospital Northern Westchester Hospital Glen Cove Hospital Peconic Bay Medical Center Huntington Hospital Phelps Hospital Lenox Hill Hospital Plainview Hospital Long Island Jewish Forest Hills South Oaks Hospital Long Island Jewish Medical Center Southside Hospital Long Island Jewish Valley Stream Staten Island University Hospital Maimonides Medical Center Syosset Hospital Manhattan Eye, Ear, and Throat Hospital Zucker Hillside Hospital Mather Hospital Nassau University Medical Center And all outpatient facilities owned or affiliated with Northwell Health NYU Langone Health -

OMH Monthly Report: December 2020
of Mental Health December 2020 Monthly Report OMH Facility Performance Metrics and Community Service Investments Table of Contents December 2020 Report Overview .............................................................................................1 Table 1: NYS OMH State PC Inpatient Descriptive Measures ................................................ 2 Table 2: Transformation and Article 28/31 RIV Summary ..................................................... 3 Table 3 Series: Reinvestment by Facility Catchment Area ..............................................4 -18 State Psychiatric Center Reinvestment Tables Table 3a: Greater Binghamton Health Center .......................................................................... 4 Table 3b: Elmira Psychiatric Center .........................................................................................5 Table 3c: St. Lawrence Psychiatric Center .............................................................................. 6 Table 3d: Sagamore Children’s Psychiatric Center .................................................................. 7 Table 3e: Pilgrim Psychiatric Center ........................................................................................8 Table 3f: Western NY Children’s – Buffalo Psychiatric Center ................................................. 9 Table 3g: Rochester Psychiatric Center ................................................................................. 10 Table 3h: New York City Psychiatric Centers ........................................................................ -

Carrier Hospital Guide
2021 Carrier Hospital Guide EmblemHealth EmblemHealth EmblemHealth Oscar Oxford Oxford Hospital Name Healthfirst County Prime Select Care Millenium Circle Metro Liberty Albert Einstein College of Medicine √ √ √ √ √ Bronx BronxCare Health System √ √ √ √ Bronx Calvary Hospital √ √ √ √ Bronx Jacobi Medical Center √ √ √ √ √ Bronx Lincoln Medical & Mental Health Center √ √ √ √ √ Bronx Montefiore Medical Center √ √ √ √ Bronx Montefiore Westchester Square √ √ Bronx North Central Bronx Hospital √ √ √ √ √ Bronx St. Barnabas Hospital √ √ √ √ √ √ Bronx Total Hospitals in Bronx County 9 4 4 7 2 7 7 Midhudson Regional Hospital √ √ √ Dutchess Northern Dutchess Hospital √ √ √ √ Dutchess Vassar Brothers Medical Center √ √ √ √ Dutchess Total Hospitals in Dutchess County 3 2 0 0 0 3 3 Brookdale University Hospital Medical Center √ √ √ √ √ Kings Brooklyn Hospital Center √ √ √ √ √ √ √ Kings Coney Island Hospital Center √ √ √ √ √ Kings Interfaith Medical Center √ √ √ √ √ Kings Kings County Hospital Center √ √ √ √ √ Kings Kingsbrook Jewish Medical Center √ √ √ √ √ Kings Maimonides Medical Center √ √ √ Kings Mount Sinai Brooklyn √ √ √ √ √ √ √ Kings NYC Health + Hospitals √ √ √ √ √ Kings New York Community Hospital of Brooklyn √ √ √ √ Kings New York Presbyterian Methodist √ √ √ √ √ Kings NYU Lutheran Medical Center √ √ √ √ Kings SUNY Downstate Medical Center √ √ √ √ Kings Woodhull Medical and Mental Health Center √ √ √ √ √ Kings Wyckoff Heights Medical Center √ √ √ √ Kings Total Hospitals in Kings County 15 6 11 10 3 13 15 Cohen Children's Medical Center √ √ -
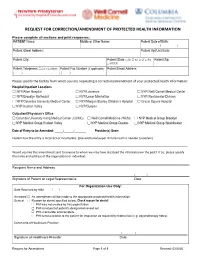
Request for Correction/Amendment of Protected Health Information
REQUEST FOR CORRECTION/AMENDMENT OF PROTECTED HEALTH INFORMATION Please complete all sections and print responses: PATIENT Name: Middle or Other Name: Patient Date of Birth: / / Patient Street Address: Patient Apt/Unit/Suite: Patient City: Patient State: ☐ NY ☐ NJ ☐ CT ☐ PA Patient Zip: ☐ OTHER:___________________________ Patient Telephone: ☐ Cell or ☐ Home Patient Fax Number (if applicable): Patient Email Address: ( ) ( ) Please specify the facility from which you are requesting a correction/amendment of your protected health information: Hospital/Inpatient Locations ☐ NYP/Allen Hospital ☐ NYP/Lawrence ☐ NYP/Weill Cornell Medical Center ☐ NYP/Brooklyn Methodist ☐ NYP/Lower Manhattan ☐ NYP/Westchester Division ☐ NYP/Columbia University Medical Center ☐ NYP/Morgan Stanley Children’s Hospital ☐ Gracie Square Hospital ☐ NYP/Hudson Valley ☐ NYP/Queens Outpatient/Physician’s Office ☐ Columbia University Irving Medical Center (CUIMC) ☐ Weill Cornell Medicine (WCM) ☐ NYP Medical Group Brooklyn ☐ NYP Medical Group Hudson Valley ☐ NYP Medical Group Queens ☐ NYP Medical Group Westchester Date of Entry to be Amended: _____/______/_______ Provider(s) Seen: __________________________________________ Explain how the entry is incorrect or incomplete. (Use additional paper if more room is needed to explain) ___________________________________________________________________________________________________________ Would you like this amendment sent to anyone to whom we may have disclosed the information in the past? If so, please specify the name and -

A Guide to Innovative, Quality Long Term Care Options in New York
A Guide to Innovative, Quality e Long Term Care c Options in New York r u o S e r 555 WEST 57TH STREET a NEW YORK, NY 10019 212.258.5330 P 212.258.5331 F WWW.CCLC.ORG C CareSource A Guide to Innovative, Quality Long Term Care Options in New York CCLC Staff Contacts: About CCLC The Continuing Care Leadership Coalition (CCLC) is a membership Scott C. Amrhein 212.506.5409 and advocacy organization representing more than 100 of the President nation’s most innovative and comprehensive not-for-profit and public long term care organizations in the New York metropolitan Roxanne G.Tena-Nelson 212.506.5412 area and beyond. CCLC’s establishment in 2003 as an affiliate of the Vice President Greater New York Hospital Association (GNYHA) highlights the growing importance of continuing care services in today’s health Desmond D’Sa 212.506.5458 care marketplace. Associate Vice President of Finance and Reimbursement CCLC’s purpose is to shape, through advocacy, research, and education, Kelly L. Donohue an environment that supports the delivery of, and access to, contin- Director of Communications 212.506.5424 uing care services of the highest quality and to provide State and national leadership in advancing effective continuing care policies Jenifer H. Fergusson and practices through the collective experience, vision, and effort Events Planner 212.506.5426 of our members. LaSheandra Hunter 212.506.5429 The members of CCLC provide mission-driven services across the Operations Assistant continuum of care to people of all ages throughout the New York metropolitan area and beyond. -

Newyork-Presbyterian Hospital Annual Report
Letters from Home 2006-2007 Annual Report NEWYORK-PRESBYTERIAN HOSPITAL Important Telephone Numbers THE ALLEN PAVILION OF NEWYORK-PRESBYTERIAN HOSPITAL NEWYORK-PRESBYTERIAN HOSPITAL/ WEILL CORNELL MEDICAL CENTER General Information (212) 932-4000 Patient Information (212) 932-4300 General Information (212) 746-5454 Admitting (212) 932-5079 Patient Information (212) 746-5000 Emergency Department (212) 932-4245 Admitting (212) 746-4250 Patient Services (212) 932-4321 Ambulance Services Dispatcher (212) 472-2222 Development (212) 821-0500 Emergency Department NEWYORK-PRESBYTERIAN HOSPITAL/ Adult (212) 746-5050 COLUMBIA UNIVERSITY MEDICAL CENTER Pediatric (212) 746-3300 General Information (212) 305-2500 Psychiatry (212) 746-0711 Patient Information (212) 305-3101 Human Resources (212) 746-1409 Admitting Marketing (212) 585-6800 Main Reception (212) 305-7091 NewYork-Presbyterian Sloane Hospital for Women (212) 342-1759 Healthcare System (212) 746-3577 Ambulance Services Dispatcher (212) 305-9999 Patient Services (212) 746-4293 Development (212) 342-0799 Physician Referral Service (800) 822-2694 Emergency Department Psychiatry, Payne Whitney Manhattan Adult (212) 305-6204 Referrals and Evaluation (888) 694-5700 Pediatric (212) 305-6628 General Information (212) 746-5700 Psychiatry (212) 305-6587 Public Affairs (212) 821-0560 Human Resources (212) 305-5625 Marketing (212) 821-0634 WESTCHESTER DIVISION OF NEWYORK-PRESBYTERIAN HOSPITAL Patient Services (212) 305-5904 Physician Referral Service (877) NYP-WELL General Information (914) 682-9100 Public Affairs (212) 305-5587 Payne Whitney Westchester Referrals and Evaluation (888) 694-5700 MORGAN STANLEY CHILDREN’S HOSPITAL Table of Contents OF NEWYORK-PRESBYTERIAN Physician Referral (800) 245-KIDS Letters from Home — 2 General Information (212) 305-KIDS Patient Information (212) 305-3101 Noteworthy — 24 Admitting (212) 305-3388 Leadership Report — 26 Emergency Department (212) 305-6628 Facts and Financials — 31 Dr. -

A New Look at Our History: Part I
1 1 MOUNT SINAI QUEENS 0 2 r e b m e v o inside N A New Look at Our History: Part I In this issue of Inside Queens, we tell the story of our Hospital’s very beginnings up through the 1930s. We will continue the story from the postwar years to the present in the December issue. Up until 2010, the accepted thinking was that our history dated to 1910. Based on that date, we thought we reached our centennial as a hospital. In fact, research shows that Mount Sinai Queens can trace its history back almost 120 years to 1892, when Astoria was hailed as “one of New York’s fairest suburbs,” a magnet for the wealthy and successful. It was nearly 20 years earlier than we first thought, in 1892, that the Hospital was founded by a group of Astoria philanthropists, led by Mrs. Frank E. Hagemeyer and included Mrs. Blackwell, Riker and Rapelye—a who’s who of the elite in northwestern Queens. The original Astoria Hospital opened in a former private residence leased by William Steinway of the Steinway piano family, and was CONTINUED ON PAGE 2 The original hospital, today’s Annex Look Focus On: Emergency Department inside Whether patients walk in or arrive by ambulance, the Emergency Department (ED) sees a wide range Joining the Medical Staff: of emergency cases—stroke, cardiac, broken bones, Melissa S. Lee, MD infections, asthma and those needing stitches, the Take a Bow list is long. “What we do hasn’t changed over the years,” says Deborah Dean, MD, Acting Interim Great American Smokeout Director, shown here to the right, second from the September Employee of right. -

MEDICAL CENTER ARCHIVES of NEWYORK-PRESBYTERIAN/WEILL CORNELL 1300 York Avenue #34 New York, NY 10065 Finding Aid to the RECORDS
MEDICAL CENTER ARCHIVES OF NEWYORK-PRESBYTERIAN/WEILL CORNELL 1300 York Avenue #34 New York, NY 10065 Finding Aid to the RECORDS OF COSMO LACOSTA Dates of Records: 1962-1989 197.5 Linear Inches (16 Boxes) Finding Aid Prepared By: Elizabeth Shepard Associate Archivist November 2014 © 2014 Medical Center Archives of NewYork-Presbyterian/Weill Cornell 2 PROVENANCE: This collection is a consolidation of four donations that Cosmo Lacosta made to the archives. They were originally cataloged under the departments that he held at the time of the donation. However, all of the records extended into different positions that he held at the Division of Professional Services and General Services (later called General and Support Services). Due to the overlap of these collections, it was decided to consolidate them into one collection to make it easier to access these records. The collections were donated as follow: General Services, date of donation not noted General and Support Services, June 8, 1988 Associate Director, Division of Professional Services, November 1995 Burn Center Records, date of donation not noted ADMINISTRATIVE/BIOGRAPHICAL NOTE: Cosmos LaCosta earned a BS in Education in 1963 from Fordham University and a MA in Public Administration (Health Administration) in 1973. He served with the U.S. Army at the hospital in Orleans, France, 1964-1965 and the U.S. Reserves from 1966-1968. He first joined the staff of New York Hospital in 1967 as an executive assistant. He moved up the ranks to assistant director (1971-1975), associate director of Professional Services (1975-1983), and Executive Associate Director of General Services (1983- 1989). -

Hospital Postcard Collection
Center for Hospital and Healthcare Administration History Hospital Postcard Collection The postcard collection is comprised of over 2,500 postcards depicting primarily U.S. hospitals and medical centers. The collection provides a visual record of a variety of hospitals, sanitoriums, and other related buildings. The postcard collection dates from 1902. The attached description and inventory are available to aid researchers using the collection. The postcard collection is part of the Center for Hospital and Healthcare Administration History, sponsored jointly by the American Hospital Association and American College of Healthcare Executives, and is available for on-site use in the AHA Resource Center. Hospital Postcard Collection Description of the Collection The collection is arranged alphabetically by state, then by city, then by name of institution. Descriptive information has been taken verbatim from the postcards themselves. Any inconsistencies in format can be attributed to this fact. Postcards for an institution that have date information come before postcards for the same institution that are undated. A number in parentheses to the right of a hospital's name indicates the number of postcards for that hospital. If no number is indicated, then there is one postcard for that hospital. Each postcard has been placed in an archival sleeve. On each sleeve is an assigned number, in order for the postcards to remain in correct sequence (for example, Alabama postcards are labeled and numbered AL-1, AL-2, AL-3, etc.). STATE City Hospital ALABAMA Alexander City Russell Hospital Anniston Fort McClellan Post Hospital [2] Birmingham Baptist Hospital Crippled Children’s Clinic and Hospital Hillman Hospital Jefferson Hospital [3] - 1943, 1944 St. -

Top Doctors Queens 2020 11 19 Yp.Indd
NOVEMBER 12, 2020 • TOP DOCTORS IN QUEENS 5 14 CASTLE CONNOLLY TOP DOCTORS IN QUEENS • NOVEMBER 19, 2020 FOR BREAKING NEWS VISIT WWW.QNS.COM top doctors 2020 Forest Hills, NY 11375 Forest Hills, NY 11375 3916 Prince Street Suite 152 Mojgan N Neman-Kuighadush, (718) 544-6633 (718) 268-6120 Flushing, NY 11354 MD Long Island Jewish Medical Center Montefiore Moses Campus (718) 353-7701 Kew Gardens Medical New York Eye and Ear Infirmary of 8361 Abingdon Road Ellen I Edgar, MD Ian Chan, MD Mount Sinai Kew Gardens, NY 11415 Complete Neurological Care 38-08 Union Street, Suite 5D (718) 441-8666 112-47 Queens Boulevard, Suite 206 Flushing, NY 11354 Flushing Hospital Medical Forest Hills, NY 11375 (212) 941-2188 Otolaryngology Center (718) 544-4200 Myles Mittleman, MD Montefiore Moses Campus Allen J Fishman, MD 58-47 Francis Lewis Boulevard Benetta Yee, MD Fishman Center for Total Eye Care Bayside, NY 11364 ProHEALTH Forest Hills Pediatrics Jade Y Hon, MD 92-29 Queens Boulevard, Suite 2-I (718) 225-5400 108-48 70th Road 14105 Northern Blvd Rego Park, NY 11374 NewYork-Presbyterian Queens Forest Hills, NY 11375 Ste 1G (718) 261-7007 (718) 263-2072 Flushing, NY 11354 Flushing Hospital Medical Center Gary M Snyder, MD Long Island Jewish Medical (718) 888-9989 Ear, Nose & Throat Associates of NY Center Mount Sinai Hospital Cono M Grasso, MD 36-29 Bell Boulevard Floor 2 - Suite Comprehensive Ophthalmology 202 Demetrios A Karides, MD 83-05 Grand Avenue Bayside, NY 11361 Physical Medicine & Rehabilitation 23-09 31st Street, Suite 5 Elmhurst, NY 11373