58225-A-Rare-Anatomical-Variation-Of-The-Lesser-Occipital-Nerve.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Superficial (And Intermediate) Cervical Plexus Block
Superficial (and Intermediate) Cervical Plexus Block Indications: -Tympanomastoid surgery. When combined with the auricular branch of the vagus (‘nerve of arnold’) by infiltrating subcutaneously into the medial side of the tragus), obviates the need for opiates. -Pinnaplasty or Otoplasty -Lymph node excision (within the anterior and posterior triangles of the neck) -Clavicular surgery or fractures (may require intermediate cervical plexus block and its combination with interscalene block, see below) -Central Venous Catheters: Renal replacement therapy central venous catheters, tunnelled central venous catheters and portacaths inserted into the subclavian or jugular veins (may require combination with ‘Pecs 1’ block for component of pain below the clavicle) -Tracheostomy (see below discussion on safety profile of performing bilateral blocks and risks of respiratory distress due to phrenic nerve or recurrent largyngeal nerve block) -More commonly in adults: thyroid (again, bilateral) and carotid surgery Contraindications: -local sepsis or rash Anatomy: The cervical plexus arises from C1-C4 mixed spinal nerves (fig. 1): Somatic sensory branches: -arise from C2-C4 as the mixed spinal nerves leave the sulcus between the anterior and posterior tubercles of the transverse process (note C7 does not have an anterior tubercle or bifid spinous process): -pass between longus capitis and middle scalene perforating the prevertebral fascia. Note at C4 level the anterior scalene has largely disappeared having taken the bulk of its vertebral bony origin lower down. The bulkiest of the scalene muscles is the middle scalene and remains in view at this level: -then pass behind the internal jugular vein out into the potential space between the investing layer of deep fascia ensheathing the sternocleidomastoid, and the prevertebral layer of deep fascia covering levator scapulae (fig. -
33. Spinal Nerves. Cervical Plexus
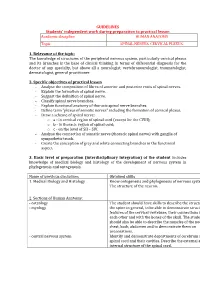
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -

Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2
Open Access Review Article DOI: 10.7759/cureus.5679 Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2 Bruno Bordoni 1 , Marta Simonelli 2 , Maria Marcella Lagana 3 1. Cardiology, Foundation Don Carlo Gnocchi, Milan, ITA 2. Osteopathy, French-Italian School of Osteopathy, Pisa, ITA 3. Radiology, IRCCS Fondazione Don Carlo Gnocchi Onlus, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract The tentorium cerebelli is a meningeal portion in relation to the skull, the nervous system, and the cervical tract. In this second part, the article discusses the systematic tentorial relationships, such as the central and cervical neurological connections, the venous circulation and highlights possible clinical alterations that could cause pain. To understand the function of anatomy, we should always remember that every area of the human body is never a segment, but a functional continuum. Categories: Physical Medicine & Rehabilitation, Anatomy, Osteopathic Medicine Keywords: tentorium cerebelli, fascia, pain, venous circulation, neurological connections, cranio Introduction And Background Cervical neurological connections The ansa cervicalis characterizes the first cervical roots and connects all anterior cervical nerve exits with the inferior floor of the oral cavity, the trigeminal system, the respiratory control system, and the sympathetic system. The descending branch of the hypoglossal nerve anastomoses with C1, forming the ansa hypoglossi or ansa cervicalis superior [1]. The inferior root of the ansa cervicalis, also known as descendens cervicalis, is formed by ascendant fibers from spinal nerves C2-C3 and occasionally fibers C4, lying anteriorly to the common carotid artery (it passes laterally or medially to the internal jugular vein upon anatomical variations) [1]. -
The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -

Communications of Transverse Cervical Cutaneous Nerve with the Cervical Branch of Facial Nerve and Its Variant Nerve Endings
ogy: iol Cu ys r h re P n t & R y e s Anatomy & Physiology: Current m e Sirasanagandla et al., Anatom Physiol 2013, 3:1 o a t r a c n h DOI: 10.4172/2161-0940.1000114 A Research ISSN: 2161-0940 Case Report Open Access Communications of Transverse Cervical Cutaneous Nerve with the Cervical Branch of Facial Nerve and its Variant Nerve Endings Deep in the Parotid Gland Srinivasa Rao Sirasanagandla*, Swamy Ravindra S, Sapna Marpalli and Satheesha Nayak B Department of Anatomy, Melaka Manipal Medical College, Manipal University, Madhav Nagar, Manipal, Karnataka, India Abstract Anastomoses between the transverse cervical cutaneous nerve and the cervical branch of facial nerve are regularly present. The anatomic locations of these anastomoses were poorly documented in the literature. During regular dissection, we came across two of such anastomoses: one of the two anastomoses was identified posterior to submandibular gland, and the other was noted within the parenchyma of the parotid gland. Prior knowledge of anatomic locations of these anastomoses is clinically important as it allows a method for identification and preservation of the cervical branch of the facial nerve as well as a starting point for retrograde facial nerve dissections. In addition, few terminal nerve endings of transverse cervical cutaneous nerve were seen along the retromandibular vein, ducts and some were penetrating the interlobular septa of parotid gland. The functional significance of anatomic variations of its nerve terminal ends deep in the gland is yet to be evaluated. Keywords: Anastomoses; Transverse cervical cutaneous nerve; (TCCN) and supraclavicular nerves pierce the fascia to supply the skin. -

Reconstruction of Complex Defects of the Extracranial Facial Nerve: Technique of “The Trifurcation Approach”
European Archives of Oto-Rhino-Laryngology (2019) 276:1793–1798 https://doi.org/10.1007/s00405-019-05418-4 HEAD AND NECK Reconstruction of complex defects of the extracranial facial nerve: technique of “the trifurcation approach” Dirk Beutner1 · Maria Grosheva2 Received: 28 January 2019 / Accepted: 31 March 2019 / Published online: 4 April 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Reconstruction of complex defects of facial nerve (FN) after extensive cancer surgery requires individualized solutions. We describe the trifurcation technique as a modifcation of the combined approach on example of two patients with locally advanced parotid cancer. Methods Due to perineural invasion, extensive resection of the FN from the mastoid segment to the peripheral branches was required. For reanimation of the upper face, a complex cervical plexus graft was sutured end-to-end to the mastoid segment of the FN trunk. The branches of the graft enabled reanimation of three peripheral temporal and zygomatic branches. The mandibular branch was sutured end-to-side to the hypoglossal nerve (hypoglossal–facial nerve transfer, HFNT). Addition- ally, the buccal branch was independently reanimated with ansa cervicalis. Results Facial reanimation was successful in both patients. Good resting tone and voluntary movement were achieved with a mild degree of synkinesis after 13 months. Patient 1 showed the Sunnybrook (SB) composite score 69 [76 (voluntary move- ment score) − 0 (resting symmetry score) − 7 (synkinesis score)]. In patient 2, the SB composite score was 76 (80 − 0 − 4, respectively). Conclusions In this trifurcation approach, cervical cutaneous plexus provides a long complex nerve graft, which allows bridging the gap between proximal FN stump and several peripheral branches without great expenditure. -
Comparative Study of Superficial Cervical Plexus Block and Nerve of Arnold Block with Intravenous Antiemetic Drugs Dexamethasone
Comparative Study of Superficial Cervical Plexus Block and Nerve of Arnold Block with Intravenous antiemetic drugs Dexamethasone and Ondansetron and Incidence of Post-operative Nausea Vomiting for Inner Ear Surgery Indiana University School of Medicine Riley Hospital for Children Principal Investigator: Malik Nouri, MD Co Investigator: Charles Yates, MD Version 2.0 Date: 01/27/2017 Page 1 of 12 Table of Contents: Study Schema 1.0 Background 2.0 Rationale and Specific Aims 3.0 Inclusion/Exclusion Criteria 4.0 Enrollment/Randomization 5.0 Study Procedures 6.0 Reporting of Adverse Events of Unanticipated Problems involving Risk to Participants or Others 7.0 Study Withdrawal/Discontinuation 8.0 Statistical Considerations 9.0 Privacy/Confidentiality Issues 10.0 Follow-up and Record Retention 11.0 Analysis of Results Page 2 of 12 1.0 Background Patients that undergo inner ear surgery often complain of postoperative nausea and vomiting (PONV) despite prophylactic antiemetic regiments with 5HT3 antagonists, steroids and vigorous hydration. Patients still experience this unpleasant feeling that may prolong hospital stay and can lead to nutritional issues such as dehydration and huge patient and family dissatisfaction. We would like to explore the use of regional anesthesia and potential antiemetic proprieties and compare it’s efficacy to the existing therapy. PONV is an unpleasant complication following anesthesia, it is well known that patients undergoing certain surgical procedures such as those involving the inner ear, the tympanomastoid cells, and the cochlear organ may be more prone to PONV. This complication can be anticipated in those instances and prophylactically treated with antiemetics, Vigorous hydration and cautious selection of anesthetic technique and avoidance of drugs known to promote nausea1, 2, 3. -

A Case of the Human Sternocleidomastoid Muscle Additionally Innervated by the Hypoglossal Nerve
Okajimas Folia Anat. Jpn., 69(6): 361-368, March, 1993 A Case of the Human Sternocleidomastoid Muscle Additionally Innervated by the Hypoglossal Nerve By Masahiro KOIZUMI, Masaharu HORIGUCHI, Shin'ichi SEKIYA, Sumio ISOGAI and Masato NAKANO Department of Anatomy, Iwate Medical University School of Medicine. Morioka, 020 Japan -Received for Publication, October 19, 1992- Key Words: Sternocleidomastoid muscle, Hypoglossal nerve, Superior sternoclavicular muscle (Hyrtl), Dual nerve supply, Gross anatomy Summary: An anomalous nerve supply from the hypoglossal nerve (XII) to the sternocleidomastoid muscle (SM) was observed in the right neck of an 82-year-old Japanese female. This nerve branch arose from the hypoglossal nerve at the origin of the superior root of the ansa cervicalis. The nerve fiber analysis revealed that this branch consisted of fibers from the hypoglossal nerve, the first and the second cervical nerves and had the same component as the superior root of the ansa cervicalis. SM appeared quite normal and the most part was innervated by the accessory nerve and a branch from the cervical plexus. The anomalous branch from XII supplied the small deep area near the anterior margin of the middle of the sternomastoid portion of SM. It is reasonable to think that the small deep area of SM, which was innervated by the anomalous branch from XII, occurs as the result of fusion of the muscular component from infrahyoid muscles. If the muscular component does not fuse with SM, it is thought to appear as an aberrant muscle such as the superior sternoclavicular muscle (Hyrtl) which is also supplied from a branch of the superior root of the ansa cervicalis. -

Mapping Sensory Nerve Communications Between Peripheral Nerve Territories
Clinical Anatomy 27:681–690 (2014) ORIGINAL COMMUNICATION Mapping Sensory Nerve Communications Between Peripheral Nerve Territories 1 2 1* ADIL LADAK, R. SHANE TUBBS, AND ROBERT J. SPINNER 1Department of Neurologic Surgery, Orthopedics and Anatomy, Mayo Clinic, Rochester, Minnesota 2Department of Neurosurgery, Children’s Hospital, Birmingham, Alabama The human cutaneous sensory map has been a work in progress over the past century, depicting sensory territories supplied by both the spinal and cranial nerves. Two critical discoveries, which shaped our understanding of cutaneous innervation, were sensory dermatome overlap between contiguous spinal levels and axial lines across areas where no sensory overlap exists. These concepts define current dermatome maps. We wondered whether the overlap between contiguous sensory territories was even tighter: if neural communications were present in the peripheral nerve territories consistently connecting contiguous spinal levels? A literature search using peer-reviewed articles and established anatomy texts was performed aimed at identifying the presence of communica- tions between sensory nerves in peripheral nerve territories and their relation- ship to areas of adjacent and non-adjacent spinal or cranial nerves and axial lines (lines of discontinuity) in the upper and lower limbs, trunk and perineum, and head and neck regions. Our findings demonstrate the consistent presence of sensory nerve communications between peripheral nerve territories derived from spinal nerves within areas of axial lines in the upper and lower limbs, trunk and perineum, and head and neck. We did not find examples of communications crossing axial lines in the limbs or lines of discontinuity in the face, but did find examples crossing axial lines in the trunk and perineum. -
The LATIN LANGUAGE and Bases of Medical Terminology
The LATIN LANGUAGE and Bases of Medical Terminology The LATIN LANGUAGE and Bases of Medical Terminology ОДЕСЬКИЙ ДЕРЖАВНИЙ МЕДИЧНИЙ УНІВЕРСИТЕТ THE ODESSA STATE MEDICAL UNIVERSITY Áiáëiîòåêà ñòóäåíòà-ìåäèêà Medical Student’s Library Започатковано 1999 р. на честь 100-річчя Одеського державного медичного університету (1900–2000 рр.) Initiated in 1999 to mark the Centenary of the Odessa State Medical University (1900–2000) 2 THE LATIN LANGUAGE AND BASES OF MEDICAL TERMINOLOGY Practical course Recommended by the Central Methodical Committee for Higher Medical Education of the Ministry of Health of Ukraine as a manual for students of higher medical educational establishments of the IV level of accreditation using English Odessa The Odessa State Medical University 2008 3 BBC 81.461я73 UDC 811.124(075.8)61:001.4 Authors: G. G. Yeryomkina, T. F. Skuratova, N. S. Ivashchuk, Yu. O. Kravtsova Reviewers: V. K. Zernova, doctor of philological sciences, professor of the Foreign Languages Department of the Ukrainian Medical Stomatological Academy L. M. Kim, candidate of philological sciences, assistant professor, the head of the Department of Foreign Languages, Latin Language and Bases of Medical Terminology of the Vinnitsa State Medical University named after M. I. Pyrogov The manual is composed according to the curriculum of the Latin lan- guage and bases of medical terminology for medical higher schools. Designed to study the bases of general medical and clinical terminology, it contains train- ing exercises for the class-work, control questions and exercises for indivi- dual student’s work and the Latin-English and English-Latin vocabularies (over 2,600 terms). For the use of English speaking students of the first year of study at higher medical schools of IV accreditation level. -

5. Upper Extremity Neuroanatomy
5. UPPER EXTREMITY compartments of the NEUROANATOMY arm). The brachial plexus divisions INTRODUCTION pass posterior to the mid-point of Regional anesthesia of the upper extremity in- the clavicle through volves two major nerve plexuses, the cervical plexus the cervico-axillary and the brachial plexus. A detailed understanding of canal. the anatomy of these nerve plexuses and surrounding • Three cords. The structures is essential for the safe and successful prac- divisions coalesce tice of regional anesthesia in this area of the body. to form three cords. The anterior CERVICAL PLEXUS divisions of the superior and middle The cervical plexus is formed from a series of nerve trunk form the loops between adjacent anterior rami of cervical nerve lateral cord. The roots C1 through C4. The cervical plexus is deep to the anterior division of sternocleidomastoid muscle and medial to the scalene the inferior trunk muscles. The deep branches of the plexus are motor becomes the medial nerves. They include the phrenic nerve (diaphragm cord. The posterior muscle) and the ansa cervicalis nerve (omohyoid, divisions of all sternothyroid, and sternohyoid muscles). The named three trunks unite nerves of the superficial cervical plexus are branches to form the posterior from the loops and emerge from the middle of the ster- Figure 5-1. Dissection of the superficial cervical plexus in the posterior triangle cord. The cords are nocleidomastoid muscle (Figure 5-1): BRACHIAL PLEXUS named based on their relationship to the axillary artery (as this • Lesser occipital nerve (C2): innervates the skin The brachial plexus is formed from the five roots neurovascular bundle passes in its sheath into posterior to the ear.