Unusual Venous Drainage of the Common Facial Vein. a Morphologycal Study ORIGINAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

Removal of Periocular Veins by Sclerotherapy
Removal of Periocular Veins by Sclerotherapy David Green, MD Purpose: Prominent periocular veins, especially of the lower eyelid, are not uncommon and patients often seek their removal. Sclerotherapy is a procedure that has been successfully used to permanently remove varicose and telangiectatic veins of the lower extremity and less frequently at other sites. Although it has been successfully used to remove dilated facial veins, it is seldom performed and often not recommended in the periocular region for fear of complications occurring in adjacent structures. The purpose of this study was to determine whether sclerotherapy could safely and effectively eradicate prominent periocular veins. Design: Noncomparative case series. Participants: Fifty adult female patients with prominent periocular veins in the lower eyelid were treated unilaterally. Patients and Methods: Sclerotherapy was performed with a 0.75% solution of sodium tetradecyl sulfate. All patients were followed for at least 12 months after treatment. Main Outcome Measures: Complete clinical disappearance of the treated vein was the criterion for success. Results: All 50 patients were successfully treated with uneventful resorption of their ectatic periocular veins. No patient required a second treatment and there was no evidence of treatment failure at 12 months. No new veins developed at the treated sites and no patient experienced any ophthalmologic or neurologic side effects or complications. Conclusions: Sclerotherapy appears to be a safe and effective means of permanently eradicating periocular veins. Ophthalmology 2001;108:442–448 © 2001 by the American Academy of Ophthalmology. Removal of asymptomatic facial veins, especially periocu- Patients and Materials lar veins, for cosmetic enhancement is a frequent request. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

Port Placement Via the Anterior Jugular Venous System: Case Report, Anatomic Considerations, and Literature Review
Hindawi Case Reports in Radiology Volume 2017, Article ID 2790290, 5 pages https://doi.org/10.1155/2017/2790290 Case Report Port Placement via the Anterior Jugular Venous System: Case Report, Anatomic Considerations, and Literature Review Gernot Rott and Frieder Boecker Radiological Department, Bethesda-Hospital Duisburg, Heerstr. 219, 47053 Duisburg, Germany Correspondence should be addressed to Gernot Rott; [email protected] Received 14 February 2017; Accepted 28 March 2017; Published 10 April 2017 Academic Editor: Dimitrios Tsetis Copyright © 2017 Gernot Rott and Frieder Boecker. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We report on a patient who was referred for port implantation with a two-chamber pacemaker aggregate on the right and total occlusion of the central veins on the left side. Venous access for port implantation was performed via left side puncture of the horizontal segment of the anterior jugular vein system (AJVS) and insertion of the port catheter using a crossover technique from the left to the right venous system via the jugular venous arch (JVA). The clinical significance of the AJVS and the JVA forcentral venous access and port implantation is emphasised and the corresponding literature is reviewed. 1. Introduction left-sided central veins with the presence of a cervical collat- eral venous flow from the left to the right side reaching the Venous access for chest port implantation may be compro- nonoccluded right-sided central veins, specifically the con- mised for a variety of reasons and finding a suitable alter- fluence to the right innominate vein (IV) and, as part of the native can be difficult. -
27. Veins of the Head and Neck
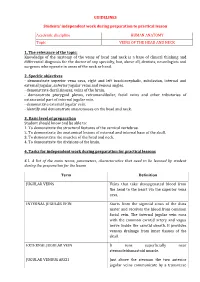
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

New Proposed Classification of Retromandibular Vein Root Variants Based on Cadaver Dissections and Review of Literature – Clinical Implications
ORIGINAL ARTICLE Eur. J. Anat. 24(2): 79-87(2020) New proposed classification of retromandibular vein root variants based on cadaver dissections and review of literature – Clinical implications Sanjoy Sanyal, Sommy M. Joeaneke Department of Anatomical Sciences, All Saints University College of Medicine, Belair, St. Vincent and the Grenadines, West Indies SUMMARY complications. Typically the retro-mandibular vein contributes to formation of common facial and external jugular veins, via its anterior and posterior divisions re- spectively. However, cervico-facial venous variants are rather common. In two successive cadaver dissections the left side of head and neck were unviewable, but the right cervico-facial veins were visible. In both cadavers the right retro-mandibular vein was undivided. The first specimen had right external jugular vein draining into the right subcla- vian vein but did not have a right common facial vein. The second specimen did not have a right external jugular vein, but had a right common faci- al vein draining into the right internal jugular vein. The first variant was characterized as Posterior Dominant Retromandibular Vein with no Common Facial Vein. The second variant was characterized as Anterior Dominant Retromandibular Vein with no External Jugular Vein. Each was sub-classified as Typical or Atypical based on its final drainage pattern. Cervico-facial venous variants often vary from case to case and side to side. Since external jugular and common facial veins are used for clini- cal and surgical interventions, accurate and struc- tured preoperative classification of variations may preclude intra-operative surprises and consequent Graphic 1. Schematic representation of typical RMV formation, division, distribution and drainage. -

The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study
brain sciences Article The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study Orhun Mete Cevik 1,2,3 , Murat Imre Usseli 1, Mert Babur 2, Cansu Unal 3,4, Murat Sakir Eksi 1, Mustafa Guduk 1, Talat Cem Ovalioglu 2, Mehmet Emin Aksoy 3 , M. Necmettin Pamir 1 and Baran Bozkurt 1,3,* 1 Department of Neurosurgery, Acıbadem Mehmet Ali Aydinlar University, 34662 Istanbul, Turkey; [email protected] (O.M.C.); [email protected] (M.I.U.); [email protected] (M.S.E.); [email protected] (M.G.); [email protected] (M.N.P.) 2 Department of Neurosurgery, Bakırkoy Training and Research Hospital for Psychiatric and Nervous Diseases, Health Sciences University, 34147 Istanbul, Turkey; [email protected] (M.B.); [email protected] (T.C.O.) 3 (CASE) Center of Advanced Simulation ant Education, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey; [email protected] (C.U.); [email protected] (M.E.A.) 4 School of Medicine, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey * Correspondence: [email protected]; Tel.: +90-533-315-6549 Abstract: Cerebral stroke continues to be one of the leading causes of mortality and long-term morbidity; therefore, carotid endarterectomy (CEA) remains to be a popular treatment for both symptomatic and asymptomatic patients with carotid stenosis. Cranial nerve injuries remain one of the major contributor to the postoperative morbidities. Anatomical dissections were carried out on 44 sides of 22 cadaveric heads following the classical CEA procedure to investigate the variations of the local anatomy as a contributing factor to cranial nerve injuries. -

Tikrit University – Collage of Dentistry Dr.Ban IS Head & Neck Anatomy 2
Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. The Face/part 2: Lec [2] Sensory nerve supply of the face: The trigeminal nerve has three divisions : ophthalmic, maxillary and mandibular. The skin of the face is supplied by the branches of the three divisions of the trigeminal nerve except the skin over the parotid gland and part of the auricle of the ear [lower part medial and lateral surfaces] which supplied by the great auricular nerve. Ophthalmic nerve.. Five cutaneous branches: 1-The lacrimal nerve supplies a small area of skin over the lateral part of the upper lid. 2-The supraorbital nerve indents the bone into a notch or a foramen. The nerve passes up, breaking into several branches which radiate out and supply the forehead and scalp up to the vertex. 1 cden.tu.edu.iq Tikrit University – collage of dentistry Dr.Ban I.S. head & neck anatomy 2nd y. 3-The smaller supratrochlear nerve passes up on the medial side of the supraorbital nerve to supply the middle of the forehead up to the hairline. 4-The infratrochlear nerve supplies skin on the medial part of the upper lid and, passing above the medial palpebral ligament, descends along the side of the external nose, supplying skin over the bridge of the nose. These four branches of the ophthalmic nerve also supply upper lid conjunctiva. 5-The external nasal nerve supplies the middle of the external nose down to the tip. It emerges between the nasal bone and the upper nasal cartilage. -

Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula
brain sciences Review Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula Justin Dye 1,*, Gary Duckwiler 2, Nestor Gonzalez 3, Naoki Kaneko 2, Robert Goldberg 4, Daniel Rootman 4, Reza Jahan 2, Satoshi Tateshima 2 and Viktor Szeder 2 1 Department of Neurosurgery, Loma Linda University, Loma Linda, CA 92354, USA 2 Division of Interventional Neuroradiology, Department of Radiological Sciences, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (G.D.); [email protected] (N.K.); [email protected] (R.J.); [email protected] (S.T.); [email protected] (V.S.) 3 Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA; [email protected] 4 Department of Ophthalmology, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (R.G.); [email protected] (D.R.) * Correspondence: [email protected]; Tel.: +1-909-558-6338 Received: 16 July 2020; Accepted: 12 August 2020; Published: 14 August 2020 Abstract: Dural arteriovenous fistulas involving the cavernous sinus can lead to orbital pain, vision loss and, in the setting of associated cortical venous reflux, intracranial hemorrhage. The treatment of dural arteriovenous fistulas has primarily become the role of the endovascular surgeon. The venous anatomy surrounding the cavernous sinus and venous sinus thrombosis that is often associated with these fistulas contributes to the complexity of these interventions. The current report gives a detailed description of the alternate endovascular routes to the cavernous sinus based on a single center’s experience as well as a literature review supporting each approach. -

Thyroid Gland- Surgical Anatomy
Thyroid Gland- Surgical Anatomy March 2019 VARSHNEY UG Lecture 1 Bi-lobed gland over 2nd & 3rd tracheal ring Weight : 20 – 30 gr March 2019 VARSHNEY UG Lecture 2 Samuel D. Gross – 1866 , Philadelphia A System of Surgery Thyroid surgery: ‘Horrid butchery’ “No honest and sensible surgeon would ever engage in thyroid surgery” March 2019 VARSHNEY UG Lecture 3 1909 Nobel Prize Theodur Kocher (1841-1917) • Mortality: • 1889 – 2.4% • 1900 – 0.18% • Emphasis on meticulous technique • Performed 5000 cases by death in 1917 March 2019 VARSHNEY UG Lecture 4 Thyroidectomy Neck Release Moraitis, Shaha. JSO 2006 •Open the “gift wrap” •Separate fascia from the muscles •Separate strap muscles •Separate sternomastoid muscle March 2019 VARSHNEY UG Lecture 5 Thyroid Gland moves with deglutition Ligament of Berry (Condensation of Pretracheal fascia) Inferior constrictor- 2 parts Thyropharyngeus {Thyroid cartilage} Cricopharyngeus {Cricoid cartilage} [Contraction – Thyroid and cricoid move up] March 2019 VARSHNEY UG Lecture 6 The thyroid gland is a very vascular structure. Superior thyroid artery (ECA), Inferior thyroid artery ( Thyrocervical trunk) Arteria thyroideaima artery (2-12% ) (innominate, subclavian, right common carotid, internal mammary, or the aortic arch. March 2019 VARSHNEY UG Lecture 7 The superior thyroid vein follows the pathway of the superior thyroid artery. The middle thyroid veins directly flow into the internal jugular vein. The inferior thyroid veins can be found just anterior to the trachea and often anastomose with each other March 2019 VARSHNEY UG Lecture 8 Nerve supply March 2019 VARSHNEY UG Lecture 9 SLN Dissection of the superior thyroid vessels parallel to the vessels on surface of thyroid & exposure of SLN. -

Venous Anatomy of the Cavernous Sinus and Relevant Veins
Journal of Neuroendovascular Therapy Advance Published Date: August 12, 2020 DOI: 10.5797/jnet.ra.2020-0086 Venous Anatomy of the Cavernous Sinus and Relevant Veins Shuichi Tanoue,1 Masaru Hirohata,2 Yasuharu Takeuchi,2 Kimihiko Orito,2 Sosho Kajiwara,2 and Toshi Abe1 The cavernous sinus (CS) is a dural sinus located on each side of the pituitary fossa. Neoplastic and vascular lesions, such as arteriovenous fistulas, frequently involve the CS. This sinus plays a role as a crossroad receiving venous blood flow from the facial, orbital, meningeal, and neural venous tributaries. The relationship between these surrounding relevant veins and the CS, as well as the CS itself, varies anatomically. For safe and effective surgical and endovascular treatment of lesions involving the CS, knowledge of the anatomy and variations of the CS and the relevant surrounding veins is highly important. In this section, the anatomy and variations of the CS and the relevant surrounding veins are outlined. Keywords▶ cavernous sinus, laterocavernous sinus, anatomy, relevant veins Introduction this section, the functions and imaging anatomy of the CS and relevant surrounding veins are reviewed. The cavernous sinus (CS) is the dural sinus that lies on the bilateral sides of the pituitary fossa of the sphenoidal body. Basis Anatomy of the CS and It functions as a venous channel receiving many types of Its Variations venous structures, including facial and orbital veins, men- ingeal veins, pituitary veins, and cerebral superficial and Basic anatomy deep veins. These surrounding venous structures present The CS is a dural sinus located between the superior orbital complex anatomy, and the CS can be affected by neo- fissure and the petrous apex of the temporal bone at the plasms and vascular disease. -

Posterior Mediastinum: Mediastinal Organs 275
104750_S_265_290_Kap_4:_ 05.01.2010 10:43 Uhr Seite 275 Posterior Mediastinum: Mediastinal Organs 275 1 Internal jugular vein 2 Right vagus nerve 3 Thyroid gland 4 Right recurrent laryngeal nerve 5 Brachiocephalic trunk 6 Trachea 7 Bifurcation of trachea 8 Right phrenic nerve 9 Inferior vena cava 10 Diaphragm 11 Left subclavian artery 12 Left common carotid artery 13 Left vagus nerve 14 Aortic arch 15 Esophagus 16 Esophageal plexus 17 Thoracic aorta 18 Left phrenic nerve 19 Pericardium at the central tendon of diaphragm 20 Right pulmonary artery 21 Left pulmonary artery 22 Tracheal lymph nodes 23 Superior tracheobronchial lymph nodes 24 Bronchopulmonary lymph nodes Bronchial tree in situ (ventral aspect). Heart and pericardium have been removed; the bronchi of the bronchopulmonary segments are dissected. 1–10 = numbers of segments (cf. p. 246 and 251). 15 12 22 6 11 5 2 1 14 2 23 1 3 21 3 20 24 4 5 4 17 8 5 6 6 15 8 7 8 9 9 10 10 Relation of aorta, pulmonary trunk, and esophagus to trachea and bronchial tree (schematic drawing). 1–10 = numbers of segments (cf. p. 246 and 251). 104750_S_265_290_Kap_4:_ 05.01.2010 10:43 Uhr Seite 276 276 Posterior Mediastinum: Mediastinal Organs Mediastinal organs (ventral aspect). The heart with the pericardium has been removed, and the lungs and aortic arch have been slightly reflected to show the vagus nerves and their branches. 1 Supraclavicular nerves 12 Right pulmonary artery 24 Left vagus nerve 2 Right internal jugular vein with ansa cervicalis 13 Right pulmonary veins 25 Left common carotid artery