Anatomic Variability in the Relation Between the Retromandibular Vein and the Facial Nerve: a Case Report, Literature Review and Classification
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Should We Report Posterior Fossa Emissary Veins?
Diagn Interv Radiol 2014; 20:78–81 NEURORADIOLOGY © Turkish Society of Radiology 2014 PICTORIAL ESSAY Why should we report posterior fossa emissary veins? Yeliz Pekçevik, Rıdvan Pekçevik ABSTRACT osterior fossa emissary veins pass through cranial apertures and par- Posterior fossa emissary veins are valveless veins that pass ticipate in extracranial venous drainage of the posterior fossa dural through cranial apertures. They participate in extracranial ve- sinuses. These emissary veins are usually small and asymptomatic nous drainage of the posterior fossa dural sinuses. The mas- P toid emissary vein, condylar veins, occipital emissary vein, in healthy people. They protect the brain from increases in intracranial and petrosquamosal sinus are the major posterior fossa emis- pressure in patients with lesions of the neck or skull base and obstructed sary veins. We believe that posterior fossa emissary veins can internal jugular veins (1). They also help to cool venous blood circulat- be detected by radiologists before surgery with a thorough understanding of their anatomy. Describing them using tem- ing through cephalic structures (2). Emissary veins may be enlarged in poral bone computed tomography (CT), CT angiography, patients with high-flow vascular malformations or severe hypoplasia or and cerebral magnetic resonance (MR) venography exam- inations results in more detailed and accurate preoperative aplasia of the jugular veins. They are associated with craniofacial syn- radiological interpretation and has clinical importance. This dromes (1, 3). Dilated emissary veins may cause tinnitus (4, 5). pictorial essay reviews the anatomy of the major and clini- We aim to emphasize the importance of reporting posterior fossa em- cally relevant posterior fossa emissary veins using high-reso- lution CT, CT angiography, and MR venography images and issary veins prior to surgeries that are related to the posterior fossa and discusses the clinical importance of reporting these vascular mastoid region. -

Venous Arrangement of the Head and Neck in Humans – Anatomic Variability and Its Clinical Inferences
Original article http://dx.doi.org/10.4322/jms.093815 Venous arrangement of the head and neck in humans – anatomic variability and its clinical inferences SILVA, M. R. M. A.1*, HENRIQUES, J. G. B.1, SILVA, J. H.1, CAMARGOS, V. R.2 and MOREIRA, P. R.1 1Department of Morphology, Institute of Biological Sciences, Universidade Federal de Minas Gerais – UFMG, Av. Antonio Carlos, 6627, CEP 31920-000, Belo Horizonte, MG, Brazil 2Centro Universitário de Belo Horizonte – UniBH, Rua Diamantina, 567, Lagoinha, CEP 31110-320, Belo Horizonte, MG, Brazil *E-mail: [email protected] Abstract Introduction: The knowledge of morphological variations of the veins of the head and neck is essential for health professionals, both for diagnostic procedures as for clinical and surgical planning. This study described changes in the following structures: retromandibular vein and its divisions, including the relationship with the facial nerve, facial vein, common facial vein and jugular veins. Material and Methods: The variations of the veins were analyzed in three heads, five hemi-heads (right side) and two hemi-heads (left side) of unknown age and sex. Results: The changes only on the right side of the face were: union between the superficial temporal and maxillary veins at a lower level; absence of the common facial vein and facial vein draining into the external jugular vein. While on the left, only, it was noted: posterior division of retromandibular, after unite with the common facial vein, led to the internal jugular vein; union between the posterior auricular and common facial veins to form the external jugular and union between posterior auricular and common facial veins to terminate into internal jugular. -

The Mandibular Landmarks About the Facial Artery and Vein With
Int. J. Morphol., 30(2):504-509, 2012. The Mandibular Landmarks about the Facial Artery and Vein with Multidetector Computed Tomography Angiography (MDCTA): an Anatomical and Radiological Morphometric Study Puntos de Referencia de la Mandíbula Relacionados a la Arteria y Vena Facial con Angiografía por Tomografía Computarizada Multidetector (ATCM): un Estudio Morfométrico Anatómico y Radiológico *Aynur Emine Cicekcibasi; *Mehmet Tugrul Yılmaz; **Demet Kıresi & *Muzaffer Seker CICEKCIBASI, A. E.; YILMAZ, M. T.; KIRESI, D. & SEKER, M. The mandibular landmarks about the facial artery and vein with multidetector computed tomography angiography (MDCTA): an anatomical and radiological morphometric study. Int. J. Morphol., 30(2):504-509, 2012. SUMMARY: The aim of this study was to investigate the course of the facial vessels according to several mandibular landmarks in living individuals using multidetector computed tomography angiography (MDCTA) to determine these related to sex and side. This study was conducted in the Radiology Department, Meram Faculty of Medicine, Necmettin Erbakan University (Konya, Turkey). In total, sixty faces from 30 specimens (15 males and 15 females) with symptoms and signs of vascular disease were evaluated for the facial vessels by MDCTA scan. The facial vessel parameters were measured according to the reference points (mandibular angle, mental protuberance, mental foramen and facial midline). The distance from the point at which the facial artery first appears in the lower margin of the mandible to the mandibular angle for right and left facial artery were observed as 3.53±0.66 cm and 3.31±0.73 cm in males, respectively. These distances were determined as 2.91±0.52 cm and 3.35±0.48 cm in females. -

Removal of Periocular Veins by Sclerotherapy
Removal of Periocular Veins by Sclerotherapy David Green, MD Purpose: Prominent periocular veins, especially of the lower eyelid, are not uncommon and patients often seek their removal. Sclerotherapy is a procedure that has been successfully used to permanently remove varicose and telangiectatic veins of the lower extremity and less frequently at other sites. Although it has been successfully used to remove dilated facial veins, it is seldom performed and often not recommended in the periocular region for fear of complications occurring in adjacent structures. The purpose of this study was to determine whether sclerotherapy could safely and effectively eradicate prominent periocular veins. Design: Noncomparative case series. Participants: Fifty adult female patients with prominent periocular veins in the lower eyelid were treated unilaterally. Patients and Methods: Sclerotherapy was performed with a 0.75% solution of sodium tetradecyl sulfate. All patients were followed for at least 12 months after treatment. Main Outcome Measures: Complete clinical disappearance of the treated vein was the criterion for success. Results: All 50 patients were successfully treated with uneventful resorption of their ectatic periocular veins. No patient required a second treatment and there was no evidence of treatment failure at 12 months. No new veins developed at the treated sites and no patient experienced any ophthalmologic or neurologic side effects or complications. Conclusions: Sclerotherapy appears to be a safe and effective means of permanently eradicating periocular veins. Ophthalmology 2001;108:442–448 © 2001 by the American Academy of Ophthalmology. Removal of asymptomatic facial veins, especially periocu- Patients and Materials lar veins, for cosmetic enhancement is a frequent request. -

Redalyc.Termination of the Facial Vein Into the External Jugular Vein: An
Jornal Vascular Brasileiro ISSN: 1677-5449 [email protected] Sociedade Brasileira de Angiologia e de Cirurgia Vascular Brasil D'Silva, Suhani Sumalatha; Pulakunta, Thejodhar; Potu, Bhagath Kumar Termination of the facial vein into the external jugular vein: an anatomical variation Jornal Vascular Brasileiro, vol. 7, núm. 2, junio, 2008, pp. 174-175 Sociedade Brasileira de Angiologia e de Cirurgia Vascular São Paulo, Brasil Available in: http://www.redalyc.org/articulo.oa?id=245016526015 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative CASE REPORT Termination of the facial vein into the external jugular vein: an anatomical variation Terminação da veia facial na veia jugular externa: uma variação anatômica Suhani Sumalatha D’Silva, Thejodhar Pulakunta, Bhagath Kumar Potu* Abstract Resumo Different patterns of variations in the venous drainage have been Padrões distintos de variações na drenagem venosa já foram observed in the past. During routine dissection in our Department of observados. Durante a dissecção de rotina em nosso Departamento Anatomy, an unusual drainage pattern of the veins of the left side of de Anatomia, observou-se um padrão incomum de drenagem das veias the face of a middle aged cadaver was observed. The facial vein do lado esquerdo da face de um cadáver de meia idade. A veia facial presented a normal course from its origin up to the base of mandible, apresentava curso normal de sua origem até a base da mandíbula, e and then it crossed the base of mandible posteriorly to the facial artery. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

PAROTIDECTOMY Johan Fagan
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY PAROTIDECTOMY Johan Fagan The facial nerve is central to parotid Structures that traverse, or are found surgery for both surgeon and patient. within the parotid gland Knowledge of the surgical anatomy and the landmarks to find the facial nerve are • Facial nerve and branches (Figure 1) the key to preserving facial nerve function. • External carotid artery: It gives off the Surgical Anatomy transverse facial artery inside the gland before dividing into the internal maxil- Parotid gland lary and the superficial temporal arteries (Figure 2). The parotid glands are situated anteriorly and inferiorly to the ear. They overlie the vertical mandibular rami and masseter muscles, behind which they extend into the retromandibular sulci. The glands extend superiorly from the zygomatic arches and inferiorly to below the angles of the mandible where they overlie the posterior bellies of the digastric and the sternoclei- domastoid muscles. The parotid duct exits the gland anteriorly, crosses the masseter muscle, curves medially around its anterior margin, pierces the buccinator muscle, and Figure 1: Main branches of facial nerve enters the mouth opposite the 2nd upper molar tooth. Superficial Muscular Aponeurotic System and Parotid Fascia The Superficial Muscular Aponeurotic System (SMAS) is a fibrous network that invests the facial muscles and connects them with the dermis. It is continuous with the platysma inferiorly; superiorly it at- taches to the zygomatic arch. In the lower face, the facial nerve courses deep to the SMAS and the platysma. The parotid Figure 2: Branches of the external carotid glands are contained within two layers of artery parotid fascia, which extend from the zygoma above and continue as cervical • Veins: The maxillary and superficial fascia below. -

A Rare Case Report of Lemierre Syndrome from the Anterior Jugular Vein
CASE REPORT A Rare Case Report of Lemierre Syndrome from the Anterior Jugular Vein Nima Rejali, DO* *Hackensack University Medical Center, Department of Emergency Medicine, Marissa Heyer, BA† Hackensack, New Jersey Doug Finefrock, DO*† †Hackensack Meridian School of Medicine, Department of Emergency Medicine, Hackensack, New Jersey Section Editor: Rick A. McPheeters, DO Submission history: Submitted March 27, 2020; Revision received June 14, 2020; Accepted July 3, 2020 Electronically published August 3, 2020 Full text available through open access at http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2020.7.47442 Introduction: Lemierre syndrome is a rare, potentially fatal, septic thrombophlebitis of the internal jugular vein. Treatment includes intravenous antibiotics for Fusobacterium necrophorum, the most common pathogen, as well as consideration for anticoagulation therapy. Case Report: A 27-year-old female presented with left-sided neck swelling and erythema. Computed tomography noted left anterior jugular vein thrombophlebitis and multiple cavitating foci, consistent with septic emboli. We report a rare case of Lemierre syndrome in which the thrombus was found in the anterior jugular vein, as opposed to the much larger internal jugular vein more traditionally associated with creating septic emboli. Conclusion: Based on an individual’s clinical symptoms, history, and radiologic findings, it is important for physicians to consider Lemierre syndrome in the differential diagnosis, as the condition may rapidly progress to septic shock and death if not treated promptly. The use of anticoagulation therapy remains controversial, and there is a lack of established standard care because the syndrome is so rare. [Clin Pract Cases Emerg Med. 2020;4(3):454–457.] Keywords: Sepsis; septic emboli; thrombophlebitis; case report; Lemierre. -

Temporal Regions and Ear
Unit 16: Temporal regions and ear GENERAL OBJECTIVES: - general considerations of the organization of layers in parotid and temporal/infratemporal regions - muscles of mastication and TMJ - structure and function of the ear - irrigation and innervations of parotid, temporal/infratemporal regions SPECIFIC OBJECTIVES: 1. Parotid region Boundaries (Parotid Bed): Sup., Inf., Ant., Post.. Med. (Styloid Process), Lat. (Superficial Fascia with Great Auricular Nerve) Contents: Parotid Fascia (continuous with Investing Fascia) Parotid Gland: Position, Parts, Parotid Duct Structures within the Gland: Ext. Carotid Artery -> Terminal Branches Retromandibular Vein -> Anterior & Posterior Branches Parotid Lymph Nodes Facial Nerve -> 5 Terminal Branches 2. Temporal and infratemporal regions Boundaries and contents: Spenomandibular Ligament Pterygoid Muscles (Lateral & Medial) Maxillary Artery (1st., 2nd. & 3rd. Parts) Branches: Middle Meningeal (Extracranial Course) Others Pterygoid Venous Plexus & Communications Mandibular Nerve (V3): Ant. & Post. Divisions Branches: Muscular, Buccal & Auriculotemporal Nerves Inferior Alveolar & Lingual Nerves Chorda Tympani Otic Ganglion (Parasympathetic) 3. Temporomandibular Joint Articular Surfaces Capsule & Ligaments, Sphenomandibular Ligament Articular Disc (2 separate joint cavities & movements) Movements of the T.M.J.: [(i) Rotation, (ii) Anterior Gliding] -> Opening/Closing Protraction/Retraction 4. Branchial (pharyngeal arch) muscle groups (Muscles of mastication) Muscles of Mastication Masseter, Temporalis, -
27. Veins of the Head and Neck
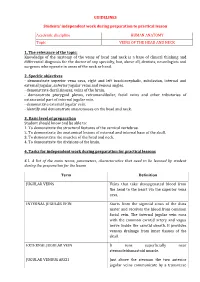
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

New Proposed Classification of Retromandibular Vein Root Variants Based on Cadaver Dissections and Review of Literature – Clinical Implications
ORIGINAL ARTICLE Eur. J. Anat. 24(2): 79-87(2020) New proposed classification of retromandibular vein root variants based on cadaver dissections and review of literature – Clinical implications Sanjoy Sanyal, Sommy M. Joeaneke Department of Anatomical Sciences, All Saints University College of Medicine, Belair, St. Vincent and the Grenadines, West Indies SUMMARY complications. Typically the retro-mandibular vein contributes to formation of common facial and external jugular veins, via its anterior and posterior divisions re- spectively. However, cervico-facial venous variants are rather common. In two successive cadaver dissections the left side of head and neck were unviewable, but the right cervico-facial veins were visible. In both cadavers the right retro-mandibular vein was undivided. The first specimen had right external jugular vein draining into the right subcla- vian vein but did not have a right common facial vein. The second specimen did not have a right external jugular vein, but had a right common faci- al vein draining into the right internal jugular vein. The first variant was characterized as Posterior Dominant Retromandibular Vein with no Common Facial Vein. The second variant was characterized as Anterior Dominant Retromandibular Vein with no External Jugular Vein. Each was sub-classified as Typical or Atypical based on its final drainage pattern. Cervico-facial venous variants often vary from case to case and side to side. Since external jugular and common facial veins are used for clini- cal and surgical interventions, accurate and struc- tured preoperative classification of variations may preclude intra-operative surprises and consequent Graphic 1. Schematic representation of typical RMV formation, division, distribution and drainage. -

7. Internal Jugular Vein the Internal Jugular Vein Is a Large Vein That Receives Blood from the Brain, Face, and Neck
د.احمد فاضل Lecture 16 Anatomy The Root of the Neck The root of the neck can be defined as the area of the neck immediately above the inlet into the thorax. Muscles of the Root of the Neck Scalenus Anterior Muscle Scalenus Medius Muscle The Thoracic Duct The thoracic duct begins in the abdomen at the upper end of the cisterna chyli. It enters the thorax through the aortic opening in the diaphragm and ascends upward, inclining gradually to the left. On reaching the superior mediastinum, it is found passing upward along the left margin of the esophagus. At the root of the neck, it continues to ascend along the left margin of the esophagus until it reaches the level of the transverse process of the seventh cervical vertebra. Here, it bends laterally behind the carotid sheath. On reaching the medial border of the scalenus anterior, it turns 1 downward and drains into the beginning of the left brachiocephalic vein. It may, however, end in the terminal part of the subclavian or internal jugular veins. Main Nerves of the Neck Cervical Plexus Brachial Plexus The brachial plexus is formed in the posterior triangle of the neck by the union of the anterior rami of the 5th, 6th, 7th, and 8th cervical and the first thoracic spinal nerves. This plexus is divided into roots, trunks, divisions, and cords. The roots of C5 and 6 unite to form the upper trunk, the root of C7 continues as the middle trunk, and the roots of C8 and T1 unite to form the lower trunk.