NYU Hospitals Center
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IMG-Friendly Hospitals” in the United States of America
List of “IMG-friendly hospitals” in the United States of America. The authors do not guarantee complete accuracy as this is a moving target. The list serves the purpose of giving you an idea of the programs that have historically been IMG- friendly. As outlined in the book “The International Medical Graduate’s Best Hope”, the authors do not advocate complete reliance on lists but rather encourage a one-on-one search of residency programs according to individual characteristics. STATE PROGRAM H-1B J1 GC ALABAMA Carraway Methodist Medical Center NO NO YES University of Alabama Medical Center ? ? YES Population: Time Zone: Weather: Cost of living: STATE PROGRAM H-1B J1 GC ARKANSAS University of Arkansas for Medical Sciences YES YES YES Population: Time Zone: Weather: Cost of living: STATE PROGRAM H-1B J1 GC ARIZONA Maricopa Medical Center NO NO YES Mayo Clinic Scottsdale NO YES YES University of Arizona & Affiliated Hospitals NO YES YES Population Time Zone Weather Cost of living STATE PROGRAM H-1B J1 GC CALIFORNIA Alameda County Medical Ctr/Highland NO NO YES Hospital Cedars-Sinai Medical Center NO YES YES Kaiser Permanente Med. Ctr., San Francisco NO NO YES Kaiser Permanente Med. Ctr., Santa Clara NO NO YES Kaiser Permanente Medical Center, Oakland NO YES YES Stanford University NO YES YES University of California at Los Angeles Med. NO YES YES Ctr. University of California at Los Angeles Med. NO YES YES Ctr. University of California at San Diego NO YES YES University of Southern California NO YES YES Population Time Zone Weather Cost of living STATE PROGRAM H-1B J1 GC COLORADO Exempla St. -
NYU Hospitals Center Request for Expansion of Existing Ambulance Service
NYU Hospitals Center Request for Expansion of Existing Ambulance Service PREPARED FOR: New York State Department of Health The Regional EMS Council of New York City PREPARED BY: NYU Hospitals Center Emergency Medical Services March 7th, 2016 Table of Contents Application Part I (Narrative) Introduction Section 1 - Selwices and Staffing - Existent and Proposed Section 2 - Population Demographics Section 3 - Description of Calls Section 4 - Response Times Section 5- Quality of Service Section 6 - Mutual Aid Section 7 - Member Qualifications and Sldli Retention Section 8 - Communications Section 9 - Fiscal Stability Section 10 - Organization and Administration Section 11 - Cost-Benefit Ratio Section 12 - Community and Government Support Section 13 - Reallocation of Existing Resources Section 14- Statement from Service Medical Director & ALS Level of Service Documentation Attachments Application Part II (State Forms and Competency and Fitness) Section 1 - Application for Expansion of EMS Selwice (DOH-BEMS 3777) Section 2 - Affirmation of Competency and Fitness (DOH-BEMS 3778) Section 3 - Resumes for Individuals Providing Affirmations of Competency and Fitness Application Part III (Letters of Endorsement) Section 1 - Sample Letter of Endorsement Section 2 - List of Individuals/Agencies to which Sample Letter of Endorsement was sent Section 3 - Letters of Endorsement Section 4 - Mail Receipts Application Part I (Narrative) Introduction NYU Hospitals Center ("NYUHC") is seeking to permanently expand its current operating territory of southwest Brooklyn (New York City 68 and 72 Police Precincts) to all of Brooklyn and Manhattan (the "Proposed Service Area"). Temporary expansion [for all five boroughs] was approved on March 4th, 2016 by the NYS Department of Health (see Attachment A). -
Charter Petition Review While Ensuring Ready Access to the DRL for Any Given Section of the Charter
PUC Triumph Charter Academy and PUC Triumph Charter High School A School of Partnerships to Uplift Communities (PUC) Valley Dr. Jacqueline Elliot Adriana Abich Partnerships to Uplift Communities (PUC) - Valley 1405 N. San Fernando Blvd. Suite 303 Burbank, CA 91502 818-559-7699 Voice 818-559-8641 Fax Submitted: September 14, 2015 PUC Triumph Charter Academy and PUC Triumph Charter High School Table of Contents ASSURANCES AND AFFIRMATION 4 ELEMENT 1 – THE EDUCATIONAL PROGRAM 6 GENERAL INFORMATION 6 1.1 COMMUNITY NEED FOR CHARTER SCHOOL 10 1.2 STUDENT POPULATION TO BE SERVED 32 1.3 Five Year Enrollment Plan 42 1.4 Surrounding Schools Demographic and Performance Data 43 1.5 VISION & MISSION 44 1.6 EDUCATED PERSON OF THE 21ST CENTURY 44 1.7 HOW LEARNING BEST OCCURS 46 1.8 HOW THE GOALS ENABLE SELF‐MOTIVATED, COMPETENT LIFE‐LONG LEARNERS 49 1.9 REQUIREMENTS OF CALIFORNIA EDUCATION CODE § 47605(B)(5)(A)(II) 52 1.10 INSTRUCTIONAL DESIGN 61 1.11 CURRICULUM 71 1.12 GRADUATION REQUIREMENTS 91 1.13 INSTRUCTIONAL METHODOLOGIES AND STRATEGIES 94 1.14 STUDENT MASTERY OF CA CCSS AND OTHER STATE CONTENT STANDARDS 96 1.15 DEVELOPMENT OF TECHNOLOGY‐RELATED SKILLS 100 1.16 ACADEMIC CALENDAR 102 1.17 DAILY SCHEDULES 103 1.18 INSTRUCTIONAL DAYS AND MINUTES 109 1.19 TEACHER RECRUITMENT 109 1.20 PROFESSIONAL DEVELOPMENT 111 1.21 MEETING THE NEEDS OF ENGLISH LEARNERS 117 1.22 MEETING THE NEEDS OF GIFTED STUDENTS 122 1.23 MEETING THE NEEDS OF STUDENTS ACHIEVING BELOW GRADE LEVEL 124 1.24 MEETING THE NEEDS OF SOCIO‐ECONOMICALLY DISADVANTAGED STUDENTS 132 1.25 MEETING -

Rheumatology
NYU Langone Medical Center 550 First Avenue, New York, NY 10016 nyulmc.org RHEUMATOLOGY 2014 YEAR IN REVIEW CONTENTS 1 Letter from the Chairs 2 Facts & Figures 1 Message from the Director 4 New & Noteworthy 2 Facts & Figures 6 Section 4 New & Noteworthy 42 Research 10 Clinical Care and Research 44 Education 11 Lupus and Neonatal Lupus 13 Behçet’s Syndrome 48 Publications 14 Rheumatology and Osteoporosis 5164 LoPsoriaticcations Arthritis 18 Rheumatoid Arthritis and Osteoarthritis 55 Leadership 20 Education & Training 56 NYU Langone Medical Center Facts & Figures 24 Professional Activities 57 NYU Langone Medical Center Leadership Design: Ideas On Purpose, www.ideasonpurpose.com 27 Leadership, Locations Produced by: Office of Communications and Marketing, NYU Langone Medical Center NYU LANGONE MEDICAL CENTER / RHEUMATOLOGY / 2014 PAGE 1 MESSAGE FROM THE DIRECTOR Dear Colleagues and Friends, The tripartite mission of our division is clear: Deliver comprehensive state-of-the-art clinical care, translate and integrate medicine and science, and increase the knowledge base of our trainees. I’m proud to report that in 2014, with the dedication of all faculty members, we have made significant strides in all three areas, as evidenced in the following pages. Under the guidance of our previous division director, Steven B. Abramson, MD, now chair of the Department of Medicine, the Judith and Stewart Colton Center for Autoimmunity was established. The center aims to advance discoveries about the microbiome and its relationship to autoimmune disease, and to leverage this new knowledge to develop strategies for prevention and JILL P. BUYON, MD treatment. Our vision of a comprehensive, multidisciplinary Psoriatic Arthritis Center dedicated to the bench-to-bedside integration of dermatology and Director, Division of Rheumatology, rheumatology has now been realized, and a strong laboratory research base will Department of Medicine stand behind this center to further our understanding of psoriatic arthritis and NYU Langone Medical Center develop novel therapies. -

Barbara Bowman Leadership Fellows Program
Barbara Cohort Bowman Leadership 2017 Fellows The Early Childhood Leadership Academy is pleased to present the policy memos developed by the 2017 Policy Cohort of the Barbara Bowman Leadership Fellows Program. Memos SPECIAL ACKNOWLEDGEMENTS Support The Early Childhood Leadership Academy at Erikson Institute gratefully acknowledges the support and generosity of The Irving B. Harris Foundation for its support of the Barbara Bowman Leadership Fellows program. BARBARA BOWMAN We are honored to have the program named after one of Erikson Institute’s founders, Barbara Taylor Bowman. Barbara’s legacy as an education activist, policy adviser, and early childhood practitioner matches the characteristics of the fellows this program aims to attract. Furthermore, her dedication to ensuring that diversity and equity are mutually reinforced provides the framework that supports the entire program experience. This effort draws from Erikson’s mission-driven work to ensure a future in which all children have equitable opportunities to realize their full potential through leadership and policy influence. Special thanks to President and CEO, Geoffrey A. Nagle for his continuous commitment to the program. ACKNOWLEDGEMENTS Participating Organizations TABLE OF CONTENTS ACCESS ..........................................................................................................1 CARISA HURLEY ...................................................................................................... 1 CINDY LA .............................................................................................................. -

NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 )
NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 ) County Nursing Home Address Phone # Hours of Operation Location of Drop‐off 780 Albany Shaker Rd., Thursdays Albany County Nursing Home 518-869-2231 Receiving Department Albany Albany, 12111 8 AM- Noon 180 Washington Ave. Ext., Daughters Of Sarah Nursing Center 518-456-7831 8 AM-4 PM Reception desk in lobby Albany Albany, 12203 Reception Main Campus - 40 Autumn Drive, Sharps received in an Eddy Village Green at Beverwyck 518-482-8774 8 AM-8 PM Slingerlands, 12159 appropriate sealed puncture Albany proof container Guilderland Center Rehabilitation 428 Route 146, Guilderland, 518-861-5141 10 AM-1 PM Lobby Albany and Extended Care Facility 12085 Our Lady Of Hope Residence-little 1 Jeanne Jugan Lane, Wednesday 518-785-4551 Lobby Albany Sisters Of The Poor Latham, 12110 9-11AM 2 Mercycare Lane, Monday thru Friday Main Lobby at Reception Our Lady Of Mercy Life Center 518-464-8100 Albany Guilderland, 12084 9:00AM -3:00PM Desk 27 Hackett Blvd., Monday-Friday St Margarets Center 518-591-3300 Reception Desk Albany Albany, 12208 8:00 AM-4 PM St Peter's Nursing and Rehabilitation 301 Hackett Blvd., Monday-Friday 518-525-7600 Reception Desk Albany Center Albany, 12208 10:00 AM-3 PM Teresian House Nursing Home Co 200 Washington Ave Ext., Front Entrance, Infrom 518-456-2000 8 AM-3 PM Albany Inc Albany 12203 Switchboard Operator Monday-Friday 140 West Main St., Cuba Memorial Hospital Inc Snf 585-968-2000 8 AM-4 PM Hospital Lobby Cuba 14727 Allegany Highland Park Rehabilitation -

Return of Organization Exempt from Income
l efile GRAPHIC p rint - DO NOT PROCESS As Filed Data - DLN: 93493042019134 Return of Organization Exempt From Income Tax OMB No 1545-0047 Form 990 Under section 501 (c), 527, or 4947 (a)(1) of the Internal Revenue Code ( except black lung benefit trust or private foundation) 2012 Department of the Treasury Internal Revenue Service 1-The organization may have to use a copy of this return to satisfy state reporting requirements A For the 2012 calendar year, or tax year beginning 07-01-2012 , 2012, and ending 06-30-2013 C Name of organization B Check if applicable D Employer identification number PEER HEALTH EXCHANGE INC F Address change 56-2374305 Doing Business As F Name change fl Initial return Number and street (or P 0 box if mail is not delivered to street address) Room/suite E Telephone number 70 GOLD STREET p Terminated (415)684-1230 (- Amended return City or town, state or country, and ZIP + 4 SAN FRANCISCO, CA 94133 I Application pending G Gross receipts $ 8,773,516 F Name and address of principal officer H(a) Is this a group return for LOUISE D LANGHEIER affiliates? (-Yes No 70 GOLD STREET SAN FRANCISCO,CA 94133 H(b) Are all affiliates included? F Yes F_ No If "No," attach a list (see instructions) I Tax-exempt status F 501(c)(3) 1 501(c) ( ) I (insert no ) (- 4947(a)(1) or F_ 527 H(c) Group exemption number - J Website :1- WWW PEERHEALTHEXCHANGE ORG K Form of organization F Corporation 1 Trust F_ Association (- Other 0- L Year of formation 2003 M State of legal domicile NY Summary 1 Briefly describe the organization's mission or most significant activities TO GIVE TEENAGERS THE KNOWLEDGE AND SKILLS THEY NEED TO MAKE HEALTHY DECISIONS w 2 Check this box if the organization discontinued its operations or disposed of more than 25% of its net assets 3 Number of voting members of the governing body (Part VI, line 1a) . -

The Blue and White
THE UNDERGRADUATE MAGAZINE OF COLUMBIA UNIVERSITY, EST. 1890 THE BLUE AND WHITE Vol. XIX No. III May 2013 Lies My Teacher Told Me What you need to know before you teach for America Paying it Forward Pervasive debt at Columbia's nontraditional college ALS O INSIDE: CULTURE! AND SUB-CULTURE! Conor Skelding, CC ’14, Editor in Chief ANNA BAHR, BC ’14, Managing Editor ALLIE CURRY, CC ’13, Senior Editor Will Holt, CC ’15, Senior Editor TORSTEN ODLAND, CC ’15, Senior Editor CLAIRE SABEL, CC ’13, Senior Editor JESSIE CHASAN-TABer, CC ’16, Layout Editor LEILA MGALOBLISHVILI, CC ’16, Senior Illustrator ZUZANA GIERTLOVA, BC ’14, Publisher SOMER OMAR, CC ’16, Public Editor Staff Writers NAOMI SHArp, CC ’15 ALEXANDER PINES, CC ’16 Contributors NAOMI COHen, CC ’15 KATIE DONAHoe, BC ’16 BRITT FOSSUM, CC ’16 LUCA MARZORAti, CC ’15 MATTHEW SCHANTZ, CC ’13 DANIEL STONE, CC ’16 ALEXANDRA SVOKOS, CC ’14 HALLIE NELL SWANSON, CC ’16 Artists JULIETTE CHEN, CC ’16 BRITT FOSSUM, CC ’16 JIYOON HAN, CC ’13 ANGEL JIANG, CC ’15 KATHARINE LIN, CC ’16 ELISA MIRKIL, CC ’16 ALEXANDER PINES, CC ’16 ANNE SCOTTI, CC ’16 HANK SHORB, CC ’16 Editors Emeriti SYLVIE KREKOW, BC ’13 BRIAN WAGNER, SEAS ’13 THE BLUE & WHITE Vol. XIX FAMAM EXTENDIMUS FACTIS No. III COLUMNS FEATURES 4 BLUEBOOK Sylvie Krekow & 10 AT TWO SWORDS’ LENGTH: SHOULD YOU GRADUATE? 6 BLUE NOTES Brian Wagner Our monthly prose and cons 8 CAMPUS CHARACTERS 12 VERILY VERITAS Will Holt 13 ALL BROOKLYN BEER TASTES THE SAME 27 CURIO COLUMBIANA A B&W editor hops to Brooklyn to see what’s brewing 28 SKETCHBOOK 34 MEASURE -
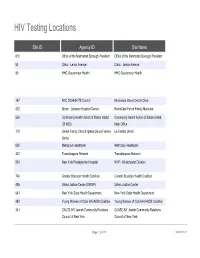
HIV Testing Locations
HIV Testing Locations Site ID Agency ID Site Name 810 Office of the Manhattan Borough President Office of the Manhattan Borough President 53 Clinic - Lenox Avenue Clinic - Lenox Avenue 90 HHC Gouverneur Health HHC Gouverneur Health 167 NYC DOHMH TB Control Morrisania Chest Center Clinic 822 Bronx - Lebanon Hospital Center BronxCare Fulton Family Medicine 524 Community Health Action of Staten Island Community Health Action of Staten Island- (CHASI) Main Office 119 United Family Church-Iglesia De La Familia La Familia Unida Unida 605 Metroplus Healthplan Metroplus Healthplan 442 Transdiaspora Network Transdiaspora Network 542 New York Presbyterian Hospital NYP - Westchester Division 746 Greater Brooklyn Health Coalition Greater Brooklyn Health Coalition 495 Urban Justice Center (SWOP) Urban Justice Center 641 New York State Health Department New York State Health Department 452 Young Women of Color HIV/AIDS Coalition Young Women of Color HIV/AIDS Coalition 341 CAUSE-NY Jewish Community Relations CAUSE-NY Jewish Community Relations Council of New York Council of New York Page 1 of 533 09/30/2021 HIV Testing Locations Hours Monday Hours Tuesday 11:00 AM - 7:00 PM 9:00 AM - 5:00 PM 8:00 AM - 8:00 PM 8:00 AM - 8:00 PM CLOSED CLOSED 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 2 of 533 09/30/2021 HIV Testing Locations Hours Wednesday Hours Thursday 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM 8:30 AM - 5:00 PM 8:00 AM - 8:00 PM 8:30 AM - 5:00 PM 8:30 AM - 5:00 PM 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 3 of 533 09/30/2021 HIV Testing Locations Hours Friday -

August 9, 2021 RELIEF RESOURCES and SUPPORTIVE
September 24, 2021 RELIEF RESOURCES AND SUPPORTIVE INFORMATION1 • Health & Wellness • Housing • Workplace Support • Human Rights • Education • Bilingual and Culturally Competent Material • Beware of Scams • Volunteering • Utilities • Legal Assistance • City and State Services • Burial • Transportation • New York Forward/Reopening Guidance • Events HEALTH & WELLNESS • Financial Assistance and Coaching o COVID-19 Recovery Center : The City Comptroller has launched an online, multilingual, comprehensive guide to help New Yorkers navigate the many federal, state and city relief programs that you may qualify for. Whether you’re a tenant, homeowner, parent, small business owner, or excluded worker, this online guide offers information about a range of services and financial support. o New York City will be extending free tax assistance to help families claim their new federal child tax credit. As an investment in the long-term recovery from the pandemic, the federal American Rescue Plan made changes to the Child Tax Credit so families get half of the fully refundable credit—worth up to $3,600 per child—as monthly payments in 2021 and the other half as a part of their refund in 1 Compiled from multiple public sources 2022. Most families will automatically receive the advance payments, but 250,000+ New York City families with more than 400,000 children need to sign up with the IRS to receive the Credit. The Advance Child Tax Credits payments began on July 15, 2021 and most New Yorkers will receive their payments automatically. However, New Yorkers who have not submitted information to the IRS need to either file their taxes or enter their information with the IRS’ Child Tax Credit Non-Filer Sign-Up Tool For more information about the Advance Child Tax Credit including access to Multilingual flyer and poster—and NYC Free Tax Prep, visit nyc.gov/TaxPrep or call 311. -

HAVAA Invitation
RD AWA XILIAN AN EMENT L AU D VOLUNTEER ACHIEV ITA SP HO D AR AW T EN EM V IE H C A R E E T N U The United Hospital Fund is dedicated to creating the health care system all of us want for ourselves, our families, and our neighbors. Please consider honoring one of today’s extraordinary volunteers or auxilians, and supporting the work of the Fund, by becoming a Patron or Sponsor. This unique awards program brings public attention to the invaluable contributions of our honorees, and the other 50,000 committed volunteers in our city, who make such an important difference to patients and their families and extend the ability of New York’s hospitals to provide the best care possible. Patrons and Sponsors will be recognized in the event’s Program and all gifts will be gratefully acknowledged. Please use the enclosed reply card to indicate your level of support. Please join us for tea at the Waldorf as the United Hospital Fund honors the 2009 recipients of the # HOSPITAL AUXILIAN and VOLUNTEER ACHIEVE#MENT AWARD Friday, March 6, 2009 1:00 p.m. to 3:00 p.m The Grand Ballroom of The Waldorf-Astoria Park Avenue at 50th Street, New York City Special Guest Sade Baderinwa Co-anchor,WABC-TV Eyewitness News at 5:00 RSVP by February 10, 2009 on the enclosed card Generously underwritten by TD Bank United Hospital Fund The United Hospital Fund is a health services research and J. Barclay Collins II philanthropic organization whose Chairman mission is to shape positive change James R. -

A Guide to Innovative, Quality Long Term Care Options in New York
A Guide to Innovative, Quality e Long Term Care c Options in New York r u o S e r 555 WEST 57TH STREET a NEW YORK, NY 10019 212.258.5330 P 212.258.5331 F WWW.CCLC.ORG C CareSource A Guide to Innovative, Quality Long Term Care Options in New York CCLC Staff Contacts: About CCLC The Continuing Care Leadership Coalition (CCLC) is a membership Scott C. Amrhein 212.506.5409 and advocacy organization representing more than 100 of the President nation’s most innovative and comprehensive not-for-profit and public long term care organizations in the New York metropolitan Roxanne G.Tena-Nelson 212.506.5412 area and beyond. CCLC’s establishment in 2003 as an affiliate of the Vice President Greater New York Hospital Association (GNYHA) highlights the growing importance of continuing care services in today’s health Desmond D’Sa 212.506.5458 care marketplace. Associate Vice President of Finance and Reimbursement CCLC’s purpose is to shape, through advocacy, research, and education, Kelly L. Donohue an environment that supports the delivery of, and access to, contin- Director of Communications 212.506.5424 uing care services of the highest quality and to provide State and national leadership in advancing effective continuing care policies Jenifer H. Fergusson and practices through the collective experience, vision, and effort Events Planner 212.506.5426 of our members. LaSheandra Hunter 212.506.5429 The members of CCLC provide mission-driven services across the Operations Assistant continuum of care to people of all ages throughout the New York metropolitan area and beyond.