Distal Third Metacarpal Bone Palmar Cortical Stress Fractures in Four Thoroughbred Racehorses C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Orthopaedics Instructions: To best navigate the list, first download this PDF file to your computer. Then navigate the document using the bookmarks feature in the left column. The bookmarks expand and collapse. Finally, ensure that you look at the top of each category and work down to review notes or specific instructions. Bookmarks: Bookmarks: notes or specific with expandable instructions and collapsible topics As you start using the codes, it is recommended that you also check in Index and Tabular lists to ensure there is not a code with more specificity or a different code that may be more appropriate for your patient. Copyright APTA 2016, ALL RIGHTS RESERVED. Last Updated: 09/14/16 Contact: [email protected] Orthopaedics Disorder by site: Ankle Achilles tendinopathy ** Achilles tendinopathy is not listed in ICD10 M76.6 Achilles tendinitis Achilles bursitis M76.61 Achilles tendinitis, right leg M76.62 Achilles tendinitis, left leg ** Tendinosis is not listed in ICD10 M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, excluding foot M76.892 Other specified enthesopathies of left lower limb, excluding foot Posterior tibialis dysfunction **Posterior Tibial Tendon Dysfunction (PTTD) is not listed in ICD10 M76.82 Posterior tibial tendinitis M76.821 Posterior tibial tendinitis, right leg M76.822 Posterior tibial tendinitis, left leg M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, -

(Bucked Shins) in the Flat Racing Horse: Prevalence, Diagnosis, Pathogenesis, and Associated Factors
Journal of Dairy, Veterinary & Animal Research Mini Review Open Access A review of dorsal metacarpal disease (bucked shins) in the flat racing horse: prevalence, diagnosis, pathogenesis, and associated factors Abstract Volume 5 Issue 6 - 2017 Dorsal metacarpal disease (DMD) is the most common cause of lostdays to training S Couch,1 BD Nielsen2 and racing in Thoroughbred racehorses. Colloquially termed ‘bucked’ or ‘sore’ shins, 1Royal (Dick) School of Veterinary Studies, University of this initially painful condition commonly occurs in the first season of training and can Edinburgh, United Kingdom raise welfare concerns. Clinical signs include pain with digital palpation and swelling 2Department of Animal Science, Michigan State University, USA on the dorsal, and sometimes dorso-medial, aspect of the third metacarpal (McIII). Periostitis and excessive growth of periosteal bone can be present as a response to Correspondence: Brian D Nielsen, Michigan State University, high strain cyclic fatigue. Whilst DMD can resolve with rest or reduced exercise, it Department of Animal Science, 474 S. Shaw Lane, East Lansing, can leave bone susceptible to future catastrophic fracture at the same site, particularly MI 48824 1225, USA, Tel 517 432 1378, Fax 517 353 1699, saucer fractures of the lamellar bone of the diaphysis. Some trainers continue to work Email [email protected] an animal through DMD, with the view that it will only happen once, but it can re- occur. Additionally, the animal is in discomfort and has a weakened skeletal system. Received: September 13, 2017 | Published: September 25, In vivo studies of the effects of cyclic strain on the skeletal system of Thoroughbreds 2017 are notoriously difficult, due to the many variables involved and in vitro studies cannot mimic true training and racing conditions. -

Clinical Medical Policy
CLINICAL MEDICAL POLICY Noninvasive Electrical Bone Growth Stimulators Policy Name: (osteogenesis stimulators) Policy Number: MP-070-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 12/15/2018 Issue Date: 01/15/2019 Effective Date: 01/15/2019 Annual Approval Date: 10/17/2019 Revision Date: N/A Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 78 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical and DME benefits of the Company’s Medicaid products for medically necessary noninvasive electrical bone growth stimulators as treatment of nonunion long bone fractures or congenital pseudarthrosis. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-070-MD-PA Page 1 of 78 DEFINITIONS Prior Authorization Review Panel - A panel of representatives from within the PA Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Non-invasive (Osteogenic) Electrical Bone Growth Stimulator – A device that uses pulsed- electromagnetic fields, capacitative coupling or combined magnetic fields to generate a weak electric current through the target site. -

Fractures of the Neck of the Fifth Metacarpal Bone. Medium-Term Results in 28 Cases Treated by Percutaneous Transverse Pinning I
Injury, Int. J. Care Injured 43 (2012) 242–245 Contents lists available at SciVerse ScienceDirect Injury jo urnal homepage: www.elsevier.com/locate/injury Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning V. Potenza *, R. Caterini, F. De Maio, S. Bisicchia, P. Farsetti Department of Orthopaedic Surgery, University of Rome ‘Tor Vergata’, Rome, Italy A R T I C L E I N F O A B S T R A C T Article history: The purpose of this study was to report the medium-term results in 28 patients affected by closed Accepted 27 October 2011 displaced fractures of the neck of the fifth metacarpal bone (boxer’s fracture) with an associated severe swelling of the hand, who were treated with percutaneous transverse K-wire pinning, to verify the Keywords: effectiveness of this surgical treatment. We opted for this treatment in all cases in which malrotation of Boxer’s fracture the fifth finger and volar angulation of the metacarpal head greater than 308 were associated with a Transverse pinning severe swelling of the hand. All the patients were reviewed clinically and radiologically at an average of Metacarpal neck fracture 25 months after surgery. At the final follow-up, no patient reported residual pain. All patients had full extension of the fifth finger, except two in whom we observed a limitation of the extension of the fifth metacarpophalangeal (MP) joint of about 108, without significant impairment of hand function. All patients had at least 908 flexion of the fifth MP joint and full range of motion of the interphalangeal (IP) joints. -

Functional Anatomy of the Equine Musculoskeletal System
1 CHAPTER Functional Anatomy of the Equine Musculoskeletal System ANNA DEE FAILS ANATOMIC NOMENCLATURE AND USAGE Foot Veterinary medical anatomists have been using the The foot consists of the hoof and all it encloses: the Nomina Anatomica Veterinaria, created by the Inter connective tissue corium (dermis), digital cushion, distal national Committee on Veterinary Gross Anatomical phalanx (coffin bone), most of the cartilages of the distal Nomenclature since 1968 to standardize the names of phalanx, distal interphalangeal (coffin) joint, distal part anatomical structures.46 This chapter endeavors to use the of the middle phalanx (short pastern bone), distal sesa most current, correct terms as outlined in that publication. moid (navicular) bone, podotrochlear bursa (navicular Nonetheless, equine practitioners need to be equally fluent bursa), several ligaments, tendons of insertion of the in older terminology, which is likely to be in wide usage common digital extensor and deep digital flexor mus among horse owners and equine professionals. This chap cles, blood vessels, and nerves. Skin between the heels is ter will provide useful and common synonyms for many also part of the foot. structures, along with their more technically correct terms. Figure 1.1 provides the directional terms for veteri HOOF WALL, SOLE, AND FROG nary anatomy that will be used in this chapter. With the exception of the ocular and oral cavity structures, the The hoof is continuous with the epidermis at the cor terms anterior, posterior, superior, and inferior are not onet, and the underlying corium of the hoof is likewise applicable to quadrupeds. continuous with the dermis of the skin. -

Developing Learning Models to Teach Equine Anatomy and Biomechanics
The University of Maine DigitalCommons@UMaine Honors College Spring 5-2017 Developing Learning Models to Teach Equine Anatomy and Biomechanics Zandalee E. Toothaker University of Maine Follow this and additional works at: https://digitalcommons.library.umaine.edu/honors Part of the Animal Sciences Commons, and the Veterinary Anatomy Commons Recommended Citation Toothaker, Zandalee E., "Developing Learning Models to Teach Equine Anatomy and Biomechanics" (2017). Honors College. 453. https://digitalcommons.library.umaine.edu/honors/453 This Honors Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Honors College by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. DEVELOPING LEARNING MODELS TO TEACH EQUINE ANATOMY AND BIOMECHANICS By Zandalee E. Toothaker A Thesis Submitted in Partial Fulfillment of the Requirements for a Degree with Honors (Animal and Veterinary Science) The Honors College University of Maine May 2017 Advisory Committee: Dr. Robert C. Causey, Associate Professor of Animal and Veterinary Sciences, Advisor Dr. David Gross, Adjunct Associate Professor in Honors (English) Dr. Sarah Harlan-Haughey, Assistant Professor of English and Honors Dr. Rita L. Seger, Researcher of Animal and Veterinary Sciences Dr. James Weber, Associate Professor and Animal and Veterinary Sciences © 2017 Zandalee Toothaker All Rights Reserved ABSTRACT Animal owners and professionals benefit from an understanding of an animal’s anatomy and biomechanics. This is especially true of the horse. A better understanding of the horse’s anatomy and weight bearing capabilities will allow people to treat and prevent injuries in equine athletes and work horses. -
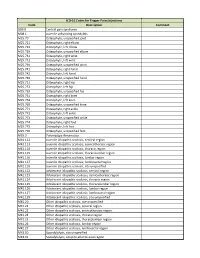
ICD-10 Codes for Trigger Point Injections
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic -

Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without
Original Article / Orijinal Araflt›rma 15 Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without Thenar Atrophy Tenar Atrofisi Olmayan Karpal Tünel Sendromlu Hastalarda Metakarpal Kemik Yo¤unlu¤unun De¤erlendirilmesi Serpil Savafl, Berna Okudan1, Hasan Rifat Koyuncuo¤lu2, Hakan Çelik, Tamer Karaaslan3, Mustafa Y›ld›z 4 Süleyman Demirel Üniversitesi T›p Fakültesi Fiziksel T›p ve Rehabilitasyon, 2Nöroloji, 3Beyin Cerrahisi ve 4Nükleer T›p Anabilim Dal›, Isparta, Türkiye, 1Yeditepe Üniversitesi T›p Fakültesi Nükleer T›p Anabilim Dal›, ‹stanbul, Türkiye Abstract Özet Objective: Bone loss due to thenar atrophy was reported in the me- Amaç: Premenopozal karpal tünel sendromlu (KTS) kad›nlarda te- tacarpal bones in premenopausal patients with carpal tunnel nar atrofiye ba¤l› olarak metakarpal kemik yo¤unlu¤u kayb› oldu- syndrome (CTS). The present study was designed to assess bone ¤u bilinmektedir. Bu çal›flman›n amac›, tenar atrofisi olmayan KTS’li density in the metacarpal bones in patients with CTS without hastalarda metakarpal kemik mineral yo¤unlu¤unu de¤erlendir- thenar atrophy and to correlate the metacarpal bone density with mek, metakarpal kemik yo¤unlu¤u ile elektrofizyolojik bulgular›, el the electrophysiological findings, hand strength and Boston gücü ve Boston Anketi aras›ndaki iliflkiyi belirlemektir. Questionnaire (BQ). Hastalar ve Yöntem: Çal›flmaya tenar atrofisi olmayan 30 KTS’li pre- Patients and Methods: Thirty premenopausal patients with CTS menopozal hasta ile 32 premenopozal kontrol olgu al›nd›. KTS’li without thenar atrophy were enrolled in this study. Thirty-two hastalar›n semptom fliddeti ve fonksiyonel durumlar› Bostan Anke- consecutive premenopausal women were included in the study as ti ile de¤erlendirildi. -

0Riginal Article the Cadaveric Study of Extensor Carpi Radialis Longus Muscle on the Developmental Basis
International J. of Healthcare & Biomedical Research, Volume: 1, Issue: 4, July 2013, Pages 241-245 0riginal article The cadaveric study of extensor carpi radialis longus muscle on the developmental basis. *Sawant SP Department of Anatomy, K. J. Somaiya Medical College, Somaiya Ayurvihar, Eastern Express Highway, Sion, Mumbai-400 022. *Corresponding author: [email protected] Abstract: Introduction: Our aim was to study the extensor carpi radialis longus muscle on the basis of development in 100 cadavers in India. Materials & Methods: This study on extensor carpi radialis longus was performed on 100 (200 specimens of superior extremities) embalmed donated cadavers (90 males & 10 females) in the department of Anatomy of K.J.Somaiya Medical College, Sion, Mumbai, India. Observations: Out of 200 specimens the variation was observed in 22 specimens. The extensor carpi radialis brevis was absent and the extensor carpi radialis longus was giving two tendons in the second compartment of extensor retinaculum before its insertion while passing deep to the abductor pollicis longus. The arterial pattern of upper limb were also observed. The variation was unilateral. The left upper limb was normal. Conclusions: A lack of knowledge of such type of variations might complicate surgical repair. Keywords: Extensor Carpi Radialis Longus, Physiotherapist, Electromyography. Introduction: The extrinsic extensor muscles of the humerus, the lateral intermuscular septum, and the hand are located in the back of the forearm and by a few fibers at the lateral epicondyle of the have long tendons connecting them to bones in the humerus. Distal to this, the extensor carpi radialis hand, where they exert their action. -
Case Reports Series A, B, C & D Table of Contents
ACTEC X H E • • C S A T S E R REPO Case Reports Series A, B, C & D Table of ConTents Revision Total Joint Series A, Number 1 ..................................................................................................................................................... 3 Use of opteform® to Repair failed Total Knee Prosthesis with osteolysis, Harry Schmaltz, MD Series A, Number 2 ..................................................................................................................................................... 5 Use of opteform® to Repair Acetabular osteolysis Series A, Number 4 ..................................................................................................................................................... 7 large osteolytic Defect Repair Using opteform® Through an Illiac Window, Abbott Kagan, MD Series A, Number 5 ..................................................................................................................................................... 9 Repair of Acetabular fracture and osteolysis with opteform®-Two Year follow-Up, Wayne Moody, MD fACS Series A, Number 6 ................................................................................................................................................... 11 Acetabular Reconstruction with opteform® and Reconstruction Ring, Wayne Moody, MD fACS Series A, Number 7 ................................................................................................................................................... 13 Use of opteform® -

DISTAL RADIUS FRACTURES: REHABILITATIVE EVALUATION and TREATMENT PDH Academy Course #OT-1901 | 5 CE HOURS
CONTINUING EDUCATION for Occupational Therapists DISTAL RADIUS FRACTURES: REHABILITATIVE EVALUATION AND TREATMENT PDH Academy Course #OT-1901 | 5 CE HOURS This course is offered for 0.5 CEUs (Intermediate level; Category 2 – Occupational Therapy Process: Evaluation; Category 2 – Occupational Therapy Process: Intervention; Category 2 – Occupational Therapy Process: Outcomes). The assignment of AOTA CEUs does not imply endorsement of specific course content, products, or clinical procedures by AOTA. Course Abstract This course addresses the rehabilitation of patients with distal radius fractures. It begins with a review of relevant terminology and anatomy, next speaks to medical intervention, and then examines the role of therapy as it pertains to evaluation, rehabilitation, and handling complications. It concludes with case studies. Target audience: Occupational Therapists, Occupational Therapy Assistants, Physical Therapists, Physical Therapist Assistants (no prerequisites). NOTE: Links provided within the course material are for informational purposes only. No endorsement of processes or products is intended or implied. Learning Objectives At the end of this course, learners will be able to: ❏ Differentiate between definitions and terminology pertaining to distal radius fractures ❏ Recall the normal anatomy and kinesiology of the wrist ❏ Identify elements of medical diagnosis and treatment of distal radius fractures ❏ Recognize roles of therapy as it pertains to the evaluation and rehabilitation of distal radius fractures ❏ Distinguish -

Avascular Necrosis of the Head of the Third Metacarpal Bone
Case Report J Korean Orthop Assoc 2012; 47: 146-149 • http://dx.doi.org/10.4055/jkoa.2012.47.2.146 www.jkoa.org Avascular Necrosis of the Head of the Third Metacarpal Bone Youn-Moo Heo, M.D., Sang-Bum Kim, M.D., Jin-Woong Yi, M.D., Kwang-Kyoon Kim, M.D., Jung-Bum Lee, M.D., and Seung-Kwan Ryu, M.D. Department of Orthopaedic Surgery, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea Avascular necrosis of the metacarpal head named as ‘Dieterich disease’ is a very rare condition. Because of the lack of information about the natural course and treatment of this disease, the ideal treatment has not been established as yet. We report a case of avascular necrosis that occurred at the 3rd metacarpal head after fractures of the 4th and 5th metacarpal base; this was treated conservatively and obtained the spontaneous resolution. Key words: Metacarpal bones, head, Avascular necrosis of bone Avascular necrosis occurring in the metacarpal head, which was re- which occurred after punching a sandbag around 11 months ago. ported first by Dieterich1) in 1932, is a very rare disease. This disease At that time, the patient did not have pain in the third metacarpo- occurs usually in one metacarpal head2-7) but sometimes invades phalangeal joint and there had not been any notable symptom after multiple metacarpal heads.8) There is no ideal treatment for avascular the treatment of the fracture was completed. No abnormal find- necrosis in the metacarpal head, and various progresses and results ing was observed in the third metacarpal head in simple x-ray and after treatment have been reported according to cases.9) The pres- computed tomography at the early stage of fracture and in simple x- ent authors experienced a case of avascular necrosis in the adjacent ray in 2 months after the surgery (Fig.