Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bilateral Calcified Ischiogluteal Bursitis and Shoulder Tendinopathy
Bilateral Calcified Ischiogluteal Bursitis and Conflict of Interest: None Shoulder Tendinopathy: A Case Report declared Seyyed-Mohsen Hosseininejad1,2, Saman Shakeri1, Hossein Mohebbi1, Mehdi Aarabi2, Shiva Momen3 This article has been peer reviewed. 1Shahid Beheshti University of Medical Sciences, Tehran, Iran 2 Golestan University of Medical Sciences, Gorgan, Iran Article Submitted on: 21st 3Mazandaran University of Medical Sciences, Sari, Iran January 2019 Article Accepted on: 1st ABSTRACT June 2020 The ischiogluteal bursitis which is a rare the buttock. Ischiogluteal bursitis Aspiration Funding Sources: None disorder is irregularly found between the showed calcareous deposits; local injection declared gluteus maximus and ischial tuberosity. A of corticosteroid helped the patient to get 41-year-old female with bilateral calcifying free of symptoms. Calcified ischiogluteal Correspondence to: Dr ischiogluteal bursitis and her right shoulder bursitis is a rare condition but simply Seyyed-Mohsen Hosseininejad tendinopathy were presented. She had no diagnosed on x-ray. Local steroid injection related past medical history nor trauma to could provide symptom relief. Address: Shahid Beheshti University of Medical Sciences, Tehran, Iran Keywords: Calcifying Ischiogluteal Bursitis; Aspiration; Treatment; Shoulder pain; Tendinopathy E-mail: Hosseininejad.s.mohsen INTRODUCTION painful swelling in her both buttocks. The patient @gmail.com Ischiogluteal bursitis is a rare condition in which had no related past medical history nor recent Cite this Article: bursa between the gluteus maximus muscle and major trauma. Ischial tuberosities had swelling Hosseininejad SM, ischial tuberosity, which physiologically and tenderness in. Right shoulder had positive Shakeri S, Mohebbi H, decreases the frictional force, develops impingement tests but full range of motion. Aarabi M, Momen S. -

Endoscopic Hamstring Repair
Lorem Ipsum Endoscopic Hamstring Repair Carlos A. Guanche, MD Southern California Orthopedic Institute 12 Lorem Ipsum 2 Endoscopic Hamstring Repair With the expansion of knowledge regarding hip pathologies as a result of the increased treatment of hip problems arthroscopically has come an expanded treatment of many injuries that were previously treated through open methods. The treatment of symptomatic ischial bursitis and hamstring injuries is one such area. In this paper, the author describes the surgical procedure and discusses the findings and preliminary outcomes in a group of the first 15 patients undergoing the procedure. The clinical rationale associated with the treatment algorithm is also discussed. Hamstring injuries have been effectively addressed in the past with a variety of open methods.(1,2) However, the endoscopic management of much pathology previously treated with more invasive, open approaches has evolved. The technique described in this chapter is another such evolution. Hamstring injuries are common and can affect all levels of The hamstrings originate from the ischial tuberosity and athletes. (3-7) There is a continuum of hamstring injuries insert distally below the knee on the proximal tibia, with the that can range from musculotendinous strains to avulsion exception of the short head of the biceps femoris. The tibial injuries. (3,4) Most hamstring strains do not require surgical branch of the sciatic nerve innervates the semitendinosus, intervention and resolve with a variety of modalities and semimembranosus, and the peroneal branch of the sciatic rest. (3-7) In some patients, chronic pain can occur at the nerve innervates the long head of the biceps femoris.(5) hamstring origin from either partial or complete tears as well as from chronic ischial bursitis. -

(Bucked Shins) in the Flat Racing Horse: Prevalence, Diagnosis, Pathogenesis, and Associated Factors
Journal of Dairy, Veterinary & Animal Research Mini Review Open Access A review of dorsal metacarpal disease (bucked shins) in the flat racing horse: prevalence, diagnosis, pathogenesis, and associated factors Abstract Volume 5 Issue 6 - 2017 Dorsal metacarpal disease (DMD) is the most common cause of lostdays to training S Couch,1 BD Nielsen2 and racing in Thoroughbred racehorses. Colloquially termed ‘bucked’ or ‘sore’ shins, 1Royal (Dick) School of Veterinary Studies, University of this initially painful condition commonly occurs in the first season of training and can Edinburgh, United Kingdom raise welfare concerns. Clinical signs include pain with digital palpation and swelling 2Department of Animal Science, Michigan State University, USA on the dorsal, and sometimes dorso-medial, aspect of the third metacarpal (McIII). Periostitis and excessive growth of periosteal bone can be present as a response to Correspondence: Brian D Nielsen, Michigan State University, high strain cyclic fatigue. Whilst DMD can resolve with rest or reduced exercise, it Department of Animal Science, 474 S. Shaw Lane, East Lansing, can leave bone susceptible to future catastrophic fracture at the same site, particularly MI 48824 1225, USA, Tel 517 432 1378, Fax 517 353 1699, saucer fractures of the lamellar bone of the diaphysis. Some trainers continue to work Email [email protected] an animal through DMD, with the view that it will only happen once, but it can re- occur. Additionally, the animal is in discomfort and has a weakened skeletal system. Received: September 13, 2017 | Published: September 25, In vivo studies of the effects of cyclic strain on the skeletal system of Thoroughbreds 2017 are notoriously difficult, due to the many variables involved and in vitro studies cannot mimic true training and racing conditions. -

Clinical Medical Policy
CLINICAL MEDICAL POLICY Noninvasive Electrical Bone Growth Stimulators Policy Name: (osteogenesis stimulators) Policy Number: MP-070-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 12/15/2018 Issue Date: 01/15/2019 Effective Date: 01/15/2019 Annual Approval Date: 10/17/2019 Revision Date: N/A Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 78 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical and DME benefits of the Company’s Medicaid products for medically necessary noninvasive electrical bone growth stimulators as treatment of nonunion long bone fractures or congenital pseudarthrosis. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-070-MD-PA Page 1 of 78 DEFINITIONS Prior Authorization Review Panel - A panel of representatives from within the PA Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Non-invasive (Osteogenic) Electrical Bone Growth Stimulator – A device that uses pulsed- electromagnetic fields, capacitative coupling or combined magnetic fields to generate a weak electric current through the target site. -

Fractures of the Neck of the Fifth Metacarpal Bone. Medium-Term Results in 28 Cases Treated by Percutaneous Transverse Pinning I
Injury, Int. J. Care Injured 43 (2012) 242–245 Contents lists available at SciVerse ScienceDirect Injury jo urnal homepage: www.elsevier.com/locate/injury Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning V. Potenza *, R. Caterini, F. De Maio, S. Bisicchia, P. Farsetti Department of Orthopaedic Surgery, University of Rome ‘Tor Vergata’, Rome, Italy A R T I C L E I N F O A B S T R A C T Article history: The purpose of this study was to report the medium-term results in 28 patients affected by closed Accepted 27 October 2011 displaced fractures of the neck of the fifth metacarpal bone (boxer’s fracture) with an associated severe swelling of the hand, who were treated with percutaneous transverse K-wire pinning, to verify the Keywords: effectiveness of this surgical treatment. We opted for this treatment in all cases in which malrotation of Boxer’s fracture the fifth finger and volar angulation of the metacarpal head greater than 308 were associated with a Transverse pinning severe swelling of the hand. All the patients were reviewed clinically and radiologically at an average of Metacarpal neck fracture 25 months after surgery. At the final follow-up, no patient reported residual pain. All patients had full extension of the fifth finger, except two in whom we observed a limitation of the extension of the fifth metacarpophalangeal (MP) joint of about 108, without significant impairment of hand function. All patients had at least 908 flexion of the fifth MP joint and full range of motion of the interphalangeal (IP) joints. -

Functional Anatomy of the Equine Musculoskeletal System
1 CHAPTER Functional Anatomy of the Equine Musculoskeletal System ANNA DEE FAILS ANATOMIC NOMENCLATURE AND USAGE Foot Veterinary medical anatomists have been using the The foot consists of the hoof and all it encloses: the Nomina Anatomica Veterinaria, created by the Inter connective tissue corium (dermis), digital cushion, distal national Committee on Veterinary Gross Anatomical phalanx (coffin bone), most of the cartilages of the distal Nomenclature since 1968 to standardize the names of phalanx, distal interphalangeal (coffin) joint, distal part anatomical structures.46 This chapter endeavors to use the of the middle phalanx (short pastern bone), distal sesa most current, correct terms as outlined in that publication. moid (navicular) bone, podotrochlear bursa (navicular Nonetheless, equine practitioners need to be equally fluent bursa), several ligaments, tendons of insertion of the in older terminology, which is likely to be in wide usage common digital extensor and deep digital flexor mus among horse owners and equine professionals. This chap cles, blood vessels, and nerves. Skin between the heels is ter will provide useful and common synonyms for many also part of the foot. structures, along with their more technically correct terms. Figure 1.1 provides the directional terms for veteri HOOF WALL, SOLE, AND FROG nary anatomy that will be used in this chapter. With the exception of the ocular and oral cavity structures, the The hoof is continuous with the epidermis at the cor terms anterior, posterior, superior, and inferior are not onet, and the underlying corium of the hoof is likewise applicable to quadrupeds. continuous with the dermis of the skin. -

Evaluation of the Hip Adam Lewno, DO PCSM Fellow, University of Michigan Primary Care Sports Update 2017 DEPARTMENT of FAMILY MEDICINE
DEPARTMENT OF FAMILY MEDICINE Evaluation of the Hip Adam Lewno, DO PCSM Fellow, University of Michigan Primary Care Sports Update 2017 DEPARTMENT OF FAMILY MEDICINE Disclosures • Financial: None • Images: I would like to acknowledge the work of the original owners and artists of the pictures used today DEPARTMENT OF FAMILY MEDICINE Objectives • Identify the main anatomic components of the hip • Perform basic Hip examination along with associated special tests • Use a group educational model to correlate Hip examination with hip anatomy DEPARTMENT OF FAMILY MEDICINE Why do we care about the Hip? • The hip distributes weight between the appendicular and axial skeleton but it is also the joint from which motion is initiated and executed for the lower extremity • Forces through the hip joint can reach 3-5 times the body weight during running and jumping • 10-24% of athletic injuries in children are hip related • 5-6% adult athletic injuries in adults are hip and pelvis DEPARTMENT OF FAMILY MEDICINE Why is the Hip difficult to diagnosis? The hip is difficult to diagnosis secondary to parallel presenting symptoms of back pain which can exist concomitantly or independently of hip pathology DEPARTMENT OF FAMILY MEDICINE Hip Anatomy • Bone • Ligament • Muscle • Nerve • Vessels DEPARTMENT OF FAMILY MEDICINE DEPARTMENT OF FAMILY MEDICINE Bones DEPARTMENT OF FAMILY MEDICINE Ligaments DEPARTMENT OF FAMILY MEDICINE Everything is Connected DEPARTMENT OF FAMILY MEDICINE Muscles DEPARTMENT OF FAMILY MEDICINE Important Movers DEPARTMENT OF FAMILY MEDICINE -

Nonspinal Musculoskeletal Disorders That Mimic Spinal Conditions
REVIEW DHRUV B. PATEDER, MD JOHN BREMS, MD ISADOR LIEBERMAN, MD, FRCS(C)* CME Attending Spine Surgeon, Steadman Cleveland Clinic Spine Institute, Cleveland Clinic Spine Institute, and Department CREDIT Hawkins Clinic Spine Surgery, Cleveland Clinic of Orthopaedic Surgery, Cleveland Clinic; Professor Frisco/Vail, CO of Surgery, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University GORDON R. BELL, MD ROBERT F. McLAIN, MD Associate Director, Center for Spine Cleveland Clinic Spine Institute, Health, The Neurological Institute, Cleveland Clinic Cleveland Clinic Masquerade: Nonspinal musculoskeletal disorders that mimic spinal conditions ■ ABSTRACT OT ALL PAIN in the neck or back actual- N ly originates from the spine. Sometimes Nonspinal musculoskeletal disorders frequently cause pain in the neck or back is caused by a prob- neck and back pain and thus can mimic conditions of the lem in the shoulder or hip or from peripheral spine. Common mimics are rotator cuff tears, bursitis in nerve compression in the arms or legs. the hip, peripheral nerve compression, and arthritis in the This article focuses on the diagnostic fea- shoulder and hip. A thorough history and physical tures of common—and uncommon—non- examination, imaging studies, and ancillary testing can spinal musculoskeletal problems that can mas- usually help determine the source of pain. querade as disorders of the spine. A myriad of nonmusculoskeletal disorders can also cause ■ KEY POINTS neck or back pain, but they are beyond the scope of this article. Medical disorders that Neck pain is commonly caused by shoulder problems can present as possible spinal problems have such as rotator cuff disease, glenohumeral arthritis, and been reviewed in the December 2007 issue of humeral head osteonecrosis. -

Developing Learning Models to Teach Equine Anatomy and Biomechanics
The University of Maine DigitalCommons@UMaine Honors College Spring 5-2017 Developing Learning Models to Teach Equine Anatomy and Biomechanics Zandalee E. Toothaker University of Maine Follow this and additional works at: https://digitalcommons.library.umaine.edu/honors Part of the Animal Sciences Commons, and the Veterinary Anatomy Commons Recommended Citation Toothaker, Zandalee E., "Developing Learning Models to Teach Equine Anatomy and Biomechanics" (2017). Honors College. 453. https://digitalcommons.library.umaine.edu/honors/453 This Honors Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Honors College by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. DEVELOPING LEARNING MODELS TO TEACH EQUINE ANATOMY AND BIOMECHANICS By Zandalee E. Toothaker A Thesis Submitted in Partial Fulfillment of the Requirements for a Degree with Honors (Animal and Veterinary Science) The Honors College University of Maine May 2017 Advisory Committee: Dr. Robert C. Causey, Associate Professor of Animal and Veterinary Sciences, Advisor Dr. David Gross, Adjunct Associate Professor in Honors (English) Dr. Sarah Harlan-Haughey, Assistant Professor of English and Honors Dr. Rita L. Seger, Researcher of Animal and Veterinary Sciences Dr. James Weber, Associate Professor and Animal and Veterinary Sciences © 2017 Zandalee Toothaker All Rights Reserved ABSTRACT Animal owners and professionals benefit from an understanding of an animal’s anatomy and biomechanics. This is especially true of the horse. A better understanding of the horse’s anatomy and weight bearing capabilities will allow people to treat and prevent injuries in equine athletes and work horses. -
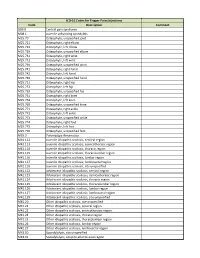
ICD-10 Codes for Trigger Point Injections
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic -

Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without
Original Article / Orijinal Araflt›rma 15 Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without Thenar Atrophy Tenar Atrofisi Olmayan Karpal Tünel Sendromlu Hastalarda Metakarpal Kemik Yo¤unlu¤unun De¤erlendirilmesi Serpil Savafl, Berna Okudan1, Hasan Rifat Koyuncuo¤lu2, Hakan Çelik, Tamer Karaaslan3, Mustafa Y›ld›z 4 Süleyman Demirel Üniversitesi T›p Fakültesi Fiziksel T›p ve Rehabilitasyon, 2Nöroloji, 3Beyin Cerrahisi ve 4Nükleer T›p Anabilim Dal›, Isparta, Türkiye, 1Yeditepe Üniversitesi T›p Fakültesi Nükleer T›p Anabilim Dal›, ‹stanbul, Türkiye Abstract Özet Objective: Bone loss due to thenar atrophy was reported in the me- Amaç: Premenopozal karpal tünel sendromlu (KTS) kad›nlarda te- tacarpal bones in premenopausal patients with carpal tunnel nar atrofiye ba¤l› olarak metakarpal kemik yo¤unlu¤u kayb› oldu- syndrome (CTS). The present study was designed to assess bone ¤u bilinmektedir. Bu çal›flman›n amac›, tenar atrofisi olmayan KTS’li density in the metacarpal bones in patients with CTS without hastalarda metakarpal kemik mineral yo¤unlu¤unu de¤erlendir- thenar atrophy and to correlate the metacarpal bone density with mek, metakarpal kemik yo¤unlu¤u ile elektrofizyolojik bulgular›, el the electrophysiological findings, hand strength and Boston gücü ve Boston Anketi aras›ndaki iliflkiyi belirlemektir. Questionnaire (BQ). Hastalar ve Yöntem: Çal›flmaya tenar atrofisi olmayan 30 KTS’li pre- Patients and Methods: Thirty premenopausal patients with CTS menopozal hasta ile 32 premenopozal kontrol olgu al›nd›. KTS’li without thenar atrophy were enrolled in this study. Thirty-two hastalar›n semptom fliddeti ve fonksiyonel durumlar› Bostan Anke- consecutive premenopausal women were included in the study as ti ile de¤erlendirildi. -

Prolo Your Pain Away: Curing Chronic Pain with Prolotherapy
PROLO YOUR PAIN AWAY®, 4TH EDITION CUR NG CHRONICWITH PAIN PROLOTHERAPY Ross A. Hauser, MD & Marion A. Boomer Hauser, MS, RD PROLO YOUR PAIN AWAY! Curing Chronic Pain with Prolotherapy 4TH EDITION Ross A. Hauser, MD & Marion A. Boomer Hauser, MS, RD Sorridi Business Consulting Library of Congress Cataloging-in-Publication Data Hauser, Ross A., author. Prolo your pain away! : curing chronic pain with prolotherapy / Ross A. Hauser & Marion Boomer Hauser. — Updated, fourth edition. pages cm Includes bibliographical references and index. ISBN 978-0-9903012-0-2 1. Intractable pain—Treatment. 2. Chronic pain— Treatment. 3. Sclerotherapy. 4. Musculoskeletal system —Diseases—Chemotherapy. 5. Regenerative medicine. I. Hauser, Marion A., author. II. Title. RB127.H388 2016 616’.0472 QBI16-900065 Text, illustrations, cover and page design copyright © 2017, Sorridi Business Consulting Published by Sorridi Business Consulting 9738 Commerce Center Ct., Fort Myers, FL 33908 Printed in the United States of America All rights reserved. International copyright secured. No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form by any means— electronic, mechanical, photocopying, recording, or otherwise—without the prior written permission of the publisher. The only exception is in brief quotations in printed reviews. Scripture quotations are from: Holy Bible, New International Version®, NIV® Copyrights © 1973, 1978, 1984, International Bible Society. Used by permission of Zondervan Publishing House. All rights reserved.