The Cervical Plexus by Prof
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Superficial (And Intermediate) Cervical Plexus Block
Superficial (and Intermediate) Cervical Plexus Block Indications: -Tympanomastoid surgery. When combined with the auricular branch of the vagus (‘nerve of arnold’) by infiltrating subcutaneously into the medial side of the tragus), obviates the need for opiates. -Pinnaplasty or Otoplasty -Lymph node excision (within the anterior and posterior triangles of the neck) -Clavicular surgery or fractures (may require intermediate cervical plexus block and its combination with interscalene block, see below) -Central Venous Catheters: Renal replacement therapy central venous catheters, tunnelled central venous catheters and portacaths inserted into the subclavian or jugular veins (may require combination with ‘Pecs 1’ block for component of pain below the clavicle) -Tracheostomy (see below discussion on safety profile of performing bilateral blocks and risks of respiratory distress due to phrenic nerve or recurrent largyngeal nerve block) -More commonly in adults: thyroid (again, bilateral) and carotid surgery Contraindications: -local sepsis or rash Anatomy: The cervical plexus arises from C1-C4 mixed spinal nerves (fig. 1): Somatic sensory branches: -arise from C2-C4 as the mixed spinal nerves leave the sulcus between the anterior and posterior tubercles of the transverse process (note C7 does not have an anterior tubercle or bifid spinous process): -pass between longus capitis and middle scalene perforating the prevertebral fascia. Note at C4 level the anterior scalene has largely disappeared having taken the bulk of its vertebral bony origin lower down. The bulkiest of the scalene muscles is the middle scalene and remains in view at this level: -then pass behind the internal jugular vein out into the potential space between the investing layer of deep fascia ensheathing the sternocleidomastoid, and the prevertebral layer of deep fascia covering levator scapulae (fig. -
33. Spinal Nerves. Cervical Plexus
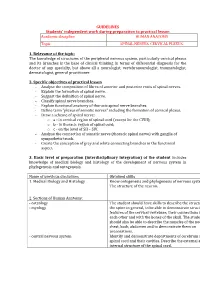
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Unusual Organization of the Ansa Cervicalis: a Case Report
CASE REPORT ISSN- 0102-9010 UNUSUAL ORGANIZATION OF THE ANSA CERVICALIS: A CASE REPORT Ranjana Verma1, Srijit Das2 and Rajesh Suri3 Department of Anatomy, Maulana Azad Medical College, New Delhi-110002, India. ABSTRACT The superior root of the ansa cervicalis is formed by C1 fibers carried by the hypoglossal nerve, whereas the inferior root is contributed by C2 and C3 nerves. We report a rare finding in a 40-year-old male cadaver in which the vagus nerve fused with the hypoglossal nerve immediately after its exit from the skull on the left side. The vagus nerve supplied branches to the sternohyoid, sternothyroid and superior belly of the omohyoid muscles and also contributed to the formation of the superior root of the ansa cervicalis. In this arrangement, paralysis of the infrahyoid muscles may result following lesion of the vagus nerve anywhere in the neck. The cervical location of the vagus nerve was anterior to the common carotid artery within the carotid sheath. This case report may be of clinical interest to surgeons who perform laryngeal reinnervation and neurologists who diagnose nerve disorders. Key words: Ansa cervicalis, hypoglossal nerve, vagus nerve, variations INTRODUCTION cadaver. The right side was normal. The neck region The ansa cervicalis is a nerve loop formed was dissected and the neural structures in the carotid by the union of superior and inferior roots. The and muscular triangle regions were exposed, with superior root is a branch of the hypoglossal nerve particular attention given to the organization of the containing C1 fibers, whereas the inferior root is ansa cervicalis. -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -

Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2
Open Access Review Article DOI: 10.7759/cureus.5679 Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2 Bruno Bordoni 1 , Marta Simonelli 2 , Maria Marcella Lagana 3 1. Cardiology, Foundation Don Carlo Gnocchi, Milan, ITA 2. Osteopathy, French-Italian School of Osteopathy, Pisa, ITA 3. Radiology, IRCCS Fondazione Don Carlo Gnocchi Onlus, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract The tentorium cerebelli is a meningeal portion in relation to the skull, the nervous system, and the cervical tract. In this second part, the article discusses the systematic tentorial relationships, such as the central and cervical neurological connections, the venous circulation and highlights possible clinical alterations that could cause pain. To understand the function of anatomy, we should always remember that every area of the human body is never a segment, but a functional continuum. Categories: Physical Medicine & Rehabilitation, Anatomy, Osteopathic Medicine Keywords: tentorium cerebelli, fascia, pain, venous circulation, neurological connections, cranio Introduction And Background Cervical neurological connections The ansa cervicalis characterizes the first cervical roots and connects all anterior cervical nerve exits with the inferior floor of the oral cavity, the trigeminal system, the respiratory control system, and the sympathetic system. The descending branch of the hypoglossal nerve anastomoses with C1, forming the ansa hypoglossi or ansa cervicalis superior [1]. The inferior root of the ansa cervicalis, also known as descendens cervicalis, is formed by ascendant fibers from spinal nerves C2-C3 and occasionally fibers C4, lying anteriorly to the common carotid artery (it passes laterally or medially to the internal jugular vein upon anatomical variations) [1]. -
The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -

Human Anatomy
Human Anatomy د.فراس عبد الرحمن Lec.13 The neck Overview The neck is the area of the body between the base of the cranium superiorly and the suprasternal notch and the clavicles inferiorly. The neck joins the head to the trunk and limbs, serving as a major conduit for structures passing between them. Many important structures are crowded together in the neck, such as muscles, arteries, veins, nerves, lymphatics, thyroid and parathyroid glands, trachea, larynx, esophagus, and vertebrae. Carotid/jugular blood vessels are the major structures commonly injured in penetrating wounds of the neck. The brachial plexuses of nerves originate in the neck and pass inferolaterally to enter the axillae and continue to supply the upper limbs. Lymph from structures in the head and neck drains into cervical lymph nodes. Skin of the Neck The natural lines of cleavage of the skin (Wrinkle lines) are constant and run almost horizontally around the neck. This is important clinically because an incision along a cleavage line will heal as a narrow scar, whereas one that crosses the lines will heal as a wide or heaped-up scar. Fasciae of the Neck The neck is surrounded by a superficial cervical fascia that lies deep to the skin and invests the platysma muscle (a muscle of facial expression). A second deep cervical fascia tightly invests the neck structures and is divided into three layers. Superficial Cervical Fascia The superficial fascia of the neck forms a thin layer that encloses the platysma muscle. Also embedded in it are the cutaneous nerves, the superficial veins, and the superficial lymph nodes. -

Protection of Supraclavicular Nerve in the Surgical Procedures of Clavicle Fracture Fixation
Protection of Supraclavicular Nerve in the Surgical Procedures of Clavicle Fracture Fixation Abulaiti Abula First Aliated Hospital of Xinjiang Medical University Yanshi Liu First Aliated Hospital of Xinjiang Medical University Kai Liu First Aliated Hospital of Xinjiang Medical University Feiyu Cai First Aliated Hospital of Xinjiang Medical University Alimujiang Abulaiti First Aliated Hospital of Xinjiang Medical University Xiayimaierdan Maimaiti First Aliated Hospital of Xinjiang Medical University Peng Ren First Aliated Hospital of Xinjiang Medical University Aihemaitijiang yusufu ( [email protected] ) First Aliated Hospital of Xinjiang Medical University Research Article Keywords: Clavicle fracture, Open reduction and internal xation, Supraclavicular nerve injury Posted Date: May 27th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-549126/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/13 Abstract Background: The present study was to evaluate the clinical effectiveness of the protection of the supraclavicular nerve in the treatment of clavicle fracture using fracture reduction and percutaneous external locking plate xation or open reduction and internal xation (ORIF). Methods: A total of 27 patients suffered clavicle fracture and underwent fracture reduction and external or internal xation with reserved clavicular epithelial nerve in our department from January 2015 to January 2020 were retrospectively collected, including 19 males and 8 females with a mean age of 42 years (range 21 to 57 years). Among them, 17 patients were treated with the fracture reduction and percutaneous external locking plate xation, while the other 10 patients were treated with ORIF. The sensory function of the affected shoulder area and the superior lateral thoracic area after surgery was collected and analyzed, as well as the satisfaction rate after the xation was removed. -

A Comprehensive Review of Anatomy and Regional Anesthesia Techniques of Clavicle Surgeries
vv ISSN: 2641-3116 DOI: https://dx.doi.org/10.17352/ojor CLINICAL GROUP Received: 31 March, 2021 Research Article Accepted: 07 April, 2021 Published: 10 April, 2021 *Corresponding author: Dr. Kartik Sonawane, Uncovering secrets of the Junior Consultant, Department of Anesthesiol- ogy, Ganga Medical Centre & Hospitals, Pvt. Ltd. Coimbatore, Tamil Nadu, India, E-mail: beauty bone: A comprehensive Keywords: Clavicle fractures; Floating shoulder sur- gery; Clavicle surgery; Clavicle anesthesia; Procedure review of anatomy and specific anesthesia; Clavicular block regional anesthesia techniques https://www.peertechzpublications.com of clavicle surgeries Kartik Sonawane1*, Hrudini Dixit2, J.Balavenkatasubramanian3 and Palanichamy Gurumoorthi4 1Junior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 2Fellow in Regional Anesthesia, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 3Senior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 4Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India Abstract The clavicle is the most frequently fractured bone in humans. General anesthesia with or without Regional Anesthesia (RA) is most frequently used for clavicle surgeries due to its complex innervation. Many RA techniques, alone or in combination, have been used for clavicle surgeries. These include interscalene block, cervical plexus (superficial and deep) blocks, SCUT (supraclavicular nerve + selective upper trunk) block, and pectoral nerve blocks (PEC I and PEC II). The clavipectoral fascial plane block is also a safe and simple option and replaces most other RA techniques due to its lack of side effects like phrenic nerve palsy or motor block of the upper limb. -

Communications of Transverse Cervical Cutaneous Nerve with the Cervical Branch of Facial Nerve and Its Variant Nerve Endings
ogy: iol Cu ys r h re P n t & R y e s Anatomy & Physiology: Current m e Sirasanagandla et al., Anatom Physiol 2013, 3:1 o a t r a c n h DOI: 10.4172/2161-0940.1000114 A Research ISSN: 2161-0940 Case Report Open Access Communications of Transverse Cervical Cutaneous Nerve with the Cervical Branch of Facial Nerve and its Variant Nerve Endings Deep in the Parotid Gland Srinivasa Rao Sirasanagandla*, Swamy Ravindra S, Sapna Marpalli and Satheesha Nayak B Department of Anatomy, Melaka Manipal Medical College, Manipal University, Madhav Nagar, Manipal, Karnataka, India Abstract Anastomoses between the transverse cervical cutaneous nerve and the cervical branch of facial nerve are regularly present. The anatomic locations of these anastomoses were poorly documented in the literature. During regular dissection, we came across two of such anastomoses: one of the two anastomoses was identified posterior to submandibular gland, and the other was noted within the parenchyma of the parotid gland. Prior knowledge of anatomic locations of these anastomoses is clinically important as it allows a method for identification and preservation of the cervical branch of the facial nerve as well as a starting point for retrograde facial nerve dissections. In addition, few terminal nerve endings of transverse cervical cutaneous nerve were seen along the retromandibular vein, ducts and some were penetrating the interlobular septa of parotid gland. The functional significance of anatomic variations of its nerve terminal ends deep in the gland is yet to be evaluated. Keywords: Anastomoses; Transverse cervical cutaneous nerve; (TCCN) and supraclavicular nerves pierce the fascia to supply the skin. -

A Source of Complication in Vagus Nerve Stimulation
PEDIATRICS CASE REPORT J Neurosurg Pediatr 15:535–538, 2015 The “vagal ansa”: a source of complication in vagus nerve stimulation Chittur Viswanathan Gopalakrishnan, MS, MCh,1 John R. W. Kestle, MD,1 and Mary B. Connolly, MB, FRCP(C)2 1Division of Neurosurgery, Department of Surgery, University of British Columbia and BC Children’s Hospital; and 2Division of Neurology, Department of Paediatrics, University of British Columbia and BC Children’s Hospital, Vancouver, British Columbia, Canada A 16-year-old boy underwent vagus nerve stimulation for treatment-resistant multifocal epilepsy. During intraoperative system diagnostics, vigorous contraction of the ipsilateral sternomastoid muscle was observed. On re-exploration, a thin nerve fiber passing from the vagus to the sternomastoid was found hooked up in the upper electrode. Detailed inspec- tion revealed an abnormal course of the superior root of the ansa cervicalis, which descended down as a single nerve trunk with the vagus and separated to join the inferior root. The authors discuss the variation in the course of the ansa cervicalis and how this could be a reason for postoperative neck muscle contractions. http://thejns.org/doi/abs/10.3171/2014.10.PEDS14259 KEY WORDS ansa cervicalis; variation; vagus nerve stimulation; epilepsy; complication; peripheral nerve HE ansa cervicalis, located in the anterior triangle of We describe an intraoperative complication noticed the neck, is formed by the anterior rami of the first during testing of the VNS system after placement of the 3 or 4 cervical spinal nerves. This nerve loop in- electrodes and the pulse generator. To the best of our Tnervates the infrahyoid muscles.5 It is frequently encoun- knowledge, it has not been previously reported. -

Reconstruction of Complex Defects of the Extracranial Facial Nerve: Technique of “The Trifurcation Approach”
European Archives of Oto-Rhino-Laryngology (2019) 276:1793–1798 https://doi.org/10.1007/s00405-019-05418-4 HEAD AND NECK Reconstruction of complex defects of the extracranial facial nerve: technique of “the trifurcation approach” Dirk Beutner1 · Maria Grosheva2 Received: 28 January 2019 / Accepted: 31 March 2019 / Published online: 4 April 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Reconstruction of complex defects of facial nerve (FN) after extensive cancer surgery requires individualized solutions. We describe the trifurcation technique as a modifcation of the combined approach on example of two patients with locally advanced parotid cancer. Methods Due to perineural invasion, extensive resection of the FN from the mastoid segment to the peripheral branches was required. For reanimation of the upper face, a complex cervical plexus graft was sutured end-to-end to the mastoid segment of the FN trunk. The branches of the graft enabled reanimation of three peripheral temporal and zygomatic branches. The mandibular branch was sutured end-to-side to the hypoglossal nerve (hypoglossal–facial nerve transfer, HFNT). Addition- ally, the buccal branch was independently reanimated with ansa cervicalis. Results Facial reanimation was successful in both patients. Good resting tone and voluntary movement were achieved with a mild degree of synkinesis after 13 months. Patient 1 showed the Sunnybrook (SB) composite score 69 [76 (voluntary move- ment score) − 0 (resting symmetry score) − 7 (synkinesis score)]. In patient 2, the SB composite score was 76 (80 − 0 − 4, respectively). Conclusions In this trifurcation approach, cervical cutaneous plexus provides a long complex nerve graft, which allows bridging the gap between proximal FN stump and several peripheral branches without great expenditure.