Cowal Palliative Care Recommendation Endorsed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Emergency Department Activity
NHS Scotland - Emergency Department Activity Attendances and Performance against the 4-hour Waiting Time Standard This is an ISD Scotland National Statistics release. The Scottish Government waiting time standard for emergency departments is that 98 % of all attendances should be seen within 4 hours. The figures presented in these tables detail the performance of each individual site and NHS board against the standard. Time Period: Apr-10 to Mar-11 Source: A&E data mart, ISD Scotland Date: 07 May 2012 List of Tables Table 1: Attendances and performance against 4-hour standard, Apr-10 to Mar-11 Total attendances, number of attendances breaching standard and attendances meeting standard (number and percentage). Figures are given at site and NHS Board level. Table 2: Attendances, Apr-10 to Mar-11 Summary table of attendances only. Figures are given at site and NHS Board level. Table 3: Performance against 4-hour standard, Apr-10 to Mar-11 Summary table of percentage of attendances meeting standard. Figures are given at site and NHS Board level. Notes: 1) The waiting time is defined as the time of arrival until the time of discharge, admission or transfer. 2) New presentations only; excludes planned return and recall attendances. 3) There are two types of site that provide emergency care; • ED - Emergency Departments; sites that provide a 24 hour emergency medicine consultant led service • MIU/Other - sites including minor injuries units (MIU), small hospitals and health centres in rural areas that carry out emergency department related activity and are GP or Nurse led. They may or may not be open 24 hours. -

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

The Manse, Main Street, Kyle of Lochalsh, IV40 8DA Property Description
The Manse, Main Street, Kyle of Lochalsh, IV40 8DA Property Description Five-bedroom extended detached bungalow located in the picturesque village of Kyle. Set within the beautiful Scottish landscape in the county of Ross-shire the property presents a wonderful opportunity to purchase on the much sought after northwest coast of Scotland. The bright and spacious property benefits from a flexible floor plan and good sized rooms throughout. It has scope for many future uses and has excellent features including double glazing and storage space. The accommodation comprises: Ground Floor - Entrance porch, hall, living room, dining room, kitchen, utility room, five bedrooms, bathroom and shower room. Gross Internal Floor Area: 145 square metres. Externally the property features garden grounds to the front side and rear. The front garden is a mixture of grass, colourful trees and shrubbery. A driveway with space for numerous cars leads to a detached garage which offers a multi-use space. There is also a fully enclosed rear garden. Local Area Kyle of Lochalsh is a lively highland village with many local amenities including banks, shops, supermarket and butchers. There are many leisure activities in the area such as a leisure pool & gym, hotels, restaurants and bars. Additional facilities include a chemist, dentist surgery & medical centre. There is a primary school within the village and secondary schooling is available in the nearby village of Plockton to which a school bus runs daily. There is a railway station within the village which offers direct services to Inverness where the airport (106 miles) has regular domestic and international flights. -

Highlands and Islands Patients' Travel Expenses Claim Form
FOR ADMIN USE – TRAVEL WARRANT YES / NO NHS HIGHLAND HIGHLANDS AND ISLANDS PATIENTS’ TRAVEL EXPENSES CLAIM FORM SECTION 1: TO BE COMPLETED BY WARD OR RECEPTION STAFF – PLEASE PRINT PATIENT’S NAME: ………………………………………………………………... CHI NUMBER: .................................................... OR DATE OF BIRTH ADDRESS: ………………………………………………………………………………………. ……………………………………………………………………………………….. …………………………………………………………………………………........ POSTCODE …………................................. DAYTIME CONTACT NO: ................................................. NAME & ADDRESS OF YOUR GP PRACTICE : ……………………………………………………………………………............…… SECTION 2: TO BE COMPLETED BY (OR ON BEHALF OF) PATIENT HOSPITAL ATTENDED: ………………………………………………………………………………………………….. WARD NUMBER/NAME: ………………………............... HOSPITAL CONSULTANT: …………………….........………… INPATIENTS: DATE OF ADMISSION: ….....…/….....…/….....… TIME OF ADMISSION: ……........……….. DATE OF DISCHARGE: .……../……...../……...... TIME OF DISCHARGE: ……........………. OUTPATIENTS AND DAYCASE PATIENTS: DATES AND TIMES OF APPOINTMENTS: 1. ...…../……../…….. …...... : …….. 3. ……../… …../…... …..... : …….. 2. …../… …../… ….. …….. : …….. 4. ……../……../…….. …….. : …….. SECTION 3: TO BE COMPLETED BY HOSPITAL STAFF I confirm that the patient named above attended this hospital on the dates stated: HOSPITAL STAMP Signature: ……………………………………………………...................................... Print Name : .......................................................................................................... Designation: …………......................................……………………………………… -

NHS Highland Board November 2019 Item 6 CHIEF EXECUTIVE AND
NHS Highland Board November 2019 Item 6 CHIEF EXECUTIVE AND DIRECTORS REPORT – EMERGING ISSUES AND UPDATES Report by Iain Stewart, Chief Executive The Board is asked to: • Note the updates provided in the report. Introduction from CEO The engagement strategy which is helping to shape the ‘Culture Fit for the Future’ has been moving ahead. Fiona Hogg will be giving a detailed update on our progress with our Culture Programme later in the agenda. I am pleased with the progress which is being made, it’s a long-term piece of work which needs careful research and planning to make sure we understand the problems we need to address. There are some key milestones being achieved and presented at this Board meeting. A governance structure is in place and our revised plans are ready to be agreed and rolled out. Many of the actions planned have been shaped by our ongoing engagement with the Board and with our colleagues across North Highland and Argyll & Bute and I’m delighted that our impending review in Argyll & Bute is going to provide further valuable insights and information. In terms of the cost improvement programme, we continue to make good progress, with the current level of identified opportunities valued at £29M which when adjusted for the likelihood of delivery reduces to £22M. Of particular note is that 80% of the forecast savings are recurrent so the savings gain will benefit future financial years. Workstreams are ensuring the remaining plans in this financial year are approved, that ideas are progressed to plans and that changes already implemented go on to deliver the expected savings. -

Wester Ross Ros An
Scottish Natural Heritage Explore for a day Wester Ross Ros an lar Wester Ross has a landscape of incredible beauty and diversity Historically people have settled along the seaboard, sustaining fashioned by a fascinating geological history. Mountains of strange, themselves by combining cultivation and rearing livestock with spectacular shapes rise up from a coastline of diverse seascapes. harvesting produce from the sea. Crofting townships, with their Wave battered cliffs and crevices are tempered by sandy beaches small patch-work of in-bye (cultivated) fields running down to the or salt marsh estuaries; fjords reach inland several kilometres. sea can be found along the coast. The ever changing light on the Softening this rugged landscape are large inland fresh water lochs. landscape throughout the year makes it a place to visit all year The area boasts the accolade of two National Scenic Area (NSA) round. designations, the Assynt – Coigach NSA and Wester Ross NSA, and three National Nature Reserves; Knockan Crag, Corrieshalloch Symbol Key Gorge and Beinn Eighe. The North West Highland Geopark encompasses part of north Wester Ross. Parking Information Centre Gaelic dictionary Paths Disabled Access Gaelic Pronunciation English beinn bayn mountain gleann glyown glen Toilets Wildlife watching inbhir een-er mouth of a river achadh ach-ugh field mòr more big beag bake small Refreshments Picnic Area madainn mhath mat-in va good morning feasgar math fess-kur ma good afternoon mar sin leat mar shin laht goodbye Admission free unless otherwise stated. 1 11 Ullapool 4 Ullapul (meaning wool farm or Ulli’s farm) This picturesque village was founded in 1788 as a herring processing station by the British Fisheries Association. -
Caithness and Sutherland Proposed Local Development Plan Committee Version November, 2015
Caithness and Sutherland Proposed Local Development Plan Committee Version November, 2015 Proposed CaSPlan The Highland Council Foreword Foreword Foreword to be added after PDI committee meeting The Highland Council Proposed CaSPlan About this Proposed Plan About this Proposed Plan The Caithness and Sutherland Local Development Plan (CaSPlan) is the second of three new area local development plans that, along with the Highland-wide Local Development Plan (HwLDP) and Supplementary Guidance, will form the Highland Council’s Development Plan that guides future development in Highland. The Plan covers the area shown on the Strategy Map on page 3). CaSPlan focuses on where development should and should not occur in the Caithness and Sutherland area over the next 10-20 years. Along the north coast the Pilot Marine Spatial Plan for the Pentland Firth and Orkney Waters will also influence what happens in the area. This Proposed Plan is the third stage in the plan preparation process. It has been approved by the Council as its settled view on where and how growth should be delivered in Caithness and Sutherland. However, it is a consultation document which means you can tell us what you think about it. It will be of particular interest to people who live, work or invest in the Caithness and Sutherland area. In preparing this Proposed Plan, the Highland Council have held various consultations. These included the development of a North Highland Onshore Vision to support growth of the marine renewables sector, Charrettes in Wick and Thurso to prepare whole-town visions and a Call for Sites and Ideas, all followed by a Main Issues Report and Additional Sites and Issues consultation. -
(Public Pack)Agenda Document for Integration Joint Board (IJB), 27/05/2020 13:00
Public Document Pack 20 May 2020 NOTICE OF MEETING A meeting of the INTEGRATION JOINT BOARD (IJB) will be held VIA SKYPE on WEDNESDAY, 27 MAY 2020 at 1:00 PM, which you are requested to attend. BUSINESS 1. APOLOGIES FOR ABSENCE 2. DECLARATIONS OF INTEREST 3. MINUTES (Pages 3 - 12) Integration Joint Board held on 25 March 2020 4. MINUTES OF COMMITTEES (a) Clinical and Care Governance Committee held on 23 January 2020 (to follow) (b) Finance and Policy Committee held on 6 March 2020 (Pages 13 - 16) (c) Clinical and Care Governance Committee held on 26 March 2020 (to follow) (d) Finance and Policy Committee held on 27 March 2020 (Pages 17 - 20) 5. CHIEF OFFICER'S REPORT (Pages 21 - 24) Report by Chief Officer 6. COVID-19 MOBILISATION READINESS UPDATE AND LOOK FORWARD TO LIVING AND OPERATING WITH COVID-19 (Pages 25 - 36) Report by Head of Strategic Planning and Performance 7. THE ROLE OF PUBLIC HEALTH TO DATE IN THE COVID -19 RESPONSE (Pages 37 - 54) Report by Associate Director of Public Health 8. UPDATE ON PROGRESS WITH THE STURROCK REVIEW ACTIONS INCLUDING A REPORT ON THE ARGYLL & BUTE CULTURE SURVEY AND PLANS FOR THE LAUNCH OF THE HEALING PROCESS (Pages 55 - 118) Report by Chief Officer and Director of Human Resources and Organisational Development NHS Highland 9. STAFF HEALTH AND WELLBEING (a) Employee / Staff Wellbeing and Resilience / COVID-19 (Pages 119 - 144) Report by Head of Customer Support Services (b) HR Resourcing (Pages 145 - 156) Report by Head of Customer Support Services 10. ENHANCED CARE HOME ASSURANCE (Pages 157 - 168) Report by Head of Adult Care 11. -
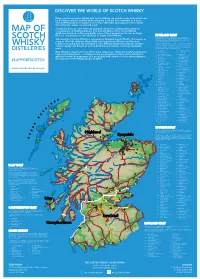
2019 Scotch Whisky
©2019 scotch whisky association DISCOVER THE WORLD OF SCOTCH WHISKY Many countries produce whisky, but Scotch Whisky can only be made in Scotland and by definition must be distilled and matured in Scotland for a minimum of 3 years. Scotch Whisky has been made for more than 500 years and uses just a few natural raw materials - water, cereals and yeast. Scotland is home to over 130 malt and grain distilleries, making it the greatest MAP OF concentration of whisky producers in the world. Many of the Scotch Whisky distilleries featured on this map bottle some of their production for sale as Single Malt (i.e. the product of one distillery) or Single Grain Whisky. HIGHLAND MALT The Highland region is geographically the largest Scotch Whisky SCOTCH producing region. The rugged landscape, changeable climate and, in The majority of Scotch Whisky is consumed as Blended Scotch Whisky. This means as some cases, coastal locations are reflected in the character of its many as 60 of the different Single Malt and Single Grain Whiskies are blended whiskies, which embrace wide variations. As a group, Highland whiskies are rounded, robust and dry in character together, ensuring that the individual Scotch Whiskies harmonise with one another with a hint of smokiness/peatiness. Those near the sea carry a salty WHISKY and the quality and flavour of each individual blend remains consistent down the tang; in the far north the whiskies are notably heathery and slightly spicy in character; while in the more sheltered east and middle of the DISTILLERIES years. region, the whiskies have a more fruity character. -

8-12 Weeks Questionnaire
Scottish Government Maternal and Infant Nutrition Survey Investigating health care and early feeding choices and experiences in the first 12 weeks following the birth of your new baby This is a survey about your choices and experiences in the first 12 weeks following the birth of your new baby. Please complete this questionnaire with respect to your baby who was born between March and April 2017. The information you provide will help us to understand more about the choices new parents make and help health care professionals to better support new parents. All of the answers you provide will be entirely confidential. Please read the enclosed letter for more information about this survey. Instructions The survey takes around 15-20 minutes to complete. Please answer all questions, unless the instructions ask you to skip a question. For most questions, you will be asked to put a tick in the box next to the statement which most applies to you. For example, if your answer is yes, write in a tick as below: P Yes No Don’t worry if you make a mistake; just cross it out and tick the correct answer. Sometimes you will be asked to write in a number. Please enter numbers as figures rather than words. For example: 6 Weeks 2 Days If you prefer, you can complete this survey online at: survey.natcen.ac.uk/MINS5 You will be asked to enter the User Code that can be found on the letter that came with this survey. Alternatively, you can give your answers by calling the FREEPHONE survey helpline on 0800 652 4568. -

4.11 Chief Executive and Directors Report
NHS Highland Board 24 July 2018 Item 4.11 CHIEF EXECUTIVE AND DIRECTORS REPORT – EMERGING ISSUES AND UPDATES Report by Elaine Mead, Chief Executive The Board is asked to: • Note the updates provided in the report. Chief Officer Argyll and Bute Health and Social Care Partnership It is with much regret to report that Christina West has resigned from the post of Chief Officer for Argyll and Bute Health and Social Care Partnership with a leaving date of 30th September 2018. Integration of health and social care has been one of the most significant changes in the public sector for decades. Under Christina’s Leadership she leaves Argyll and Bute’s Health and Social Care Partnership in a positive position to move forward, with plans in place to redesign services not least to meet the demographic challenges. Christina takes with her our grateful thanks, for her hard work, determination and commitment to developing health and social care services for the people of Argyll and Bute. She embraced the Highland Quality Approach and has been an invaluable member of NHS Highland’s Senior Leadership team. The recruitment process is underway to secure a new Chief Officer. Dr Grays Temporary Service Model for Women and Children’s services A new temporary service model for Women and Children’s services at Dr Gray’s Hospital is to be put in place to allow maternity and paediatric service to continue in Elgin. The change comes after NHS Education for Scotland said initial indications were that only two trainee doctors had elected to work at Dr Gray’s at the next intake in August – six less than the number required.