New Proposed Classification of Retromandibular Vein Root Variants Based on Cadaver Dissections and Review of Literature – Clinical Implications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Should We Report Posterior Fossa Emissary Veins?
Diagn Interv Radiol 2014; 20:78–81 NEURORADIOLOGY © Turkish Society of Radiology 2014 PICTORIAL ESSAY Why should we report posterior fossa emissary veins? Yeliz Pekçevik, Rıdvan Pekçevik ABSTRACT osterior fossa emissary veins pass through cranial apertures and par- Posterior fossa emissary veins are valveless veins that pass ticipate in extracranial venous drainage of the posterior fossa dural through cranial apertures. They participate in extracranial ve- sinuses. These emissary veins are usually small and asymptomatic nous drainage of the posterior fossa dural sinuses. The mas- P toid emissary vein, condylar veins, occipital emissary vein, in healthy people. They protect the brain from increases in intracranial and petrosquamosal sinus are the major posterior fossa emis- pressure in patients with lesions of the neck or skull base and obstructed sary veins. We believe that posterior fossa emissary veins can internal jugular veins (1). They also help to cool venous blood circulat- be detected by radiologists before surgery with a thorough understanding of their anatomy. Describing them using tem- ing through cephalic structures (2). Emissary veins may be enlarged in poral bone computed tomography (CT), CT angiography, patients with high-flow vascular malformations or severe hypoplasia or and cerebral magnetic resonance (MR) venography exam- inations results in more detailed and accurate preoperative aplasia of the jugular veins. They are associated with craniofacial syn- radiological interpretation and has clinical importance. This dromes (1, 3). Dilated emissary veins may cause tinnitus (4, 5). pictorial essay reviews the anatomy of the major and clini- We aim to emphasize the importance of reporting posterior fossa em- cally relevant posterior fossa emissary veins using high-reso- lution CT, CT angiography, and MR venography images and issary veins prior to surgeries that are related to the posterior fossa and discusses the clinical importance of reporting these vascular mastoid region. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

Unusual Venous Drainage of the Common Facial Vein. a Morphologycal Study ORIGINAL
International INTERNATIONAL ARCHIVES OF MEDICINE 2018 Medical Society SECTION: HUMAN ANATOMY Vol. 11 No. 29 http://imedicalsociety.org ISSN: 1755-7682 doi: 10.3823/2570 Unusual Venous Drainage of the Common Facial Vein. A Morphologycal Study ORIGINAL Sergio Ivan Granados-Torres1, Humberto Ferreira-Arquez2 1 Medicine student sixth Semester, University of Pamplona, Norte de Abstract Santander, Colombia, South America 2 Professor Human Morphology, Medicine Background: Anatomical knowledge of the facial vasculature is cru- Program, University of Pamplona, Morphology Laboratory Coordinator, cial not only for anatomists but also for oral and maxillofacial surgery, University of Pamplona. plastic surgeon, otorhinolaryngologists. Access pathways, pedicled and free flap transfer, and explantation and transplantation of total Contact information: faces are based on the proper assessment and use of the facial veins and arteries. The anatomical variations reported in the present study Ivan Granados-Torres. confirms the need for preoperative vascular imaging for sure good Address: University Campus, Kilometer venous outflow for the free flap survival. 1. Via Bucaramanga. Norte de Santander, Colombia. Suramérica, Pamplona Zip code: Aims: The aim of the present study was to describe a rare anato- 543050 Tel: 573176222213 mical variation of the common facial vein which not been previously described. [email protected] Methods and Findings: Head and neck region were carefully dissected as per standard dissection procedure, studied serially during the years 2013-2017 in 15 males and 2 females, i.e. 34 sides, embal- med adults cadavers with different age group, in the laboratory of Morphology of the University of Pamplona. In 33 sides (97 %) of the cases the anterior facial vein (FV) terminated into the internal jugular vein via the common facial vein (CFV) as per standard anatomic des- cription. -

Removal of Periocular Veins by Sclerotherapy
Removal of Periocular Veins by Sclerotherapy David Green, MD Purpose: Prominent periocular veins, especially of the lower eyelid, are not uncommon and patients often seek their removal. Sclerotherapy is a procedure that has been successfully used to permanently remove varicose and telangiectatic veins of the lower extremity and less frequently at other sites. Although it has been successfully used to remove dilated facial veins, it is seldom performed and often not recommended in the periocular region for fear of complications occurring in adjacent structures. The purpose of this study was to determine whether sclerotherapy could safely and effectively eradicate prominent periocular veins. Design: Noncomparative case series. Participants: Fifty adult female patients with prominent periocular veins in the lower eyelid were treated unilaterally. Patients and Methods: Sclerotherapy was performed with a 0.75% solution of sodium tetradecyl sulfate. All patients were followed for at least 12 months after treatment. Main Outcome Measures: Complete clinical disappearance of the treated vein was the criterion for success. Results: All 50 patients were successfully treated with uneventful resorption of their ectatic periocular veins. No patient required a second treatment and there was no evidence of treatment failure at 12 months. No new veins developed at the treated sites and no patient experienced any ophthalmologic or neurologic side effects or complications. Conclusions: Sclerotherapy appears to be a safe and effective means of permanently eradicating periocular veins. Ophthalmology 2001;108:442–448 © 2001 by the American Academy of Ophthalmology. Removal of asymptomatic facial veins, especially periocu- Patients and Materials lar veins, for cosmetic enhancement is a frequent request. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

PAROTIDECTOMY Johan Fagan
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY PAROTIDECTOMY Johan Fagan The facial nerve is central to parotid Structures that traverse, or are found surgery for both surgeon and patient. within the parotid gland Knowledge of the surgical anatomy and the landmarks to find the facial nerve are • Facial nerve and branches (Figure 1) the key to preserving facial nerve function. • External carotid artery: It gives off the Surgical Anatomy transverse facial artery inside the gland before dividing into the internal maxil- Parotid gland lary and the superficial temporal arteries (Figure 2). The parotid glands are situated anteriorly and inferiorly to the ear. They overlie the vertical mandibular rami and masseter muscles, behind which they extend into the retromandibular sulci. The glands extend superiorly from the zygomatic arches and inferiorly to below the angles of the mandible where they overlie the posterior bellies of the digastric and the sternoclei- domastoid muscles. The parotid duct exits the gland anteriorly, crosses the masseter muscle, curves medially around its anterior margin, pierces the buccinator muscle, and Figure 1: Main branches of facial nerve enters the mouth opposite the 2nd upper molar tooth. Superficial Muscular Aponeurotic System and Parotid Fascia The Superficial Muscular Aponeurotic System (SMAS) is a fibrous network that invests the facial muscles and connects them with the dermis. It is continuous with the platysma inferiorly; superiorly it at- taches to the zygomatic arch. In the lower face, the facial nerve courses deep to the SMAS and the platysma. The parotid Figure 2: Branches of the external carotid glands are contained within two layers of artery parotid fascia, which extend from the zygoma above and continue as cervical • Veins: The maxillary and superficial fascia below. -

Anatomic Variability in the Relation Between the Retromandibular Vein and the Facial Nerve: a Case Report, Literature Review and Classification
Folia Morphol. Vol. 72, No. 4, pp. 371–375 DOI: 10.5603/FM.2013.0062 C A S E R E P O R T Copyright © 2013 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Anatomic variability in the relation between the retromandibular vein and the facial nerve: a case report, literature review and classification M. Piagkou1, M. Tzika2, G. Paraskevas2, K. Natsis2 1Department of Anatomy, Medical School, National and Kapodistrian University of Athens, Greece 2Department of Anatomy, Medical School, Aristotle University of Thessaloniki, Greece [Received 5 April 2013; Accepted 24 May 2013] Knowledge of anatomic variations concerning head and neck veins is important to surgeons performing interventions in these regions, as well as to radiologists. The retromandibular vein is used as a guide to expose the facial nerve branches inside the parotid gland, during parotid surgery and open reduction of mandibular condyle fractures. It is also used as a landmark for localisation of the nerve and compartmentalisation of parotid gland lesions preoperatively, during computed tomography, magnetic resonance imaging and sonography. In this paper, the anomalous retromandibular vein’s course on the left side of a male cadaver is described. The vein was formed around the nerve, while the maxillary vein travelled medial to the facial nerve branches and superficial to the superficial temporal vein. Interestingly, the facial nerve temporofacial division crossed again the superficial temporal vein upwards, forming a “nerve fork”. The incidence of the reported variability of the relationship between the retromandibular vein and the facial nerve are discussed with a detailed literature review. Accordingly, the typical deep position of the retromandibular vein in relation to the facial nerve is estimated to 88.17% to all sides. -

Temporal Regions and Ear
Unit 16: Temporal regions and ear GENERAL OBJECTIVES: - general considerations of the organization of layers in parotid and temporal/infratemporal regions - muscles of mastication and TMJ - structure and function of the ear - irrigation and innervations of parotid, temporal/infratemporal regions SPECIFIC OBJECTIVES: 1. Parotid region Boundaries (Parotid Bed): Sup., Inf., Ant., Post.. Med. (Styloid Process), Lat. (Superficial Fascia with Great Auricular Nerve) Contents: Parotid Fascia (continuous with Investing Fascia) Parotid Gland: Position, Parts, Parotid Duct Structures within the Gland: Ext. Carotid Artery -> Terminal Branches Retromandibular Vein -> Anterior & Posterior Branches Parotid Lymph Nodes Facial Nerve -> 5 Terminal Branches 2. Temporal and infratemporal regions Boundaries and contents: Spenomandibular Ligament Pterygoid Muscles (Lateral & Medial) Maxillary Artery (1st., 2nd. & 3rd. Parts) Branches: Middle Meningeal (Extracranial Course) Others Pterygoid Venous Plexus & Communications Mandibular Nerve (V3): Ant. & Post. Divisions Branches: Muscular, Buccal & Auriculotemporal Nerves Inferior Alveolar & Lingual Nerves Chorda Tympani Otic Ganglion (Parasympathetic) 3. Temporomandibular Joint Articular Surfaces Capsule & Ligaments, Sphenomandibular Ligament Articular Disc (2 separate joint cavities & movements) Movements of the T.M.J.: [(i) Rotation, (ii) Anterior Gliding] -> Opening/Closing Protraction/Retraction 4. Branchial (pharyngeal arch) muscle groups (Muscles of mastication) Muscles of Mastication Masseter, Temporalis, -
27. Veins of the Head and Neck
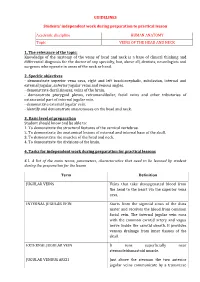
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

7. Internal Jugular Vein the Internal Jugular Vein Is a Large Vein That Receives Blood from the Brain, Face, and Neck
د.احمد فاضل Lecture 16 Anatomy The Root of the Neck The root of the neck can be defined as the area of the neck immediately above the inlet into the thorax. Muscles of the Root of the Neck Scalenus Anterior Muscle Scalenus Medius Muscle The Thoracic Duct The thoracic duct begins in the abdomen at the upper end of the cisterna chyli. It enters the thorax through the aortic opening in the diaphragm and ascends upward, inclining gradually to the left. On reaching the superior mediastinum, it is found passing upward along the left margin of the esophagus. At the root of the neck, it continues to ascend along the left margin of the esophagus until it reaches the level of the transverse process of the seventh cervical vertebra. Here, it bends laterally behind the carotid sheath. On reaching the medial border of the scalenus anterior, it turns 1 downward and drains into the beginning of the left brachiocephalic vein. It may, however, end in the terminal part of the subclavian or internal jugular veins. Main Nerves of the Neck Cervical Plexus Brachial Plexus The brachial plexus is formed in the posterior triangle of the neck by the union of the anterior rami of the 5th, 6th, 7th, and 8th cervical and the first thoracic spinal nerves. This plexus is divided into roots, trunks, divisions, and cords. The roots of C5 and 6 unite to form the upper trunk, the root of C7 continues as the middle trunk, and the roots of C8 and T1 unite to form the lower trunk. -

The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study
brain sciences Article The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study Orhun Mete Cevik 1,2,3 , Murat Imre Usseli 1, Mert Babur 2, Cansu Unal 3,4, Murat Sakir Eksi 1, Mustafa Guduk 1, Talat Cem Ovalioglu 2, Mehmet Emin Aksoy 3 , M. Necmettin Pamir 1 and Baran Bozkurt 1,3,* 1 Department of Neurosurgery, Acıbadem Mehmet Ali Aydinlar University, 34662 Istanbul, Turkey; [email protected] (O.M.C.); [email protected] (M.I.U.); [email protected] (M.S.E.); [email protected] (M.G.); [email protected] (M.N.P.) 2 Department of Neurosurgery, Bakırkoy Training and Research Hospital for Psychiatric and Nervous Diseases, Health Sciences University, 34147 Istanbul, Turkey; [email protected] (M.B.); [email protected] (T.C.O.) 3 (CASE) Center of Advanced Simulation ant Education, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey; [email protected] (C.U.); [email protected] (M.E.A.) 4 School of Medicine, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey * Correspondence: [email protected]; Tel.: +90-533-315-6549 Abstract: Cerebral stroke continues to be one of the leading causes of mortality and long-term morbidity; therefore, carotid endarterectomy (CEA) remains to be a popular treatment for both symptomatic and asymptomatic patients with carotid stenosis. Cranial nerve injuries remain one of the major contributor to the postoperative morbidities. Anatomical dissections were carried out on 44 sides of 22 cadaveric heads following the classical CEA procedure to investigate the variations of the local anatomy as a contributing factor to cranial nerve injuries. -

Tikrit University – Collage of Dentistry Dr.Ban IS Head & Neck Anatomy 2
Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. The Face/part 2: Lec [2] Sensory nerve supply of the face: The trigeminal nerve has three divisions : ophthalmic, maxillary and mandibular. The skin of the face is supplied by the branches of the three divisions of the trigeminal nerve except the skin over the parotid gland and part of the auricle of the ear [lower part medial and lateral surfaces] which supplied by the great auricular nerve. Ophthalmic nerve.. Five cutaneous branches: 1-The lacrimal nerve supplies a small area of skin over the lateral part of the upper lid. 2-The supraorbital nerve indents the bone into a notch or a foramen. The nerve passes up, breaking into several branches which radiate out and supply the forehead and scalp up to the vertex. 1 cden.tu.edu.iq Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. 3-The smaller supratrochlear nerve passes up on the medial side of the supraorbital nerve to supply the middle of the forehead up to the hairline. 4-The infratrochlear nerve supplies skin on the medial part of the upper lid and, passing above the medial palpebral ligament, descends along the side of the external nose, supplying skin over the bridge of the nose. These four branches of the ophthalmic nerve also supply upper lid conjunctiva. 5-The external nasal nerve supplies the middle of the external nose down to the tip. It emerges between the nasal bone and the upper nasal cartilage.