METHODICAL GUIDANCE for the Lecture Academic Subject Human Anatomy Module No 3 "The Heart. Vessels and Nerves of the Head
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Superficial (And Intermediate) Cervical Plexus Block
Superficial (and Intermediate) Cervical Plexus Block Indications: -Tympanomastoid surgery. When combined with the auricular branch of the vagus (‘nerve of arnold’) by infiltrating subcutaneously into the medial side of the tragus), obviates the need for opiates. -Pinnaplasty or Otoplasty -Lymph node excision (within the anterior and posterior triangles of the neck) -Clavicular surgery or fractures (may require intermediate cervical plexus block and its combination with interscalene block, see below) -Central Venous Catheters: Renal replacement therapy central venous catheters, tunnelled central venous catheters and portacaths inserted into the subclavian or jugular veins (may require combination with ‘Pecs 1’ block for component of pain below the clavicle) -Tracheostomy (see below discussion on safety profile of performing bilateral blocks and risks of respiratory distress due to phrenic nerve or recurrent largyngeal nerve block) -More commonly in adults: thyroid (again, bilateral) and carotid surgery Contraindications: -local sepsis or rash Anatomy: The cervical plexus arises from C1-C4 mixed spinal nerves (fig. 1): Somatic sensory branches: -arise from C2-C4 as the mixed spinal nerves leave the sulcus between the anterior and posterior tubercles of the transverse process (note C7 does not have an anterior tubercle or bifid spinous process): -pass between longus capitis and middle scalene perforating the prevertebral fascia. Note at C4 level the anterior scalene has largely disappeared having taken the bulk of its vertebral bony origin lower down. The bulkiest of the scalene muscles is the middle scalene and remains in view at this level: -then pass behind the internal jugular vein out into the potential space between the investing layer of deep fascia ensheathing the sternocleidomastoid, and the prevertebral layer of deep fascia covering levator scapulae (fig. -
33. Spinal Nerves. Cervical Plexus
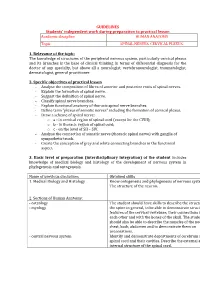
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -

The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -

A Comprehensive Review of Anatomy and Regional Anesthesia Techniques of Clavicle Surgeries
vv ISSN: 2641-3116 DOI: https://dx.doi.org/10.17352/ojor CLINICAL GROUP Received: 31 March, 2021 Research Article Accepted: 07 April, 2021 Published: 10 April, 2021 *Corresponding author: Dr. Kartik Sonawane, Uncovering secrets of the Junior Consultant, Department of Anesthesiol- ogy, Ganga Medical Centre & Hospitals, Pvt. Ltd. Coimbatore, Tamil Nadu, India, E-mail: beauty bone: A comprehensive Keywords: Clavicle fractures; Floating shoulder sur- gery; Clavicle surgery; Clavicle anesthesia; Procedure review of anatomy and specific anesthesia; Clavicular block regional anesthesia techniques https://www.peertechzpublications.com of clavicle surgeries Kartik Sonawane1*, Hrudini Dixit2, J.Balavenkatasubramanian3 and Palanichamy Gurumoorthi4 1Junior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 2Fellow in Regional Anesthesia, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 3Senior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 4Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India Abstract The clavicle is the most frequently fractured bone in humans. General anesthesia with or without Regional Anesthesia (RA) is most frequently used for clavicle surgeries due to its complex innervation. Many RA techniques, alone or in combination, have been used for clavicle surgeries. These include interscalene block, cervical plexus (superficial and deep) blocks, SCUT (supraclavicular nerve + selective upper trunk) block, and pectoral nerve blocks (PEC I and PEC II). The clavipectoral fascial plane block is also a safe and simple option and replaces most other RA techniques due to its lack of side effects like phrenic nerve palsy or motor block of the upper limb. -

Anatomic Connections of the Diaphragm: Influence of Respiration on the Body System
Journal of Multidisciplinary Healthcare Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Anatomic connections of the diaphragm: influence of respiration on the body system Bruno Bordoni1 Abstract: The article explains the scientific reasons for the diaphragm muscle being an important Emiliano Zanier2 crossroads for information involving the entire body. The diaphragm muscle extends from the trigeminal system to the pelvic floor, passing from the thoracic diaphragm to the floor of the 1Rehabilitation Cardiology Institute of Hospitalization and Care with mouth. Like many structures in the human body, the diaphragm muscle has more than one Scientific Address, S Maria Nascente function, and has links throughout the body, and provides the network necessary for breathing. Don Carlo Gnocchi Foundation, 2EdiAcademy, Milano, Italy To assess and treat this muscle effectively, it is necessary to be aware of its anatomic, fascial, and neurologic complexity in the control of breathing. The patient is never a symptom localized, but a system that adapts to a corporeal dysfunction. Keywords: diaphragm, fascia, phrenic nerve, vagus nerve, pelvis Anatomy and anatomic connections The diaphragm is a dome-shaped musculotendinous structure that is very thin (2–4 mm) and concave on its lower side and separates the chest from the abdomen.1 There is a central tendinous portion, ie, the phrenic center, and a peripheral muscular portion originating in the phrenic center itself.2 With regard to anatomic attachments, -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

Reconstruction of Complex Defects of the Extracranial Facial Nerve: Technique of “The Trifurcation Approach”
European Archives of Oto-Rhino-Laryngology (2019) 276:1793–1798 https://doi.org/10.1007/s00405-019-05418-4 HEAD AND NECK Reconstruction of complex defects of the extracranial facial nerve: technique of “the trifurcation approach” Dirk Beutner1 · Maria Grosheva2 Received: 28 January 2019 / Accepted: 31 March 2019 / Published online: 4 April 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Reconstruction of complex defects of facial nerve (FN) after extensive cancer surgery requires individualized solutions. We describe the trifurcation technique as a modifcation of the combined approach on example of two patients with locally advanced parotid cancer. Methods Due to perineural invasion, extensive resection of the FN from the mastoid segment to the peripheral branches was required. For reanimation of the upper face, a complex cervical plexus graft was sutured end-to-end to the mastoid segment of the FN trunk. The branches of the graft enabled reanimation of three peripheral temporal and zygomatic branches. The mandibular branch was sutured end-to-side to the hypoglossal nerve (hypoglossal–facial nerve transfer, HFNT). Addition- ally, the buccal branch was independently reanimated with ansa cervicalis. Results Facial reanimation was successful in both patients. Good resting tone and voluntary movement were achieved with a mild degree of synkinesis after 13 months. Patient 1 showed the Sunnybrook (SB) composite score 69 [76 (voluntary move- ment score) − 0 (resting symmetry score) − 7 (synkinesis score)]. In patient 2, the SB composite score was 76 (80 − 0 − 4, respectively). Conclusions In this trifurcation approach, cervical cutaneous plexus provides a long complex nerve graft, which allows bridging the gap between proximal FN stump and several peripheral branches without great expenditure. -
Comparative Study of Superficial Cervical Plexus Block and Nerve of Arnold Block with Intravenous Antiemetic Drugs Dexamethasone
Comparative Study of Superficial Cervical Plexus Block and Nerve of Arnold Block with Intravenous antiemetic drugs Dexamethasone and Ondansetron and Incidence of Post-operative Nausea Vomiting for Inner Ear Surgery Indiana University School of Medicine Riley Hospital for Children Principal Investigator: Malik Nouri, MD Co Investigator: Charles Yates, MD Version 2.0 Date: 01/27/2017 Page 1 of 12 Table of Contents: Study Schema 1.0 Background 2.0 Rationale and Specific Aims 3.0 Inclusion/Exclusion Criteria 4.0 Enrollment/Randomization 5.0 Study Procedures 6.0 Reporting of Adverse Events of Unanticipated Problems involving Risk to Participants or Others 7.0 Study Withdrawal/Discontinuation 8.0 Statistical Considerations 9.0 Privacy/Confidentiality Issues 10.0 Follow-up and Record Retention 11.0 Analysis of Results Page 2 of 12 1.0 Background Patients that undergo inner ear surgery often complain of postoperative nausea and vomiting (PONV) despite prophylactic antiemetic regiments with 5HT3 antagonists, steroids and vigorous hydration. Patients still experience this unpleasant feeling that may prolong hospital stay and can lead to nutritional issues such as dehydration and huge patient and family dissatisfaction. We would like to explore the use of regional anesthesia and potential antiemetic proprieties and compare it’s efficacy to the existing therapy. PONV is an unpleasant complication following anesthesia, it is well known that patients undergoing certain surgical procedures such as those involving the inner ear, the tympanomastoid cells, and the cochlear organ may be more prone to PONV. This complication can be anticipated in those instances and prophylactically treated with antiemetics, Vigorous hydration and cautious selection of anesthetic technique and avoidance of drugs known to promote nausea1, 2, 3. -

The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1
Open Access Review Article DOI: 10.7759/cureus.8697 The Five Diaphragms in Osteopathic Manipulative Medicine: Neurological Relationships, Part 1 Bruno Bordoni 1 1. Physical Medicine and Rehabilitation, Foundation Don Carlo Gnocchi, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract In osteopathic manual medicine (OMM), there are several approaches for patient assessment and treatment. One of these is the five diaphragm model (tentorium cerebelli, tongue, thoracic outlet, diaphragm, and pelvic floor), whose foundations are part of another historical model: respiratory-circulatory. The myofascial continuity, anterior and posterior, supports the notion the human body cannot be divided into segments but is a continuum of matter, fluids, and emotions. In this first part, the neurological relationships of the tentorium cerebelli and the lingual muscle complex will be highlighted, underlining the complex interactions and anastomoses, through the most current scientific data and an accurate review of the topic. In the second part, I will describe the neurological relationships of the thoracic outlet, the respiratory diaphragm and the pelvic floor, with clinical reflections. In literature, to my knowledge, it is the first time that the different neurological relationships of these anatomical segments have been discussed, highlighting the constant neurological continuity of the five diaphragms. Categories: Medical Education, Anatomy, Osteopathic Medicine Keywords: diaphragm, osteopathic, fascia, myofascial, fascintegrity, -

Mapping Sensory Nerve Communications Between Peripheral Nerve Territories
Clinical Anatomy 27:681–690 (2014) ORIGINAL COMMUNICATION Mapping Sensory Nerve Communications Between Peripheral Nerve Territories 1 2 1* ADIL LADAK, R. SHANE TUBBS, AND ROBERT J. SPINNER 1Department of Neurologic Surgery, Orthopedics and Anatomy, Mayo Clinic, Rochester, Minnesota 2Department of Neurosurgery, Children’s Hospital, Birmingham, Alabama The human cutaneous sensory map has been a work in progress over the past century, depicting sensory territories supplied by both the spinal and cranial nerves. Two critical discoveries, which shaped our understanding of cutaneous innervation, were sensory dermatome overlap between contiguous spinal levels and axial lines across areas where no sensory overlap exists. These concepts define current dermatome maps. We wondered whether the overlap between contiguous sensory territories was even tighter: if neural communications were present in the peripheral nerve territories consistently connecting contiguous spinal levels? A literature search using peer-reviewed articles and established anatomy texts was performed aimed at identifying the presence of communica- tions between sensory nerves in peripheral nerve territories and their relation- ship to areas of adjacent and non-adjacent spinal or cranial nerves and axial lines (lines of discontinuity) in the upper and lower limbs, trunk and perineum, and head and neck regions. Our findings demonstrate the consistent presence of sensory nerve communications between peripheral nerve territories derived from spinal nerves within areas of axial lines in the upper and lower limbs, trunk and perineum, and head and neck. We did not find examples of communications crossing axial lines in the limbs or lines of discontinuity in the face, but did find examples crossing axial lines in the trunk and perineum.