Blekinge Institute of Technology Doctoral Dissertation Series No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Et Eksempel På Havplanlægning På Tværs Af Kommunegrænser I Blekinge
Inter-municipal MSP Case study Blekinge Seaplanspace seminar Aalborg University, 20 February 2020 Henrik Nilsson –World Maritme University The role of municipalities in MSP u 82 coastal municipalities in Sweden u Municipalities responsible for spatial planning on land and sea areas within their boundaries u Municipal border extends to outer limit of territorial sea. u Comprehensive plans – guiding plans Marine Spatial Plan Blekinge Inter-municipal plan between 4 municipalities: • Sölvesborg • Karlshamn • Ronneby • Karlskrona • Starts at 300m from baseline – outer border of TS • Guiding plan • Adopted in autumn 2019 Development process u 2014 - Initiative taken by County Administrative Board and Blekinge Archipelago Biosphere Reserve u 2015 – Municipal inventory of data and knowledge needed for development of MSP. u 2016/2017 – Funding from Swam to continue inventory and development of plan. u Set-up of organisational structure u Working group with representatives from each municipality (planners) u Steering group at each municipality (planners, environmental strategist, port representatives etc) Stakeholder consultations 2017 u Thematic consultations: 1. Fisheries,aquaculture,energy 2. Shipping,infrastructure and extraction of natural resources 3. Nature protection, leisure and tourism 4. Defense, climate, cultural heritage Interest matrix Compatible use Limited risk of conflct Risk of conflict Clear risk of conflict Interactive GiS map • Fisheries • Aquaculture • Shipping • Defense • Nature • Energy • Infrastructure • Exploitation of natural resources • Recreation • Culture Key benefits of cooperation in inter- municipal MSP planning u Shared knowledge and competences u Ecological considerations are done from a more holistic perspective u Interest conflicts and subsequent solutions are easier to identify u Common knowledge gaps are identified as well as needs for additional competences Thank you!. -

Blekinge Bohuslän Dalarna Tema: Sveriges Landskap FACIT
Tema: Sveriges landskap FACIT: Landskapsutmaningen Blekinge 1. Kungsljus, ek och ekoxe 2. Mörrumsån 3. Sveriges trädgård 4. Bilar, maskiner, telesystem, kök, badrum samt utrustning för sportfiske 5. Gubben Rosenbom är egentligen en tiggarsparbössa som samlar ihop pengar till fattiga i staden. 6. En skärgård är ett område utanför en kust med många öar, skär och grund. Utmaning 2: -Stirr är det uppväxtstadium av fiskarten lax som föregår smoltstadiet, då den vandrar ut i havet. Den känns igen på en rad mörka tvärband längs sidan. -Smolt är ett uppväxtstadium hos lax, som kommer mellan stirr och blanklax. Smolt är silver- färgad med svarta prickar och har ändrat sina fysiologiska processer för att klara vandringen från rinnande vatten ut i havet. -Blanklax är det ljust färgade havsstadiet av lax. -Grilse är lax som återvänder till sötvatten efter mindre än två års vistelse i havet. -Vraklax är en utlekt individ av fiskarten lax. Bohuslän 1. Knubbsäl och vildkaprifol 2. Tjörn och Orust 3. Bronsåldern 4. Granit är mellan en halv miljard till cirka två miljarder gammalt. 5. Den använder klorna till att krossa skalet på snäckor och musslor. 6. Tran är en olja från kokning av bland annat fisk och säl som används vid bearbetning av läder. Förr användes den även som bränsle i oljelampor. Dalarna 1. Berguv och ängsklocka 2. Siljan 3. Nusnäs 4. Det var bättre bete för husdjuren vid fäbodarna på sommaren. 5. Skogsindustri (papper, pappersmassa, trävaror) järn- och stålindustri för tillverkning av plåt, verkstadsindustri 6. Transtrandsfjällen facit_utmaningen_sveriges landskap Tema: Sveriges landskap FACIT: Landskapsutmaningen Dalsland 1. Korp och förgätmigej 2. -
Småland‑Blekinge 2019 Monitoring Progress and Special Focus on Migrant Integration
OECD Territorial Reviews SMÅLAND-BLEKINGE OECD Territorial Reviews Reviews Territorial OECD 2019 MONITORING PROGRESS AND SPECIAL FOCUS ON MIGRANT INTEGRATION SMÅLAND-BLEKINGE 2019 MONITORING PROGRESS AND PROGRESS MONITORING SPECIAL FOCUS ON FOCUS SPECIAL MIGRANT INTEGRATION MIGRANT OECD Territorial Reviews: Småland‑Blekinge 2019 MONITORING PROGRESS AND SPECIAL FOCUS ON MIGRANT INTEGRATION This document, as well as any data and any map included herein, are without prejudice to the status of or sovereignty over any territory, to the delimitation of international frontiers and boundaries and to the name of any territory, city or area. Please cite this publication as: OECD (2019), OECD Territorial Reviews: Småland-Blekinge 2019: Monitoring Progress and Special Focus on Migrant Integration, OECD Territorial Reviews, OECD Publishing, Paris. https://doi.org/10.1787/9789264311640-en ISBN 978-92-64-31163-3 (print) ISBN 978-92-64-31164-0 (pdf) Series: OECD Territorial Reviews ISSN 1990-0767 (print) ISSN 1990-0759 (online) The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law. Photo credits: Cover © Gabriella Agnér Corrigenda to OECD publications may be found on line at: www.oecd.org/about/publishing/corrigenda.htm. © OECD 2019 You can copy, download or print OECD content for your own use, and you can include excerpts from OECD publications, databases and multimedia products in your own documents, presentations, blogs, websites and teaching materials, provided that suitable acknowledgement of OECD as source and copyright owner is given. -

Develop Sweden! the EU Structural and Investment Funds in Sweden 2014–2020
2014 –2020 Develop Sweden! The EU Structural and Investment Funds in Sweden 2014–2020 Swedish Board The Swedish of Agriculture ESF Council © Swedish Agency for Economic and Regional Growth Production: Ordförrådet Stockholm, mars 2016 Info 0617 ISBN 978-91-87903-40-3 DEVELOP SWEDEN Develop Sweden! The European Structural and Investment Funds (ESIF) provide opportunities for major investments to develop regions, individu- als and enterprises throughout Sweden. A total of SEK 67 billion (including public and/or private co-financ- ing) is to be invested in the years 2014–2020. In order for this fund- ing to have the greatest possible benefit, Sweden has agreed with the European Commission (EC) on certain priorities: • Enhance competitiveness, knowledge and innovation • Sustainable and efficient utilisation of resources for sustainable growth • Increase employment, enhance employability and improve access to the labour market In the years 2014–2020, Sweden will be participating in 27 pro- grammes financed by one of four ESIF. This brochure provides an overview of the programmes under the ESIF that concern Sweden, and the programmes in which Swedish organisations, government agencies and enterprises can participate. For those requiring more in-depth information, for example in order to seek funding, it includes references to the responsible government agencies and organisations. This brochure has been produced collaboratively by the Managing Authorities of the ESIF in Sweden. For more information about these four funds and 27 programmes, visit www.eufonder.se 1 Contents EU Structural and Investment Funds in Sweden 2014–2020 .................................................. 3 European Social Fund .............................................................................................................. 6 European Regional Development Fund ................................................................................... 8 Upper-North Sweden ............................................................................................................. -
Nils Holgerssons Underbara Matresa Blekinge Och Öland
Nils Holgerssons underbara matresa Recept och kuriosa för kockar och matgäster Blekinge och Öland ”Jag tycker det var bättre förr. Även det som var sämre var på något sätt bättre” Ölänskt talesätt Inledning Välkommen till ’’Nils Holgerssons underbara matresa’’. Under flera veckor kommer vi tillsammans göra en kulinarisk resa genom flera av Sveriges landskap, där vi bekantar oss med rätter som är typiska för just det landskap vi befinner oss i. Vid varje nytt stopp kommer det ett nytt häfte med intressant information om området och recept. Syftet med dessa häften är att ni som kockar ska få lära er lite mer om våra svenska landskapsrätter. Denna information kan ni sedan sprida vidare till era matgäster. Vi hoppas att informationen kommer att vara till nytta och att ni blir mer nyfikna på den svenska matkulturhistorian. Vi inleder denna resa med en beskrivning av vad husmanskost är av Margareta Björn. Trevlig resa! Husmanskost Förr var husmanskost en beteckning för den maten man åt i vardagslag. Grundstommen i vardagsmaten var gröt eller välling morgon och kväll. Salt strömming och sill hörde också vardagen till, liksom det salta fläsket. Denna stadiga och enformiga grundstomme lättades sedan upp av den fisk som fångades i sjöar och vattendrag och det vilda som kunde jagas. Till söndagen och vid de större helgerna försökte alla, även den fattigaste av husmödrar, servera familjen litet godare mat. Numera har husmanskost blivit beteckning för rätter som vi anser typiskt svenska. Källa: Margareta Björn, med Nils Holgersson på matresa genom Sverige. Det kulinariska Blekinge 3 000 år gamla hällristningar visar att redan då fanns det människor som upptäckt att det är värt att besöka Blekinge(1). -

Baltic Towns030306
The State and the Integration of the Towns of the Provinces of the Swedish Baltic Empire The Purpose of the Paper1 between 1561 and 1660, Sweden expanded Dalong the coasts of the Baltic Sea and throughout Scandinavia. Sweden became the dominant power in the Baltics and northern Europe, a position it would maintain until the early eighteenth century. At the same time, Swedish society was experiencing a profound transformation. Sweden developed into a typical European early modern power-state with a bureaucracy, a powerful mili- tary organization, and a peasantry bending under taxes and conscription. The kingdom of Sweden also changed from a self-contained country to an important member of the European economy. During this period the Swedish urban system developed as well. From being one of the least urbanized European countries with hardly more than 40 towns and an urbanization level of three to four per cent, Sweden doubled the number of towns and increased the urbanization level to almost ten per cent. The towns were also forced by the state into a staple-town system with differing roles in fo- reign and domestic trade, and the administrative and governing systems of the towns were reformed according to royal initiatives. In the conquered provinces a number of other towns now came under Swe- dish rule. These towns were treated in different ways by the state, as were the pro- vinces as a whole. While the former Danish and Norwegian towns were complete- ly incorporated into the Swedish nation, the German and most of the east Baltic towns were not. -

Småland–Blekinge SAMMANFATTNING
SAMMANFATTNING OECD Territorial Reviews Småland–Blekinge SAMMANFATTNING UTVÄRDERING AV TERRITORIAL REVIEW SAMT STUDIE AV INTEGRATIONSUTMANINGAR 3 Om OECD OECD är ett unikt forum för utbyte av idéer och erfarenheter samt analyser av aktuella frågor inom ett stort antal politikområden. En viktig del i detta är att hjälpa medlemsländerna att lära av varandra, diskutera gemensamma problem för att på så sätt få underlag för nationella beslut. Viktiga områden är ekonomisk politik, handelspolitik, utbildningspolitik, arbetsmarknadspolitik, antikorruption, skatter, utvecklingssamarbete, sociala frågor och internationella investeringar. Om CFE CFE, centrum för entreprenörskap, SME, regioner och städer hjälper lokala, regionala och nationella myndigheter att frigöra entreprenörers och små och medelstora företags potential, att främja inkluderande och hållbara regioner och städer, att stimulera skapande av lokala arbetstillfällen och att utveckla hållbara strategier för turism. Om detta dokument I detta dokument sammanfattas huvudresultaten från OECD:s rapport (2019), OECD Territorial Reviews: Småland–Blekinge: Monitoring progress and special focus on migrant integration, OECD Publishing, Paris. Hela publikationen finns att på https://www.oecd- ilibrary.org. Ansvarig utgivare för publikationen är OECD:s generalsekretariat. Åsikter och argument som uttrycks och används i publikationen speglar inte nödvändigtvis officiella ståndpunkter hos organisationen eller medlemsländernas regeringar. Bilder: © Mostphotos.com och Region Kalmar län Ytterligare information: -
Kingdom of Sweden
Johan Maltesson A Visitor´s Factbook on the KINGDOM OF SWEDEN © Johan Maltesson Johan Maltesson A Visitor’s Factbook to the Kingdom of Sweden Helsingborg, Sweden 2017 Preface This little publication is a condensed facts guide to Sweden, foremost intended for visitors to Sweden, as well as for persons who are merely interested in learning more about this fascinating, multifacetted and sadly all too unknown country. This book’s main focus is thus on things that might interest a visitor. Included are: Basic facts about Sweden Society and politics Culture, sports and religion Languages Science and education Media Transportation Nature and geography, including an extensive taxonomic list of Swedish terrestrial vertebrate animals An overview of Sweden’s history Lists of Swedish monarchs, prime ministers and persons of interest The most common Swedish given names and surnames A small dictionary of common words and phrases, including a small pronounciation guide Brief individual overviews of all of the 21 administrative counties of Sweden … and more... Wishing You a pleasant journey! Some notes... National and county population numbers are as of December 31 2016. Political parties and government are as of April 2017. New elections are to be held in September 2018. City population number are as of December 31 2015, and denotes contiguous urban areas – without regard to administra- tive division. Sports teams listed are those participating in the highest league of their respective sport – for soccer as of the 2017 season and for ice hockey and handball as of the 2016-2017 season. The ”most common names” listed are as of December 31 2016. -

Samverkansplan För Biosfärområde Blekinge Arkipelag
Samverkansplan för Blekinge Arkipelag Samverkansplan för biosfärområde Blekinge Arkipelag - 1 - Samverkansplan för Blekinge Arkipelag Fotografer Erika Axelsson 57 Bergslagsbild 4, 21v, 47 Robert Ekholm 24, 39v, 60, 62 Herbert Eriksen 37 Fösvarsmakten 55 Roland Gustavsson 66 Ronny Gustavsson 28 Torbjörn Frennesson 21h Britt-Marie Havby 34 Jenny Hertzman 15, 31, 32v, 40, 41, 61 Håll Sverige Rent 32h Anette Johansson 13, 67 Titel: Samverkansplan för biosfärområde Blekinge Arkipelag Joakim Johansson 43 Anja Johnsson 51 Författare: Lena Axelsson, Kerstin Carlson, Hans-Erik Fröberg, Håkan Jönsson 16 Kenneth Gyllensting, Jenny Hertzman, Birgith Juel, Karlshamns kommun 3 Eva-Marie Lundberg, Sven-Olof Petersson, Leifh Stenholm, Mats Kockum 22h, 35 Nina Södergren, Anders Thurén Ulf Lundgren 17, 22v, 36, 39h Annika Lydänge 63 Projektledare: Jenny Hertzman Sven-Erik Löfgren 25 Nils-Gustaf Nydolf 42v, 50 Grafi sk form: Annika Spåhl Jens Näslund 10 Ronneby kommun 29 Utgiven av: Länsstyrelsen Blekinge län 2011 Anders Thurén 14, 65, 118 Petra Torebrink 19, 26 Hemsida: www.blekingearkipelag.se Cecilia Serrby 18, 27, 64 Beställningsadress: Länsstyrelsen Blekinge län, 371 86 Karlskrona Martin Stålhammar 10 Nina Södergren 14, 20 Omslagsfoto: Mats Kockum Mathias Wijk 42h - 2 - Samverkansplan för Blekinge Arkipelag Vision Blekinge Arkipelag – ett hav av möjligheter! Blekinge Arkipelag står för en levande kust och skärgård där utvecklingen sker i harmoni mellan företagande och ekologi. Grunden är lokalt engagemang och omtanke om kommande generationers framtid. - 3 - Samverkansplan för Blekinge Arkipelag Blekinge Arkipelag – Samverkansplanen är ett viktigt redskap i detta arbete eftersom den värnar om områdets kvaliteter och bejakar en hållbar utveckling ett hav av möjligheter! som sker med stor hänsyn. -

Sweden Facing Climate Change – Threats and Opportunities
Sweden facing climate change – threats and opportunities Final report from the Swedish Commission on Climate and Vulnerability Stockholm 2007 Swedish Government Official Reports SOU 2007:60 This report is on sale in Stockholm at Fritzes Bookshop. Address: Fritzes, Customer Service, SE-106 47 STOCKHOLM Sweden Fax: 08 690 91 91 (national) +46 8 690 91 91 (international) Tel: 08 690 91 90 (national) +46 8 690 91 91 E-mail: [email protected] Internet: www.fritzes.se Printed by Edita Sverige AB Stockholm 2007 ISBN 978-91-38-22850-0 ISSN 0375-250X Preface The Commission on Climate and Vulnerability was appointed by the Swedish Government in June 2005 to assess regional and local impacts of global climate change on the Swedish society including costs. Bengt Holgersson Governor of the County Administrative Board in the region of Skåne was appointed head of the Com- mission. This report will be subject to a public review and will serve as one of the inputs to a forthcoming climate bill in 2008. The author have the sole responsibility for the content of the report and as such it can not be taken as the view of the Swedish Government. This report was originally produced in Swedish. It has been translated into English and the English version corresponds with the Swedish one. However, one chapter with specific proposals for changes in Swedish legislation was not translated, nor were the appendices translated. Hence, these are only available in the Swedish original version. Contents 1 Summary................................................................... 11 2 The assignment and background.................................. 35 2.1 The assignment, scope and approach..................................... -

Pressmeddelande
Pressmeddelande december 2015 Inskrivna arbetslösa 16-64 år i procent av registerbaserad arbetskraft december 2015 Uppsala Stockholm Halland Jönköping Västerbotten Västra Götaland Dalarna Norrbotten Jämtland Gotland Kalmar Örebro Kronoberg Värmland Östergötland Västernorrland Västmanland Skåne Södermanland Blekinge Gävleborg 0 1 2 3 4 5 6 7 8 9 10 11 12 Procent Källa: Arbetsförmedlingen, SCB Förändring av inskrivna arbetslösa december 2015 jämfört med motsvarande period 2014 Gotland Västra Götaland Jämtland Östergötland Västerbotten Värmland Norrbotten Stockholm Jönköping Örebro Kalmar Västernorrland Skåne Kronoberg Halland Gävleborg Blekinge Uppsala Västmanland Södermanland Dalarna -0,9 -0,8 -0,7 -0,6 -0,5 -0,4 -0,3 -0,2 -0,1 0,0 0,1 0,2 Procentenhet Källa: Arbetsförmedlingen Inskrivna öppet arbetslösa på Arbetsförmedlingen i procent av registerbaserad arbetskraft december 2015 Uppsala Jönköping Västerbotten Jämtland Halland Gotland Stockholm Norrbotten Västra Götaland Kalmar Kronoberg Östergötland Örebro Värmland Dalarna Gävleborg Västernorrland Västmanland Blekinge Södermanland Skåne 0 1 2 3 4 5 6 Procent Källa: Arbetsförmedlingen, SCB Förändring av inskrivna öppet arbetslösa december 2015 jämfört med motsvarande period 2014 Gotland Gävleborg Västra Götaland Kronoberg Jämtland Jönköping Västerbotten Kalmar Norrbotten Östergötland Stockholm Örebro Skåne Värmland Västmanland Uppsala Västernorrland Södermanland Blekinge Halland Dalarna -0,4 -0,3 -0,2 -0,1 0,0 0,1 0,2 0,3 0,4 Procentenhet Källa: Arbetsförmedlingen Inskrivna i program med -
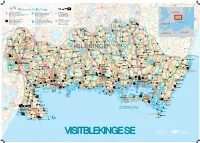
Visit Blekinge Karta
Påryd 126 Rävemåla 28 Törn Flaken Welcome to Blekinge 120 ARK56 Nav - Ledknutpunkt ARK56 Kajakled Blekingeleden Häradsbäck 120 Markerad vandringsled Sandsjön SWEDEN ARK56 Hub - Trail intersection120 Rekommenderad led för paddling Urshult Tingsryd Kvesen Vissefjärda ARK56 Knotenpunkt diverser Wege und Routen Recommended trail for kayaking Waymarked hiking trail ARK56 Węzeł - punkt zbiegu szlaków Empfohlener Paddel - Pfad Markierter Wanderweg 122 www.ark56.se Zalecana trasa kajakowa Oznakowany szlak pieszy Tiken 27 Dångebo Campingplatser - Camping Sydost RammsjönSkärgårdstrafik finns i området Sydostleden Arasjön Campsites - Camping Sydost Passenger boat services available Rekommenderad cykelled Stora Kinnen Halltorp Campingplatz - Camping Sydost Skärgårdstrafik - Passagierschiffsverkehr Recommended cycle trail Hensjön Ulvsmåla Älmtamåla Kemping - Camping Sydost Obszar publicznego transportu wodnego Empfohlener Radweg Baltic Sea www.campingsydost.se www.skargardstrafiken.com Zalecany szlak rowerowy 119 Ryd Djuramåla Saleboda DENMARKGullabo Buskahult Skumpamåla Spetsamåla Söderåkra Lyckebyån Siggamåla Åbyholm Farabol 119 Eringsboda Alvarsmåla Tjurkhult Göljahult Kolshult Falsehult POLAND130 126 GERMANY Mien Öljehult Husgöl Torsåsån Värmanshult Hjorthålan Holmsjö Fridafors R o Leryd Sillhöv- Kåraboda Björkebråten n Ledja n Boasjö 27 e dingen Torsås b y Skälmershult Björkefall å n Ärkilsmåla Dalanshult Hallabro Brännare- Belganet Hjortseryd Långsjöryd Klåvben St.Skälen Gnetteryd bygden Väghult Ebbamåla Alljungen Brunsmo Bruk St.Alljungen Mörrumsån