Three-Component Model of the Spinal Nerve Branching Pattern, Based on the View of the Lateral Somitic Frontier and Experimental Validation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Netter's Musculoskeletal Flash Cards, 1E
Netter’s Musculoskeletal Flash Cards Jennifer Hart, PA-C, ATC Mark D. Miller, MD University of Virginia This page intentionally left blank Preface In a world dominated by electronics and gadgetry, learning from fl ash cards remains a reassuringly “tried and true” method of building knowledge. They taught us subtraction and multiplication tables when we were young, and here we use them to navigate the basics of musculoskeletal medicine. Netter illustrations are supplemented with clinical, radiographic, and arthroscopic images to review the most common musculoskeletal diseases. These cards provide the user with a steadfast tool for the very best kind of learning—that which is self directed. “Learning is not attained by chance, it must be sought for with ardor and attended to with diligence.” —Abigail Adams (1744–1818) “It’s that moment of dawning comprehension I live for!” —Calvin (Calvin and Hobbes) Jennifer Hart, PA-C, ATC Mark D. Miller, MD Netter’s Musculoskeletal Flash Cards 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 NETTER’S MUSCULOSKELETAL FLASH CARDS ISBN: 978-1-4160-4630-1 Copyright © 2008 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers. Permissions for Netter Art figures may be sought directly from Elsevier’s Health Science Licensing Department in Philadelphia PA, USA: phone 1-800-523-1649, ext. 3276 or (215) 239-3276; or e-mail [email protected]. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Anterior Abdominal Wall (Continue)
Anterior rami (T7 – L1) . T7-T11 called intercostal nerves. T12 called subcostal nerve. L1 through lumber plexus i.e. ilio inguinal & ilio hypogastric nerves T7……. Epigastrum T10……Umblicus L1…Above inguinal ligament & symphysis pubis. Arterial: Upper mid line: superior epigastric artery (internal thoracic artery). Lower mid line: inferior epigastric artery (external iliac artery). Flanks: supplied by branches from intercostal artery, lumbar artery & deep circumflex iliac artery. Venous: all venous blood collected into a plexus of veins that radiate from umbilicus toward: : Above : to lateral thoracic vein then to axillary vein. Below : to superficial epigastric & greater saphenous veins then to femoral vein. Lymphatic Of Anterior abdominal Wall: Above umbilicus : drain into anterior axillary lymph nodes. Below umbilicus: drain in to superficial inguinal nodes 1)External oblique muscle. 2) Internal oblique muscle. 3) Transversus abdominis 4)Rectus abdominis. 5) Pyramidalis. Origin: The outer surface of lower 8 ribs then directed forward & downward to its insertion. Upper four slip interdigitate with seratus anterior muscle. Lower four slip interdigitate with latissimus dorsi muscle . Insertions: As a flat aponeurosis into: * Xiphoid process. * Linea alba * Pubic crest. * Pubic tubercle. * Anterior half of iliac crest . Internal Oblique Muscle: Origin : * Lumber fascia * Anterior 2/3 of iliac crest. * Lateral 2/3 of inguinal ligament. Insertion: The fibers passes upward & foreword & inserted to lower 3 ribs & their costal cartilages, xiphoid process, linea alba & symphysis pubis. Conjoint Tendon: Form from lower tendon of internal oblique joined to similar tendon from transversus abdominis . Its is attached medially to linea alba ,pubic crest & pectineal line but has a lateral free border. The spermatic cord, as it passes below this muscle, it gains a muscular cover called " Cremaster muscle " which composed of muscle & fascia. -

Scapular Winging Is a Rare Disorder Often Caused by Neuromuscular Imbalance in the Scapulothoracic Stabilizer Muscles
SCAPULAR WINGING Scapular winging is a rare disorder often caused by neuromuscular imbalance in the scapulothoracic stabilizer muscles. Lesions of the long thoracic nerve and spinal accessory nerves are the most common cause. Patients report diffuse neck, shoulder girdle, and upper back pain, which may be debilitating, associated with abduction and overhead activities. Accurate diagnosis and detection depend on appreciation on comprehensive physical examination. Although most cases resolve nonsurgically, surgical treatment of scapular winging has been met with success. True incidence is largely unknown because of under diagnosis. Most commonly it is categorized anatomically as medial or lateral shift of the inferior angle of the scapula. Primary winging occurs when muscular weakness disrupts the normal balance of the scapulothoracic complex. Secondary winging occurs when pathology of the shoulder joint pathology. Delay in diagnosis may lead to traction brachial plexopathy, periscapular muscle spasm, frozen shoulder, subacromial impingement, and thoracic outlet syndrome. Anatomy and Biomechanics Scapula is rotated 30° anterior on the chest wall; 20° forward in the sagittal plane; the inferior angle is tilted 3° upward. It serves as the attachment site for 17 muscles. The trapezius muscle accomplishes elevation of the scapula in the cranio-caudal axis and upward rotation. The serratus anterior and pectoralis major and minor muscles produce anterior and lateral motion, described as scapular protraction. Normal Scapulothoracic abduction: As the limb is elevated, the effect is an upward and lateral rotation of the inferior pole of scapula. Periscapular weakness resulting from overuse may manifest as scapular dysfunction (ie, winging). Serratus Anterior Muscle Origin From the first 9 ribs Insert The medial border of the scapula. -

Thoracic Outlet and Pectoralis Minor Syndromes
S EMINARS IN V ASCULAR S URGERY 27 (2014) 86– 117 Available online at www.sciencedirect.com www.elsevier.com/locate/semvascsurg Thoracic outlet and pectoralis minor syndromes n Richard J. Sanders, MD , and Stephen J. Annest, MD Presbyterian/St. Luke's Medical Center, 1719 Gilpin, Denver, CO 80218 article info abstract Compression of the neurovascular bundle to the upper extremity can occur above or below the clavicle; thoracic outlet syndrome (TOS) is above the clavicle and pectoralis minor syndrome is below. More than 90% of cases involve the brachial plexus, 5% involve venous obstruction, and 1% are associate with arterial obstruction. The clinical presentation, including symptoms, physical examination, pathology, etiology, and treatment differences among neurogenic, venous, and arterial TOS syndromes. This review details the diagnostic testing required to differentiate among the associated conditions and recommends appropriate medical or surgical treatment for each compression syndrome. The long- term outcomes of patients with TOS and pectoralis minor syndrome also vary and depend on duration of symptoms before initiation of physical therapy and surgical intervention. Overall, it can be expected that 480% of patients with these compression syndromes can experience functional improvement of their upper extremity; higher for arterial and venous TOS than for neurogenic compression. & 2015 Published by Elsevier Inc. 1. Introduction compression giving rise to neurogenic TOS (NTOS) and/or neurogenic PMS (NPMS). Much less common is subclavian Compression of the neurovascular bundle of the upper and axillary vein obstruction giving rise to venous TOS (VTOS) extremity can occur above or below the clavicle. Above the or venous PMS (VPMS). -

Netter's Anatomy Flash Cards – Section 7 – List 4Th Edition
Netter's Anatomy Flash Cards – Section 7 – List 4th Edition https://www.memrise.com/course/1577594/ Section 7 Lower Limb (72 cards) Plate 7-1 Hip (Coxal) Bone: Lateral View 1.1 Posterior superior iliac spine 1.2 Posterior inferior iliac spine 1.3 Greater sciatic notch 1.4 Body of ilium 1.5 Body of ischium 1.6 Ischial tuberosity 1.7 Pubic tubercle 1.8 Acetabulum 1.9 Iliac crest Plate 7-2 Hip (Coxal) Bone: Medial View 2.1 Wing (ala) of ilium (iliac fossa) 2.2 Pecten pubis (pectineal line) 2.3 Ramus of ischium 2.4 Lesser sciatic notch 2.5 Ischial spine 2.6 Articular surface (for sacrum) 2.7 Iliac tuberosity Plate 7-3 Hip Joint: Lateral View 3.1 Lunate (articular) surface of acetabulum 3.2 Articular cartilage 3.3 Head of femur 3.4 Ligament of head of femur (cut) 3.5 Obturator membrane 3.6 Acetabular labrum (fibrocartilaginous) Plate 7-4 Hip Joint: Anterior and Posterior Views 4.1 Iliofemoral ligament (Y ligament of Bigelow) 4.2 Pubofemoral ligament 4.3 Iliofemoral ligament 4.4 Ischiofemoral ligament Plate 7-5 Femur 5.1 Greater trochanter 5.2 Shaft (body) 5.3 Lateral epicondyle 5.4 Lateral condyle 5.5 Medial condyle 5.6 Medial epicondyle 5.7 Adductor tubercle 5.8 Linea aspera (Medial lip; Lateral lip) 5.9 Lesser trochanter 5.10 Intertrochanteric crest 5.11 Neck 5.12 Head Plate 7-6 Tibia and Fibula 6.1 Lateral condyle 6.2 Apex, Head, and Neck of fibula 6.3 Fibula 6.4 Lateral malleolus 6.5 Medial malleolus 6.6 Tibia 6.7 Tibial tuberosity 6.8 Medial condyle 6.9 Superior articular surfaces (medial and lateral facets) 6.10 Malleolar fossa of lateral -

Superficial (And Intermediate) Cervical Plexus Block
Superficial (and Intermediate) Cervical Plexus Block Indications: -Tympanomastoid surgery. When combined with the auricular branch of the vagus (‘nerve of arnold’) by infiltrating subcutaneously into the medial side of the tragus), obviates the need for opiates. -Pinnaplasty or Otoplasty -Lymph node excision (within the anterior and posterior triangles of the neck) -Clavicular surgery or fractures (may require intermediate cervical plexus block and its combination with interscalene block, see below) -Central Venous Catheters: Renal replacement therapy central venous catheters, tunnelled central venous catheters and portacaths inserted into the subclavian or jugular veins (may require combination with ‘Pecs 1’ block for component of pain below the clavicle) -Tracheostomy (see below discussion on safety profile of performing bilateral blocks and risks of respiratory distress due to phrenic nerve or recurrent largyngeal nerve block) -More commonly in adults: thyroid (again, bilateral) and carotid surgery Contraindications: -local sepsis or rash Anatomy: The cervical plexus arises from C1-C4 mixed spinal nerves (fig. 1): Somatic sensory branches: -arise from C2-C4 as the mixed spinal nerves leave the sulcus between the anterior and posterior tubercles of the transverse process (note C7 does not have an anterior tubercle or bifid spinous process): -pass between longus capitis and middle scalene perforating the prevertebral fascia. Note at C4 level the anterior scalene has largely disappeared having taken the bulk of its vertebral bony origin lower down. The bulkiest of the scalene muscles is the middle scalene and remains in view at this level: -then pass behind the internal jugular vein out into the potential space between the investing layer of deep fascia ensheathing the sternocleidomastoid, and the prevertebral layer of deep fascia covering levator scapulae (fig. -
33. Spinal Nerves. Cervical Plexus
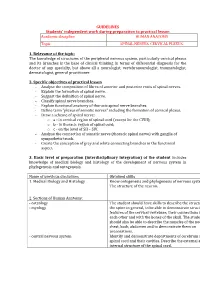
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -

University Microfilms 300 North 2Eeb Road Ann Arbor, Michigan 48106
INFORMATION TO USERS This dissertation was produced from a microfilm copy of the original document. While the most advanced technological means to photograph and reproduce this document have been used, the quality is heavily dependent upon the quality of the original submitted. The following explanation of techniques is provided to help you understand markings or patterns ...tch may appear on this reproduction. 1. The sign or "target" for pages apparently lacking from the document photographed is "Missing Page(s)''. If it was possible to obtain the missing page(s) or section, they are spliced into the film along with adjacent pages. This may have necessitated cutting thru an image and duplicating adjacent pages to insure you complete continuity. 2. When an image on the film is obliterated with a large round black mark, it is an indication that the photographer suspected that the copy may have moved during exposure and thus cause a blurred image. You will find a good image of the page in the adjacent frame. 3. When a map, drawing or chart, etc., was part of the material being photographed the photographer followed a definite method in "sectioning" the material. It is customary to begin photoing at the upper left hand corner of a large sheet and to continue photoing from left to right in equal sections with a small overlap. If necessary, sectioning is continued again — beginning below the first row and continuing on until complete. 4. The majority of users indicate that the textual content is of greatest value, however, a somewhat higher quality reproduction could be made from "photographs" if essential to the understanding of the dissertation. -

Vulvodynia: a Common and Underrecognized Pain Disorder in Women and Female Adolescents Integrating Current
21/4/2017 www.medscape.org/viewarticle/877370_print www.medscape.org This article is a CME / CE certified activity. To earn credit for this activity visit: http://www.medscape.org/viewarticle/877370 Vulvodynia: A Common and UnderRecognized Pain Disorder in Women and Female Adolescents Integrating Current Knowledge Into Clinical Practice CME / CE Jacob Bornstein, MD; Andrew Goldstein, MD; Ruby Nguyen, PhD; Colleen Stockdale, MD; Pamela Morrison Wiles, DPT Posted: 4/18/2017 This activity was developed through a comprehensive review of the literature and best practices by vulvodynia experts to provide continuing education for healthcare providers. Introduction Slide 1. http://www.medscape.org/viewarticle/877370_print 1/69 21/4/2017 www.medscape.org/viewarticle/877370_print Slide 2. Historical Perspective Slide 3. http://www.medscape.org/viewarticle/877370_print 2/69 21/4/2017 www.medscape.org/viewarticle/877370_print Slide 4. What we now refer to as "vulvodynia" was first documented in medical texts in 1880, although some believe that the condition may have been described as far back as the 1st century (McElhiney 2006). Vulvodynia was described as "supersensitiveness of the vulva" and "a fruitful source of dyspareunia" before mention of the condition disappeared from medical texts for 5 decades. Slide 5. http://www.medscape.org/viewarticle/877370_print 3/69 21/4/2017 www.medscape.org/viewarticle/877370_print Slide 6. Slide 7. http://www.medscape.org/viewarticle/877370_print 4/69 21/4/2017 www.medscape.org/viewarticle/877370_print Slide 8. Slide 9. Magnitude of the Problem http://www.medscape.org/viewarticle/877370_print 5/69 21/4/2017 www.medscape.org/viewarticle/877370_print Slide 10. -

Anatomy of Spinal Nerves in the First Turkish Illustrated Anatomy Handwritten Textbook
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DSpace@HKU Childs Nerv Syst DOI 10.1007/s00381-016-3136-9 COVER EDITORIAL Anatomy of spinal nerves in the first Turkish illustrated anatomy handwritten textbook Murat Çetkin1 & Mustafa Orhan1 & İlhan Bahşi1 & Begümhan Turhan2 Received: 26 May 2016 /Accepted: 30 May 2016 # Springer-Verlag Berlin Heidelberg 2016 BTeşrih-ül Ebdan ve Tercümânı Kıbale-i Feylesûfan^ is the the book, İtâḳî acknowledges the contributions of the Grand first handwritten anatomy textbook with illustrations written Vizier [4, 7]. in Turkish in 17th century by Şemseddîn-i İtâḳî. BTeşrih^ has Not many textbooks about anatomy existed in the Islamic different meanings such as anatomy, skeleton, and cutting a World and the Ottoman Empire until İtâḳî’sbook[9]. In other corpse into pieces [1]. BTeşrih-ül Ebdan ve Tercümânı Kıbale- medical textbooks, anatomy occupies only a few pages in i Feylesûfan ^ means dissection of the body and scholars’ different sections [4]. İtâḳî’s book is a pioneer in its area as birth knowledge [2]. Since this is the first handwritten text- it is written in Turkish, and it is supported with illustrations book in Turkish, it has great importance in the development of [4]. In addition to Turkish, the book contains mostly Arabic medicine in Ottoman Empire. This book was written while and rarely Persian terms as well [4, 6, 7]. Some editions of this Grand Vizier Recep Pasha was in power, and it was dedicated book which was written in the 17th century were reprinted in to the Sultan of that period, Murat the IVth [3, 4].