Comparative Study of Superficial Cervical Plexus Block and Nerve of Arnold Block with Intravenous Antiemetic Drugs Dexamethasone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Superficial (And Intermediate) Cervical Plexus Block
Superficial (and Intermediate) Cervical Plexus Block Indications: -Tympanomastoid surgery. When combined with the auricular branch of the vagus (‘nerve of arnold’) by infiltrating subcutaneously into the medial side of the tragus), obviates the need for opiates. -Pinnaplasty or Otoplasty -Lymph node excision (within the anterior and posterior triangles of the neck) -Clavicular surgery or fractures (may require intermediate cervical plexus block and its combination with interscalene block, see below) -Central Venous Catheters: Renal replacement therapy central venous catheters, tunnelled central venous catheters and portacaths inserted into the subclavian or jugular veins (may require combination with ‘Pecs 1’ block for component of pain below the clavicle) -Tracheostomy (see below discussion on safety profile of performing bilateral blocks and risks of respiratory distress due to phrenic nerve or recurrent largyngeal nerve block) -More commonly in adults: thyroid (again, bilateral) and carotid surgery Contraindications: -local sepsis or rash Anatomy: The cervical plexus arises from C1-C4 mixed spinal nerves (fig. 1): Somatic sensory branches: -arise from C2-C4 as the mixed spinal nerves leave the sulcus between the anterior and posterior tubercles of the transverse process (note C7 does not have an anterior tubercle or bifid spinous process): -pass between longus capitis and middle scalene perforating the prevertebral fascia. Note at C4 level the anterior scalene has largely disappeared having taken the bulk of its vertebral bony origin lower down. The bulkiest of the scalene muscles is the middle scalene and remains in view at this level: -then pass behind the internal jugular vein out into the potential space between the investing layer of deep fascia ensheathing the sternocleidomastoid, and the prevertebral layer of deep fascia covering levator scapulae (fig. -
33. Spinal Nerves. Cervical Plexus
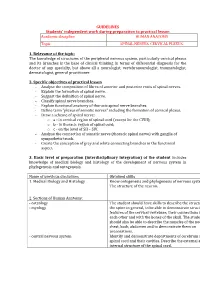
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -

The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -

Reconstruction of Complex Defects of the Extracranial Facial Nerve: Technique of “The Trifurcation Approach”
European Archives of Oto-Rhino-Laryngology (2019) 276:1793–1798 https://doi.org/10.1007/s00405-019-05418-4 HEAD AND NECK Reconstruction of complex defects of the extracranial facial nerve: technique of “the trifurcation approach” Dirk Beutner1 · Maria Grosheva2 Received: 28 January 2019 / Accepted: 31 March 2019 / Published online: 4 April 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Reconstruction of complex defects of facial nerve (FN) after extensive cancer surgery requires individualized solutions. We describe the trifurcation technique as a modifcation of the combined approach on example of two patients with locally advanced parotid cancer. Methods Due to perineural invasion, extensive resection of the FN from the mastoid segment to the peripheral branches was required. For reanimation of the upper face, a complex cervical plexus graft was sutured end-to-end to the mastoid segment of the FN trunk. The branches of the graft enabled reanimation of three peripheral temporal and zygomatic branches. The mandibular branch was sutured end-to-side to the hypoglossal nerve (hypoglossal–facial nerve transfer, HFNT). Addition- ally, the buccal branch was independently reanimated with ansa cervicalis. Results Facial reanimation was successful in both patients. Good resting tone and voluntary movement were achieved with a mild degree of synkinesis after 13 months. Patient 1 showed the Sunnybrook (SB) composite score 69 [76 (voluntary move- ment score) − 0 (resting symmetry score) − 7 (synkinesis score)]. In patient 2, the SB composite score was 76 (80 − 0 − 4, respectively). Conclusions In this trifurcation approach, cervical cutaneous plexus provides a long complex nerve graft, which allows bridging the gap between proximal FN stump and several peripheral branches without great expenditure. -

Mapping Sensory Nerve Communications Between Peripheral Nerve Territories
Clinical Anatomy 27:681–690 (2014) ORIGINAL COMMUNICATION Mapping Sensory Nerve Communications Between Peripheral Nerve Territories 1 2 1* ADIL LADAK, R. SHANE TUBBS, AND ROBERT J. SPINNER 1Department of Neurologic Surgery, Orthopedics and Anatomy, Mayo Clinic, Rochester, Minnesota 2Department of Neurosurgery, Children’s Hospital, Birmingham, Alabama The human cutaneous sensory map has been a work in progress over the past century, depicting sensory territories supplied by both the spinal and cranial nerves. Two critical discoveries, which shaped our understanding of cutaneous innervation, were sensory dermatome overlap between contiguous spinal levels and axial lines across areas where no sensory overlap exists. These concepts define current dermatome maps. We wondered whether the overlap between contiguous sensory territories was even tighter: if neural communications were present in the peripheral nerve territories consistently connecting contiguous spinal levels? A literature search using peer-reviewed articles and established anatomy texts was performed aimed at identifying the presence of communica- tions between sensory nerves in peripheral nerve territories and their relation- ship to areas of adjacent and non-adjacent spinal or cranial nerves and axial lines (lines of discontinuity) in the upper and lower limbs, trunk and perineum, and head and neck regions. Our findings demonstrate the consistent presence of sensory nerve communications between peripheral nerve territories derived from spinal nerves within areas of axial lines in the upper and lower limbs, trunk and perineum, and head and neck. We did not find examples of communications crossing axial lines in the limbs or lines of discontinuity in the face, but did find examples crossing axial lines in the trunk and perineum. -

The Cervical Plexus by Prof
The Cervical Plexus By Prof. Dr. Imran Qureshi The Cervical Plexus is formed by the ventral rami of C1, C2, C3, and C4. It supplies: o Areas of the Skin o The Respiratory Diaphragm o The Strap muscles of the Anterior Triangle of the Neck, and o The nerves to The Sternocleidomastoid, Trapezius, Scalenes, Levator Scapulae, Longus Coli, Longus Capitis etc. I. Branches to the Skin: These appear in the posterior triangle at the midpoint of the posterior border of the sternocleidomastoid. They are: The Greater Auricular Nerve, which crosses the Sternocleidomastoid obliquely, posterior to the external jugular vein and ascends toward the lobe of the ear, Lesser Occipital Nerve, which parallels the posterior border of Sternocleidomastoid and ascends toward the occipital region, Anterior Cutaneous (Transverse Cervical) Nerve, which crosses transversely across the Sternocleidomastoid to reach the skin of the anterior triangle of the neck, The Supraclavicular trunk, which passes from under cover of the Sternocleidomastoid and divides into: The Lateral supraclavicular nerve, The Intermediate supraclavicular nerve, and The Medial supraclavicular nerve. The Lateral supraclavicular passes superficial to the trapezius to supply the skin of the shoulder tip. The Intermediate and Medial supraclavicular nerves pass superficial to the clavicle to the skin of the pectoral region. 1 II. Nerve to Respiratory Diaphragm (Phrenic Nerve): This nerve, which arises from the ventral rami of C3, C4, and C5, is the motor nerve of the diaphragm. It also supplies sensory fibers, including pain, to the central area. The contribution from C5 may join that from C3 and C4 directly, or secondarily as a branch from the nerve to the subclavius muscle. -

Cervical Plexus Block
Review Article pISSN 2005-6419 • eISSN 2005-7563 KJA Cervical plexus block Korean Journal of Anesthesiology Jin-Soo Kim1, Justin Sangwook Ko2, Seunguk Bang3, Hyungtae Kim4, and Sook Young Lee1 Department of Anesthesiology and Pain Medicine, 1Ajou University College of Medicine, Suwon, 2Samsung Medical Center, Sungkyunkwan University College of Medicine, 3Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, 4Presbyterian Medical Center, Jeonju, Korea Cervical plexus blocks (CPBs) have been used in various head and neck surgeries to provide adequate anesthesia and/ or analgesia; however, the block is performed in a narrow space in the region of the neck that contains many sensitive structures, multiple fascial layers, and complicated innervation. Since the intermediate CPB was introduced in addition to superficial and deep CPBs in 2004, there has been some confusion regarding the nomenclature and definition of CPBs, particularly the intermediate CPB. Additionally, as the role of ultrasound in the head and neck region has expanded, CPBs can be performed more safely and accurately under ultrasound guidance. In this review, the authors will describe the methods, including ultrasound-guided techniques, and clinical applications of conventional deep and superficial CPBs; in addition, the authors will discuss the controversial issues regarding intermediate CPBs, including nomenclature and associated potential adverse effects that may often be neglected, focusing on the anatomy of the cervical fascial layers and cervical plexus. Finally, the authors will attempt to refine the classification of CPB methods based on the target com- partments, which can be easily identified under ultrasound guidance, with consideration of the effects of each method of CPB. -
Text Preview
ix Introduction ANATOMY . IS THE VESTIBULE OF THE TEMPLE OF MEDICAL SCIENCE. —DE LINT, 19261 The ability to perform dissection provides a unique opportunity to observe the intricate in- terplay of human structure. This is especially true if the student is able to participate in an anatomy laboratory in which several (or many) different cadavers are located. A consistent theme in the treatises of early anatomists is awe and wonder at the incredible complexity and variety of the human organism. This unique and special opportunity was not always available to aspiring students. Imagine the difficulty of performing studious dissection before the development of effective embalm- ing or refrigeration, for example. Anatomists traveled from town to town to study from “fresh” bodies that had not yet begun to decay. To compound matters, dissection of human bodies sometimes happened in secret, in closed rooms and furtively at night. For more than 4000 years, we have sought to determine the structure and function of the human body. Chinese writings and drawings from about 2500 BCE describe circulation, breathing, and many internal organs.2 Around 1600 BCE, Egyptians recorded that the blood vessels were known to come from the heart, and these early anatomists recognized the liver, spleen, kidneys, uterus, and bladder.2 Hindu medicine dating from 600 BCE contains refer- ences to the skeleton and advanced surgical procedures.2 In the third and fourth centuries BCE, Hippocrates, Aristotle, and their followers compiled observations about the musculoskeletal system and organs. Most of these were made by com- bining external observation with conjecture based on the dissection of nonhuman animals.2 Herophilus and Erasistratus, working as surgeons in Alexandria in approximately 300 BCE, made systematic studies designed to discover the workings of human anatomy.2 However, the most influential anatomist of ancient times was, perhaps, Galen. -

58225-A-Rare-Anatomical-Variation-Of-The-Lesser-Occipital-Nerve.Pdf
Open Access Case Report DOI: 10.7759/cureus.15901 A Rare Anatomical Variation of the Lesser Occipital Nerve A. Bert Chabot 1 , Joe Iwanaga 1 , Aaron S. Dumont 1 , R. Shane Tubbs 2, 3, 4 1. Department of Neurosurgery, Tulane University School of Medicine, New Orleans, USA 2. Anatomical Sciences, St. George's University, St. George's, GRD 3. Department of Neurosurgery and Structural & Cellular Biology, Tulane University School of Medicine, New Orleans, USA 4. Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, USA Corresponding author: Joe Iwanaga, [email protected] Abstract The lesser occipital nerve (LON) is a cutaneous branch of the cervical plexus that arises from the second and sometimes the third spinal nerve and innervates the scalp. During routine dissection of the neck, the LON was observed to arise directly from the spinal accessory nerve. The aberrant nerve measured 1.9 mm in diameter and 10.2 cm in length. Although anatomical variations of the LON such as duplication and triplication have been observed, we believe the origination of this nerve directly and exclusively from the spinal accessory nerve is exceedingly rare. The current case adds to the sparse literature on the variations of the LON and might be of interest to clinicians treating neurological conditions or surgeons operating in the area. Categories: Anatomy Keywords: lesser occipital nerve, variation, cadaver, clinical anatomy, spinal accessory nerve Introduction The lesser occipital nerve (LON) is a cutaneous branch of the cervical plexus and arises from the ventral rami of the second and sometimes the third cervical nerve [1,2]. -

Plexopathy/ Radiculopathy
Plexopathy/ Radiculopathy Holli A. Horak, MD University of Arizona August 2015 Radiculopathy/ Plexopathy Radiculopathy Plexopathy Common pathology Much less common Common referral to High Index of EMG laboratory suspicion • Referral may not mention plexopathy Anatomy • “shoulder pain” Pathology Special tests/study NCS/EMG findings design needed Plexopathy/ Radiculopathy Definition • Plexopathy Distal to the ventral primary rami Distal to the DRG Proximal to the individual nerve • Radiculopathy Proximal to split of dorsal/ventral rami Proximal to DRG EMG/NCS correlation Radiculopathy Plexopathy Abnormalities in Motor Multiple motor nerves nerves supplied by affected that nerve root level • All peripheral nerves distal to plexus lesion S1 radiculopathy Tibial nerve SNAPS affected • Lesion is distal to DRG Normal SNAP waveform • Lesion proximal to DRG Anatomy: Cervical Plexus: R-T-D-C-B Roots: C5-6-7-8-T1 Trunks:Upper, middle, lower Divisions:3 anterior and 3 posterior Cords:Lateral, Posterior, medial Branches: • Musculocutaneous, Median nerves • Axillary, Radial nerves • Ulnar, Median nerves Stylized Brachial Plexus Anatomy: Lumbar Plexus Ventral Rami L1-2-3-4 spinal nerves Anterior and posterior divisions • Posterior: Femoral nerve L2-3-4 • Anterior: Obturator nerve L2-3-4 Lumbosacral trunk: • L4 (some) and L5 ventral rami Connect to sacral plexus Anatomy: Sacral plexus Ventral Rami: S1-2-3-4 • Plus Lumbosacral trunk (L4-5) Anterior and Posterior divisions • Anterior: Tibial nerve L4-5-S1-2 • Posterior: -

Three-Component Model of the Spinal Nerve Branching Pattern, Based on the View of the Lateral Somitic Frontier and Experimental Validation
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.29.227710; this version posted July 30, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Three-Component Model of the Spinal Nerve Branching Pattern, based on the View of the Lateral Somitic Frontier and Experimental Validation Shunsaku Homma1*, Takako Shimada1, Ikuo Wada2, Katsuji Kumaki3, Noboru Sato3, and Hiroyuki Yaginuma1 1 Department of Neuroanatomy and Embryology, 2 Department of Cell Science, Institute of Biomedical Sciences, Fukushima Medical University, 1 Hikarigaoka, Fukushima, 960-1295 JAPAN 3 Division of Gross Anatomy and Morphogenesis, Niigata University Graduate School of Medical and Dental Sciences, Niigata, 951-8510 JAPAN * Corresponding author: S. Homma, [email protected]. bioRxiv preprint doi: https://doi.org/10.1101/2020.07.29.227710; this version posted July 30, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. ABSTRACT One of the decisive questions about human gross anatomy is unmatching the adult branching pattern of the spinal nerve to the embryonic lineages of the peripheral target muscles. The two principal branches in the adult anatomy, the dorsal and ventral rami of the spinal nerve, innervate the intrinsic back muscles (epaxial muscles), as well as the body wall and appendicular muscles (hypaxial muscles), respectively. However, progenitors from the dorsomedial myotome develop into the back and proximal body wall muscles (primaxial muscles) within the sclerotome-derived connective tissue environment.