Retromandibular Vein Position and Course
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Should We Report Posterior Fossa Emissary Veins?
Diagn Interv Radiol 2014; 20:78–81 NEURORADIOLOGY © Turkish Society of Radiology 2014 PICTORIAL ESSAY Why should we report posterior fossa emissary veins? Yeliz Pekçevik, Rıdvan Pekçevik ABSTRACT osterior fossa emissary veins pass through cranial apertures and par- Posterior fossa emissary veins are valveless veins that pass ticipate in extracranial venous drainage of the posterior fossa dural through cranial apertures. They participate in extracranial ve- sinuses. These emissary veins are usually small and asymptomatic nous drainage of the posterior fossa dural sinuses. The mas- P toid emissary vein, condylar veins, occipital emissary vein, in healthy people. They protect the brain from increases in intracranial and petrosquamosal sinus are the major posterior fossa emis- pressure in patients with lesions of the neck or skull base and obstructed sary veins. We believe that posterior fossa emissary veins can internal jugular veins (1). They also help to cool venous blood circulat- be detected by radiologists before surgery with a thorough understanding of their anatomy. Describing them using tem- ing through cephalic structures (2). Emissary veins may be enlarged in poral bone computed tomography (CT), CT angiography, patients with high-flow vascular malformations or severe hypoplasia or and cerebral magnetic resonance (MR) venography exam- inations results in more detailed and accurate preoperative aplasia of the jugular veins. They are associated with craniofacial syn- radiological interpretation and has clinical importance. This dromes (1, 3). Dilated emissary veins may cause tinnitus (4, 5). pictorial essay reviews the anatomy of the major and clini- We aim to emphasize the importance of reporting posterior fossa em- cally relevant posterior fossa emissary veins using high-reso- lution CT, CT angiography, and MR venography images and issary veins prior to surgeries that are related to the posterior fossa and discusses the clinical importance of reporting these vascular mastoid region. -

Arteria Carotis Externa ACE External Carotid Artery
Common carotid artery CCA External Carotid artery ECA Internal carotid artery, ICA Subclavian artery SA and veins Ivo Klepáček ´tooth ache´ Salisbury cathedrale Three vascular systems are finally formed: Intraembryonic (cardinal); aortic sac (later gives rise aortic arches) Vitelline (aa. + vv.) Development of the vascular Placental system (umbilical Day 27 aa. + vv.) 1st – maxillary artery 2nd – hyoid, stapedial aa. 3rd – common carotid a. and first part of the internal carotid a., external carotid a. 4th – part of the subclavian aa. some of intersegmental arteries Common carotid artery Anterolaterally – skin, fascia, sternocleidomastoid muscle, sternohyoid, sternothyroid, superior belly of the omohyoid Posteriorly – transverse process of the C4 vertebrae, prevertebral muscles, sympathetic trunk Medially – wall of the pharynx and larynx, trachea, esophagus, the lobe of the thyroid gland Laterally – the internal jugular vein, vagus nerve (posterolaterally) Fascia pretrachealis a ACC Pretracheal fascia and ACC Sympathetic plexus surrounding arteries comes from sympathetic trunk External carotid artery ECA Anterolaterally – sternocleidomastoid muscle, XII. nerve, within parotid gland is crossed by VII. nerve, fascia, skin Medially – wall of the pharynx, internal carotid artery, stylopharyngeus, pharyngeal branch of the vagus For head without orbit, inner ear and brain Internal jugular Styloid vein lies septum dorsally and laterally from internal carotid artery behind m. m. stylohyoideus and styloglossus External carotid artery lies ventrally -

The Anatomy of Th-E Blood Vascular System of the Fox ,Squirrel
THE ANATOMY OF TH-E BLOOD VASCULAR SYSTEM OF THE FOX ,SQUIRREL. §CIURUS NlGER. .RUFIVENTEB (OEOEEROY) Thai: for the 009m of M. S. MICHIGAN STATE COLLEGE Thomas William Jenkins 1950 THulS' ifliillifllfllilllljllljIi\Ill\ljilllHliLlilHlLHl This is to certifg that the thesis entitled The Anatomy of the Blood Vascular System of the Fox Squirrel. Sciurus niger rufiventer (Geoffroy) presented by Thomas William Jenkins has been accepted towards fulfillment of the requirements for A degree in MEL Major professor Date May 23’ 19500 0-169 q/m Np” THE ANATOMY OF THE BLOOD VASCULAR SYSTEM OF THE FOX SQUIRREL, SCIURUS NIGER RUFIVENTER (GEOFFROY) By THOMAS WILLIAM JENKINS w L-Ooffi A THESIS Submitted to the School of Graduate Studies of Michigan State College of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Department of Zoology 1950 \ THESlSfi ACKNOWLEDGMENTS Grateful acknowledgment is made to the following persons of the Zoology Department: Dr. R. A. Fennell, under whose guidence this study was completed; Mr. P. A. Caraway, for his invaluable assistance in photography; Dr. D. W. Hayne and Mr. Poff, for their assistance in trapping; Dr. K. A. Stiles and Dr. R. H. Manville, for their helpful suggestions on various occasions; Mrs. Bernadette Henderson (Miss Mac), for her pleasant words of encouragement and advice; Dr. H. R. Hunt, head of the Zoology Department, for approval of the research problem; and Mr. N. J. Mizeres, for critically reading the manuscript. Special thanks is given to my wife for her assistance with the drawings and constant encouragement throughout the many months of work. -

Variant Position of the Facial Nerve in Parotid Gland
eISSN 1308-4038 International Journal of Anatomical Variations (2011) 4: 3–4 Case Report Variant position of the facial nerve in parotid gland Published online January 14th, 2011 © http://www.ijav.org Rajesh B. ASTIK ABSTRACT Urvi H. DAVE The division of the parotid gland into superficial and deep lobes by facial nerve has an important implication in parotid Krishna Swami GAJENDRA gland neoplasm. This plane is used in superficial or total parotidectomy to avoid damage to the facial nerve. During routine dissection in the Department of Anatomy, we found variably located facial nerve in the parotid gland of the left side. The main trunk of the facial nerve was located between maxillary vein and superficial temporal vein. It was divided into temporofacial and cervicofacial divisions. Both divisions crossed maxillary vein superficially instead Department of Anatomy, GSL Medical College, Rajahmundry, District- East Godavari, of retromandibular vein which was formed outside the parotid gland substance. Andhra Pradesh, INDIA. The operating surgeon should be familiar with this variation during parotidectomy to reduce the iatrogenic injury to the facial nerve. © IJAV. 2011; 4: 3–4. Dr. Rajesh B. Astik Associate Professor Department of Anatomy GSL Medical College NH-5, Rajahmundry District- East Godavari. Andhra Pradesh, 533296, INDIA. +91 883 2484999 [email protected] Received July 15th, 2010; accepted January 4th, 2011 Key words [facial nerve] [parotid gland] [retromandibular vein] [total parotidectomy] Introduction vein superficially instead of the retromandibular vein. The The retromandibular vein is formed by union of the maxillary retromandibular vein was formed by union of maxillary and and superficial temporal veins in the parotid gland [1]. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

PAROTIDECTOMY Johan Fagan
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY PAROTIDECTOMY Johan Fagan The facial nerve is central to parotid Structures that traverse, or are found surgery for both surgeon and patient. within the parotid gland Knowledge of the surgical anatomy and the landmarks to find the facial nerve are • Facial nerve and branches (Figure 1) the key to preserving facial nerve function. • External carotid artery: It gives off the Surgical Anatomy transverse facial artery inside the gland before dividing into the internal maxil- Parotid gland lary and the superficial temporal arteries (Figure 2). The parotid glands are situated anteriorly and inferiorly to the ear. They overlie the vertical mandibular rami and masseter muscles, behind which they extend into the retromandibular sulci. The glands extend superiorly from the zygomatic arches and inferiorly to below the angles of the mandible where they overlie the posterior bellies of the digastric and the sternoclei- domastoid muscles. The parotid duct exits the gland anteriorly, crosses the masseter muscle, curves medially around its anterior margin, pierces the buccinator muscle, and Figure 1: Main branches of facial nerve enters the mouth opposite the 2nd upper molar tooth. Superficial Muscular Aponeurotic System and Parotid Fascia The Superficial Muscular Aponeurotic System (SMAS) is a fibrous network that invests the facial muscles and connects them with the dermis. It is continuous with the platysma inferiorly; superiorly it at- taches to the zygomatic arch. In the lower face, the facial nerve courses deep to the SMAS and the platysma. The parotid Figure 2: Branches of the external carotid glands are contained within two layers of artery parotid fascia, which extend from the zygoma above and continue as cervical • Veins: The maxillary and superficial fascia below. -

Anatomic Variability in the Relation Between the Retromandibular Vein and the Facial Nerve: a Case Report, Literature Review and Classification
Folia Morphol. Vol. 72, No. 4, pp. 371–375 DOI: 10.5603/FM.2013.0062 C A S E R E P O R T Copyright © 2013 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Anatomic variability in the relation between the retromandibular vein and the facial nerve: a case report, literature review and classification M. Piagkou1, M. Tzika2, G. Paraskevas2, K. Natsis2 1Department of Anatomy, Medical School, National and Kapodistrian University of Athens, Greece 2Department of Anatomy, Medical School, Aristotle University of Thessaloniki, Greece [Received 5 April 2013; Accepted 24 May 2013] Knowledge of anatomic variations concerning head and neck veins is important to surgeons performing interventions in these regions, as well as to radiologists. The retromandibular vein is used as a guide to expose the facial nerve branches inside the parotid gland, during parotid surgery and open reduction of mandibular condyle fractures. It is also used as a landmark for localisation of the nerve and compartmentalisation of parotid gland lesions preoperatively, during computed tomography, magnetic resonance imaging and sonography. In this paper, the anomalous retromandibular vein’s course on the left side of a male cadaver is described. The vein was formed around the nerve, while the maxillary vein travelled medial to the facial nerve branches and superficial to the superficial temporal vein. Interestingly, the facial nerve temporofacial division crossed again the superficial temporal vein upwards, forming a “nerve fork”. The incidence of the reported variability of the relationship between the retromandibular vein and the facial nerve are discussed with a detailed literature review. Accordingly, the typical deep position of the retromandibular vein in relation to the facial nerve is estimated to 88.17% to all sides. -

The Development of Mammalian Dural Venous Sinuses with Especial Reference to the Post-Glenoid Vein
J. Anat. (1967), 102, 1, pp. 33-56 33 With 12 figures Printed in Great Britian The development of mammalian dural venous sinuses with especial reference to the post-glenoid vein H. BUTLER Department ofAnatomy, University of Saskatchewan, Saskatoon, Canada The intracranial venous outflow of mammals drains into both the internal and external jugular veins and the relative role of these two veins varies between different adult mammals as well as at different phases of embryonic and foetal life. In general, the primary head vein (consisting of venae capitis medialis and lateralis and their tributaries) gives rise to the dural venous sinuses which drain into the anterior cardinal vein (the future internal jugular vein). The external jugular veins appear as the face and jaws develop but, at all times, the two venous systems freely com- municate with each other. Morphologically, as shown by Sutton (1888), both the dural venous sinuses and the external jugular venous system are extracranial in so far as they are situated outside the dura mater. The chondrocranium and the dermocranium, however, develop in between the dural venous sinuses and the external jugular vein system (Butler, 1957). Thus, in the adult mammal, the bony skull wall separates the two venous systems, and therefore the dural venous sinuses are topographically intracranial whereas the external jugular venous system is extracranial. Furthermore the development of the skull localizes the connexions between the dural venous sinuses and the external jugular venous system to the various fontanelles and neuro-vascular foramina to form the emissary veins. The post-glenoid vein is one of the more important and controversial emissary veins since its presence or absence has been used in attempts to establish mammalian phylogenetic relationships (van Gelderen, 1925; Boyd, 1930). -

Temporal Regions and Ear
Unit 16: Temporal regions and ear GENERAL OBJECTIVES: - general considerations of the organization of layers in parotid and temporal/infratemporal regions - muscles of mastication and TMJ - structure and function of the ear - irrigation and innervations of parotid, temporal/infratemporal regions SPECIFIC OBJECTIVES: 1. Parotid region Boundaries (Parotid Bed): Sup., Inf., Ant., Post.. Med. (Styloid Process), Lat. (Superficial Fascia with Great Auricular Nerve) Contents: Parotid Fascia (continuous with Investing Fascia) Parotid Gland: Position, Parts, Parotid Duct Structures within the Gland: Ext. Carotid Artery -> Terminal Branches Retromandibular Vein -> Anterior & Posterior Branches Parotid Lymph Nodes Facial Nerve -> 5 Terminal Branches 2. Temporal and infratemporal regions Boundaries and contents: Spenomandibular Ligament Pterygoid Muscles (Lateral & Medial) Maxillary Artery (1st., 2nd. & 3rd. Parts) Branches: Middle Meningeal (Extracranial Course) Others Pterygoid Venous Plexus & Communications Mandibular Nerve (V3): Ant. & Post. Divisions Branches: Muscular, Buccal & Auriculotemporal Nerves Inferior Alveolar & Lingual Nerves Chorda Tympani Otic Ganglion (Parasympathetic) 3. Temporomandibular Joint Articular Surfaces Capsule & Ligaments, Sphenomandibular Ligament Articular Disc (2 separate joint cavities & movements) Movements of the T.M.J.: [(i) Rotation, (ii) Anterior Gliding] -> Opening/Closing Protraction/Retraction 4. Branchial (pharyngeal arch) muscle groups (Muscles of mastication) Muscles of Mastication Masseter, Temporalis, -
27. Veins of the Head and Neck
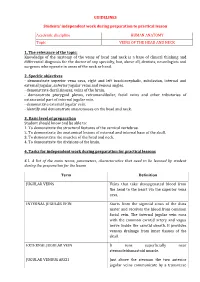
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

Atlas of Topographical and Pathotopographical Anatomy of The
Contents Cover Title page Copyright page About the Author Introduction Part 1: The Head Topographic Anatomy of the Head Cerebral Cranium Basis Cranii Interna The Brain Surgical Anatomy of Congenital Disorders Pathotopography of the Cerebral Part of the Head Facial Head Region The Lymphatic System of the Head Congenital Face Disorders Pathotopography of Facial Part of the Head Part 2: The Neck Topographic Anatomy of the Neck Fasciae, Superficial and Deep Cellular Spaces and their Relationship with Spaces Adjacent Regions (Fig. 37) Reflex Zones Triangles of the Neck Organs of the Neck (Fig. 50–51) Pathography of the Neck Topography of the neck Appendix A Appendix B End User License Agreement Guide 1. Cover 2. Copyright 3. Contents 4. Begin Reading List of Illustrations Chapter 1 Figure 1 Vessels and nerves of the head. Figure 2 Layers of the frontal-parietal-occipital area. Figure 3 Regio temporalis. Figure 4 Mastoid process with Shipo’s triangle. Figure 5 Inner cranium base. Figure 6 Medial section of head and neck Figure 7 Branches of trigeminal nerve Figure 8 Scheme of head skin innervation. Figure 9 Superficial head formations. Figure 10 Branches of the facial nerve Figure 11 Cerebral vessels. MRI. Figure 12 Cerebral vessels. Figure 13 Dural venous sinuses Figure 14 Dural venous sinuses. MRI. Figure 15 Dural venous sinuses Figure 16 Venous sinuses of the dura mater Figure 17 Bleeding in the brain due to rupture of the aneurism Figure 18 Types of intracranial hemorrhage Figure 19 Different types of brain hematomas Figure 20 Orbital muscles, vessels and nerves. Topdown view, Figure 21 Orbital muscles, vessels and nerves.