The Region of the Wrist and Hand
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Orthopaedics Instructions: To best navigate the list, first download this PDF file to your computer. Then navigate the document using the bookmarks feature in the left column. The bookmarks expand and collapse. Finally, ensure that you look at the top of each category and work down to review notes or specific instructions. Bookmarks: Bookmarks: notes or specific with expandable instructions and collapsible topics As you start using the codes, it is recommended that you also check in Index and Tabular lists to ensure there is not a code with more specificity or a different code that may be more appropriate for your patient. Copyright APTA 2016, ALL RIGHTS RESERVED. Last Updated: 09/14/16 Contact: [email protected] Orthopaedics Disorder by site: Ankle Achilles tendinopathy ** Achilles tendinopathy is not listed in ICD10 M76.6 Achilles tendinitis Achilles bursitis M76.61 Achilles tendinitis, right leg M76.62 Achilles tendinitis, left leg ** Tendinosis is not listed in ICD10 M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, excluding foot M76.892 Other specified enthesopathies of left lower limb, excluding foot Posterior tibialis dysfunction **Posterior Tibial Tendon Dysfunction (PTTD) is not listed in ICD10 M76.82 Posterior tibial tendinitis M76.821 Posterior tibial tendinitis, right leg M76.822 Posterior tibial tendinitis, left leg M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, -

Four Unusual Cases of Congenital Forelimb Malformations in Dogs
animals Article Four Unusual Cases of Congenital Forelimb Malformations in Dogs Simona Di Pietro 1 , Giuseppe Santi Rapisarda 2, Luca Cicero 3,* , Vito Angileri 4, Simona Morabito 5, Giovanni Cassata 3 and Francesco Macrì 1 1 Department of Veterinary Sciences, University of Messina, Viale Palatucci, 98168 Messina, Italy; [email protected] (S.D.P.); [email protected] (F.M.) 2 Department of Veterinary Prevention, Provincial Health Authority of Catania, 95030 Gravina di Catania, Italy; [email protected] 3 Institute Zooprofilattico Sperimentale of Sicily, Via G. Marinuzzi, 3, 90129 Palermo, Italy; [email protected] 4 Veterinary Practitioner, 91025 Marsala, Italy; [email protected] 5 Ospedale Veterinario I Portoni Rossi, Via Roma, 57/a, 40069 Zola Predosa (BO), Italy; [email protected] * Correspondence: [email protected] Simple Summary: Congenital limb defects are sporadically encountered in dogs during normal clinical practice. Literature concerning their diagnosis and management in canine species is poor. Sometimes, the diagnosis and description of congenital limb abnormalities are complicated by the concurrent presence of different malformations in the same limb and the lack of widely accepted classification schemes. In order to improve the knowledge about congenital limb anomalies in dogs, this report describes the clinical and radiographic findings in four dogs affected by unusual congenital forelimb defects, underlying also the importance of reviewing current terminology. Citation: Di Pietro, S.; Rapisarda, G.S.; Cicero, L.; Angileri, V.; Morabito, Abstract: Four dogs were presented with thoracic limb deformity. After clinical and radiographic S.; Cassata, G.; Macrì, F. Four Unusual examinations, a diagnosis of congenital malformations was performed for each of them. -

Fractures of the Neck of the Fifth Metacarpal Bone. Medium-Term Results in 28 Cases Treated by Percutaneous Transverse Pinning I
Injury, Int. J. Care Injured 43 (2012) 242–245 Contents lists available at SciVerse ScienceDirect Injury jo urnal homepage: www.elsevier.com/locate/injury Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning V. Potenza *, R. Caterini, F. De Maio, S. Bisicchia, P. Farsetti Department of Orthopaedic Surgery, University of Rome ‘Tor Vergata’, Rome, Italy A R T I C L E I N F O A B S T R A C T Article history: The purpose of this study was to report the medium-term results in 28 patients affected by closed Accepted 27 October 2011 displaced fractures of the neck of the fifth metacarpal bone (boxer’s fracture) with an associated severe swelling of the hand, who were treated with percutaneous transverse K-wire pinning, to verify the Keywords: effectiveness of this surgical treatment. We opted for this treatment in all cases in which malrotation of Boxer’s fracture the fifth finger and volar angulation of the metacarpal head greater than 308 were associated with a Transverse pinning severe swelling of the hand. All the patients were reviewed clinically and radiologically at an average of Metacarpal neck fracture 25 months after surgery. At the final follow-up, no patient reported residual pain. All patients had full extension of the fifth finger, except two in whom we observed a limitation of the extension of the fifth metacarpophalangeal (MP) joint of about 108, without significant impairment of hand function. All patients had at least 908 flexion of the fifth MP joint and full range of motion of the interphalangeal (IP) joints. -

The Ossification of the Metacarpal and Phalangeal Bones in Human Foetuses
Folia Morphol. Vol. 63, No. 3, pp. 329–332 Copyright © 2004 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl The ossification of the metacarpal and phalangeal bones in human foetuses Florian Czerwiński1, Ewa Tomasik1, Małgorzata Tomasik2, Aldona Mahaczek-Kordowska1 1Department of Anatomy, Pomeranian Academy of Medicine, Szczecin, Poland 2Department of General Dentistry, Pomeranian Academy of Medicine, Szczecin, Poland [Received 4 November 2002; Revised 17 February 2004; Accepted 17 February 2004] An evaluation was made of the ossification level of the metacarpal and pha- langeal bones in human foetuses of both sexes from the 4th to the 9th month of gestation. Our results indicate that ossification of phalangeal bones 1 to 5 al- ways started at the distal end of the phalanx and endochondral ossification prevailed in the proximal phalanx of the thumb. Key words: human foetus, metacarpal bones, phalangeal bones, ossification INTRODUCTION Most human skeletal bones are ossified on a car- tilaginous base [5, 14]. This is a complex process pro- gressing dynamically in time and ossification consti- tutes the final phase of this complex process [3]. Thorough observation of the ossification of the foe- tal skeleton is made possible by means of the radio- logical method and evaluation of histological speci- mens [9]. This study presents the ossification of the metacarpal and phalangeal bones in human foetus- es at different stages of gestation. MATERIAL AND METHOD Eighty-six hands were examined taken from hu- man foetuses of both sexes aged from 4 to 9 months of gestation. -

Functional Anatomy of the Equine Musculoskeletal System
1 CHAPTER Functional Anatomy of the Equine Musculoskeletal System ANNA DEE FAILS ANATOMIC NOMENCLATURE AND USAGE Foot Veterinary medical anatomists have been using the The foot consists of the hoof and all it encloses: the Nomina Anatomica Veterinaria, created by the Inter connective tissue corium (dermis), digital cushion, distal national Committee on Veterinary Gross Anatomical phalanx (coffin bone), most of the cartilages of the distal Nomenclature since 1968 to standardize the names of phalanx, distal interphalangeal (coffin) joint, distal part anatomical structures.46 This chapter endeavors to use the of the middle phalanx (short pastern bone), distal sesa most current, correct terms as outlined in that publication. moid (navicular) bone, podotrochlear bursa (navicular Nonetheless, equine practitioners need to be equally fluent bursa), several ligaments, tendons of insertion of the in older terminology, which is likely to be in wide usage common digital extensor and deep digital flexor mus among horse owners and equine professionals. This chap cles, blood vessels, and nerves. Skin between the heels is ter will provide useful and common synonyms for many also part of the foot. structures, along with their more technically correct terms. Figure 1.1 provides the directional terms for veteri HOOF WALL, SOLE, AND FROG nary anatomy that will be used in this chapter. With the exception of the ocular and oral cavity structures, the The hoof is continuous with the epidermis at the cor terms anterior, posterior, superior, and inferior are not onet, and the underlying corium of the hoof is likewise applicable to quadrupeds. continuous with the dermis of the skin. -

Metacarpal Fractures: Practical Methods for Measurement of Shortening, Angulation, and Malrotation
J Orthop Spine Trauma. 2020 March; 6(1): 9-13. DOI: http://dx.doi.org/10.18502/jost.v6i1.4535 Educational Corner Metacarpal Fractures: Practical Methods for Measurement of Shortening, Angulation, and Malrotation Rohollah Khajeh 1, Behzad Enayati1, Farzad Vosughi2, Seyed Mohammad Javad Mortazavi 3,* 1 Fellowship of Hand Surgery, Joint Reconstruction Research Center, Tehran University of Medical Sciences, Tehran, Iran 2 Resident, Department of Orthopedics, Joint Reconstruction Research Center, Tehran University of Medical Sciences, Tehran, Iran 3 Professor, Department of Orthopedic Surgery, Joint Reconstruction Research Center, Tehran University of Medical Sciences, Tehran, Iran *Corresponding author: Seyed Mohammad Javad Mortazavi; Department of Orthopedic Surgery, Joint Reconstruction Research Center, Tehran University of Medical Sciences, Tehran, Iran. Tel: +98-2161192767, Email: [email protected] Received: 09 October 2019; Revised: 15 December 2019; Accepted: 17 January 2020 Keywords: Metacarpus; Fractures, Bone; Hand Deformities, Acquired Citation: Khajeh R, Enayati B, Vosughi F, Mortazavi SMJ. Metacarpal Fractures: Practical Methods for Measurement of Shortening, Angulation, and Malrotation. J Orthop Spine Trauma 2020; 6(1): 9-13. Background different metacarpal fractures. Articular fractures involving less than 20% of the joint Phalangeal, distal radius, and metacarpal fractures are surface and nondisplaced or minimally displaced shaft the most frequent upper limb fractures, respectively (1). fractures, without significant angulation, malrotation, or The incidence of metacarpal fractures in the United States shortening are treated with immobilization in the of America (USA) is 13.6 among every 100000 population intrinsic plus position (6). Bony apposition of at least 50% annually (2). Metacarpal fractures compose 30-40 percent and maximal bone shortening of 5 mm is acceptable. -

Developing Learning Models to Teach Equine Anatomy and Biomechanics
The University of Maine DigitalCommons@UMaine Honors College Spring 5-2017 Developing Learning Models to Teach Equine Anatomy and Biomechanics Zandalee E. Toothaker University of Maine Follow this and additional works at: https://digitalcommons.library.umaine.edu/honors Part of the Animal Sciences Commons, and the Veterinary Anatomy Commons Recommended Citation Toothaker, Zandalee E., "Developing Learning Models to Teach Equine Anatomy and Biomechanics" (2017). Honors College. 453. https://digitalcommons.library.umaine.edu/honors/453 This Honors Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Honors College by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. DEVELOPING LEARNING MODELS TO TEACH EQUINE ANATOMY AND BIOMECHANICS By Zandalee E. Toothaker A Thesis Submitted in Partial Fulfillment of the Requirements for a Degree with Honors (Animal and Veterinary Science) The Honors College University of Maine May 2017 Advisory Committee: Dr. Robert C. Causey, Associate Professor of Animal and Veterinary Sciences, Advisor Dr. David Gross, Adjunct Associate Professor in Honors (English) Dr. Sarah Harlan-Haughey, Assistant Professor of English and Honors Dr. Rita L. Seger, Researcher of Animal and Veterinary Sciences Dr. James Weber, Associate Professor and Animal and Veterinary Sciences © 2017 Zandalee Toothaker All Rights Reserved ABSTRACT Animal owners and professionals benefit from an understanding of an animal’s anatomy and biomechanics. This is especially true of the horse. A better understanding of the horse’s anatomy and weight bearing capabilities will allow people to treat and prevent injuries in equine athletes and work horses. -
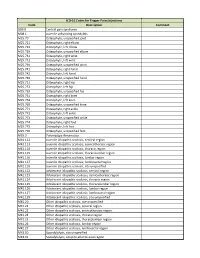
ICD-10 Codes for Trigger Point Injections
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic -

Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without
Original Article / Orijinal Araflt›rma 15 Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without Thenar Atrophy Tenar Atrofisi Olmayan Karpal Tünel Sendromlu Hastalarda Metakarpal Kemik Yo¤unlu¤unun De¤erlendirilmesi Serpil Savafl, Berna Okudan1, Hasan Rifat Koyuncuo¤lu2, Hakan Çelik, Tamer Karaaslan3, Mustafa Y›ld›z 4 Süleyman Demirel Üniversitesi T›p Fakültesi Fiziksel T›p ve Rehabilitasyon, 2Nöroloji, 3Beyin Cerrahisi ve 4Nükleer T›p Anabilim Dal›, Isparta, Türkiye, 1Yeditepe Üniversitesi T›p Fakültesi Nükleer T›p Anabilim Dal›, ‹stanbul, Türkiye Abstract Özet Objective: Bone loss due to thenar atrophy was reported in the me- Amaç: Premenopozal karpal tünel sendromlu (KTS) kad›nlarda te- tacarpal bones in premenopausal patients with carpal tunnel nar atrofiye ba¤l› olarak metakarpal kemik yo¤unlu¤u kayb› oldu- syndrome (CTS). The present study was designed to assess bone ¤u bilinmektedir. Bu çal›flman›n amac›, tenar atrofisi olmayan KTS’li density in the metacarpal bones in patients with CTS without hastalarda metakarpal kemik mineral yo¤unlu¤unu de¤erlendir- thenar atrophy and to correlate the metacarpal bone density with mek, metakarpal kemik yo¤unlu¤u ile elektrofizyolojik bulgular›, el the electrophysiological findings, hand strength and Boston gücü ve Boston Anketi aras›ndaki iliflkiyi belirlemektir. Questionnaire (BQ). Hastalar ve Yöntem: Çal›flmaya tenar atrofisi olmayan 30 KTS’li pre- Patients and Methods: Thirty premenopausal patients with CTS menopozal hasta ile 32 premenopozal kontrol olgu al›nd›. KTS’li without thenar atrophy were enrolled in this study. Thirty-two hastalar›n semptom fliddeti ve fonksiyonel durumlar› Bostan Anke- consecutive premenopausal women were included in the study as ti ile de¤erlendirildi. -
Case Reports Series A, B, C & D Table of Contents
ACTEC X H E • • C S A T S E R REPO Case Reports Series A, B, C & D Table of ConTents Revision Total Joint Series A, Number 1 ..................................................................................................................................................... 3 Use of opteform® to Repair failed Total Knee Prosthesis with osteolysis, Harry Schmaltz, MD Series A, Number 2 ..................................................................................................................................................... 5 Use of opteform® to Repair Acetabular osteolysis Series A, Number 4 ..................................................................................................................................................... 7 large osteolytic Defect Repair Using opteform® Through an Illiac Window, Abbott Kagan, MD Series A, Number 5 ..................................................................................................................................................... 9 Repair of Acetabular fracture and osteolysis with opteform®-Two Year follow-Up, Wayne Moody, MD fACS Series A, Number 6 ................................................................................................................................................... 11 Acetabular Reconstruction with opteform® and Reconstruction Ring, Wayne Moody, MD fACS Series A, Number 7 ................................................................................................................................................... 13 Use of opteform® -

Macroanatomy of the Bones of Thoracic Limb of an Asian Elephant (Elephas Maximus)
Int. J. Morphol., 34(3):909-917, 2016. Macroanatomy of the Bones of Thoracic Limb of an Asian Elephant (Elephas maximus) Macroanatomía de los Huesos del Miembro Torácico de un Elefante Asiático (Elephas maximus) A. S. M. Lutful Ahasan*; Md. Abul Quasem*; Mohammad Lutfur Rahman*; Rubyath Binte Hasan*; A. S. M. Golam Kibria* & Subrata Kumar Shil* AHASAN, A. M. S. L.; QUASEM, M. A.; RAHMAN, M. L.; HASAN, R. B.; KIBRIA, A. S. M. G. & SHIL, S. K. Macroanatomy of the bones of thoracic limb of an Asian Elephant (Elephas maximus). Int. J. Morphol., 34(3):909-917, 2016. SUMMARY: Bones of forelimb were studied from a prepared skeleton of an adult female Asian elephant (Elephas maximus) in Anatomy Museum of Chittagong Veterinary and Animal Sciences University to understand the morphological form and structure of Asian elephant forelimb. The angle was approximately 123º between caudal border of scapula and caudal border of humerus. The scapula, humerus and bones of the antebrachium (particularly the ulna) were massive bones. The bones of manus were the short and relatively small. The dorsal border of scapula extended from the level of proximal extremity of first rib to the middle of the 6th rib. Ventral angle of scapula articulated with humerus by elongated shaped glenoid cavity (cavitas glenoidalis) of scapula and head of humerus (caput humeri). The major tubercle (tuberculum majus) of humerus was situated laterally to the head, which had smaller cranial part with large caudal part and extended cranially to the head. The crest of minor tubercle (tuberculum minus) was present as the rough line on the mediocaudal surface of humerus that ends in a slight depressed or elevated area, known as teres major tuberosity (tuberositas teres major). -
5Th Metacarpal Fractures Information for Patients
[Type here] Virtual fracture clinic 5th Metacarpal Fractures Information for patients What is a 5th metacarpal fracture? Your hand is made up of five metacarpal bones that connect your fingers and thumb to your wrist. A 5th metacarpal fracture (also known as a boxer’s fracture) is a break in the bone that connects your little finger to your wrist. A break is the same as a fracture. What causes a 5th metacarpal fracture? 5th metacarpal fractures usually occur when there is impact between a hand that is closed in a fist with a firm object, such as the ground or a wall. 5th metacarpal fractures are the most commonly occurring fractures in the hand. What are the signs and symptoms of a 5th metacarpal fracture? If you have fractured your 5th metacarpal bone you may notice that the back of your hand and the little finger are swollen and it will be more difficult to see the knuckles. You may also have some bruising and find it difficult to open and close your fingers. An x-ray should be taken to check the position of the fracture. What are the treatments available for a 5th metacarpal fracture? Most 5th metacarpal fractures are successfully treated without surgery. Even in cases where the alignment of the bone fragments is disrupted, the bones usually heal without any serious long term consequences. The options for non-surgical management are usually to: 1. ‘Buddy strap’ the little finger to the ring finger for two to four weeks and move it as pain allows 2.