Topic № 1. the Subject Operative Surgery. the Main Principles of Operations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Splenic Artery Embolization for the Treatment of Gastric Variceal Bleeding Secondary to Splenic Vein Thrombosis Complicated by Necrotizing Pancreatitis: Report of a Case
Hindawi Publishing Corporation Case Reports in Medicine Volume 2016, Article ID 1585926, 6 pages http://dx.doi.org/10.1155/2016/1585926 Case Report Splenic Artery Embolization for the Treatment of Gastric Variceal Bleeding Secondary to Splenic Vein Thrombosis Complicated by Necrotizing Pancreatitis: Report of a Case Hee Joon Kim, Eun Kyu Park, Young Hoe Hur, Yang Seok Koh, and Chol Kyoon Cho Department of Surgery, Chonnam National University Medical School, Gwangju, Republic of Korea Correspondence should be addressed to Chol Kyoon Cho; [email protected] Received 11 August 2016; Accepted 1 November 2016 Academic Editor: Omer Faruk Dogan Copyright © 2016 Hee Joon Kim et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Splenic vein thrombosis is a relatively common finding in pancreatitis. Gastric variceal bleeding is a life-threatening complication of splenic vein thrombosis, resulting from increased blood flow to short gastric vein. Traditionally, splenectomy is considered the treatment of choice. However, surgery in necrotizing pancreatitis is dangerous, because of severe inflammation, adhesion, and bleeding tendency. In the Warshaw operation, gastric variceal bleeding is rare, even though splenic vein is resected. Because the splenic artery is also resected, blood flow to short gastric vein is not increased problematically. Herein, we report a case of gastric variceal bleeding secondary to splenic vein thrombosis complicated by necrotizing pancreatitis successfully treated with splenic artery embolization. Splenic artery embolization could be the best treatment option for gastric variceal bleeding when splenectomy is difficult such as in case associated with severe acute pancreatitis or associated with severe adhesion or in patients withhigh operation risk. -

Diseases of Salivary Glands: Review
ISSN: 1812–1217 Diseases of Salivary Glands: Review Alhan D Al-Moula Department of Dental Basic Science BDS, MSc (Assist Lect) College of Dentistry, University of Mosul اخلﻻضة امخجوًف امفموي تُئة رطبة، حتخوي ػىل طبلة ركِلة من امسائل ثدغى انوؼاب ثغطي امسطوح ادلاخوَة و متﻷ امفراغات تني ااطَة امفموًة و اﻷس نان. انوؼاب سائل مؼلد، ًنذج من امغدد انوؼاتَة، اذلي ًوؼة دورا" ىاما" يف اﶈافظة ػىل سﻻمة امفم. املرىض اذلٍن ؼًاهون من هلص يف اﻷفراز انوؼايب حكون دلهيم مشبلك يف اﻷلك، امخحدث، و امبوع و ًطبحون غرضة مﻷههتاابت يف اﻷغش َة ااطَة و امنخر املندرش يف اﻷس نان. ًوخد ثﻻثة أزواج من امغدد انوؼاتَة ام ئرُسة – امغدة امنكفِة، امغدة حتت امفكِة، و حتت انوساهَة، موضؼيا ٍكون خارج امخجوًف امفموي، يف حمفظة و ميخد هظاهما املنَوي مَفرغ افرازاهتا. وًوخد أًضا" امؼدًد من امغدد انوؼاتَة امطغرية ، انوساهَة، اتحنكِة، ادلىوزيًة، انوساهَة احلنكِة وما كبل امرخوًة، ٍكون موضؼيا مﻷسفل و مضن امغشاء ااطي، غري حماطة مبحفظة مع هجاز كنَوي كطري. افرازات امغدد انوؼاتَة ام ئرُسة مُست مدشاهبة. امغدة امفكِة ثفرز مؼاب مطيل غين ابﻷمِﻻز، وامغدة حتت امفكِة ثنذج مؼاب غين اباط، أما امغدة حتت انوساهَة ثنذج مؼااب" مزخا". ثبؼا" ميذه اﻷخذﻻفات، انوؼاب املوحود يق امفم ٌشار امَو مكزجي. ح كرَة املزجي انوؼايب مُس ثس َطا" واملادة اﻷضافِة اموػة من لك املفرزات انوؼاتَة، اكمؼدًد من امربوثُنات ثنذلل ثرسػة وثوخطق هبدروكس َل اﻷتُذاًت مﻷس نان و سطوح ااطَة امفموًة. ثبدأ أمراض امغدد انوؼاتَة ػادة تخغريات اندرة يف املفرزات و ام كرتَة، وىذه امخغريات ثؤثر اثهواي" من خﻻل جشلك انووحية اجلرثومِة و املوح، اميت تدورىا ثؤدي اىل خنور مذفش َة وأمراض وس َج دامعة. ىذه اﻷمراض ميكن أن ثطبح شدًدة تؼد املؼاجلة امشؼاغَة ﻷن امؼدًد من احلاﻻت اجليازًة )مثل امسكري، امخوَف اهكُيس( ثؤثر يف اجلراين انوؼايب، و ٌش خيك املرض من حفاف يف امفم. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

Anatomical Variants in the Termination of the Cephalic Vein Stoyan Novakov1*, Elena Krasteva2
Institute of Experimental Morphology, Pathology and Anthropology with Museum Bulgarian Anatomical Society Acta morphologica et anthropologica, 25 (3-4) Sofia • 2018 Anatomical Variants in the Termination of the Cephalic Vein Stoyan Novakov1*, Elena Krasteva2 1 Department of Anatomy, Histology and Embryology, 2Department of Propaedeutics of Surgical Di- seases, Medical Faculty, Medical University of Plovdiv * Corresponding author e-mail: [email protected] Jugulocephalic vein is atavistic structure which is very rare. The low incidence of the variations of the cephalic vein in deltopectoral triangle and its position on the anterior surface of the clavicle and the neck doesn’t make it less important for the clinical practice. Phylo- and ontogenesis explain the formation of the above mentioned variations. We followed the pattern of the cephalic vein in its proximal part and termination to describe possible variations. In this long term study on 140 upper limbs of 70 cadavers, 4 or 2,9% of the cephalic veins were variable. The direct empting of the cephalic vein into internal jugular is an exception with few descriptions at the moment. The rareness of this anatomical variation doesn’t make it less important for clinical practice. It is described as a possible obstacle in catheter implantation, clavicle fractures and creation of arteriovenous fistula in patients on hemodialysis. Key words:cadavers, human anatomy variation, cephalic vein, external jugular vein, jugulocephalic vein Introduction Cephalic vein (CV) belongs to the group of superficial veins of the upper limb. It usually forms over the anatomical snuff-box on the radial side of the wrist from the radial end of the dorsal venous plexus. -

Brachium and Cubital Fossa
Anatomy Guy Dissection Sheet 1/15/2012 Brachium and Cubital Fossa Dr. Craig Goodmurphy Anatomy Guy Major Dissection Objectives – Anterior Compartment 1. Maintain the superficial veins but work the fascia of the brachium off the anterior compartment noting the intermuscular septae 2. Clean and identify the three muscle of the anterior arm and their attachments 3. Mobilize the contents of the brachial fascia as it extends from the axillary fascia to the elbow noting the median, ulnar and medial brachial and medial antebrachial cutaneous nerves 4. Follow the musculocutaneous nerve as it passes through the coracobrachialis and between the biceps and brachialis noting motor branches and the lateral antebrachial cutaneous nerve Major Dissection Objectives – Cubital Fossa & Posterior Compartment 6. Mobilize the cubital fossa veins and review the boundaries 7. Clean the biceps tendon and reflect the aponeurosis 8. Locate the contents of the fossa including the bifurcation of the brachial artery, median nerve and floor muscles 9. Have a partner elevate the arm to dissect posteriorly and remove the skin and fascia 10. Locate the three heads of the triceps and their attachments 11. Locate the profunda brachii artery and radial nerve at the triangular interval and between the brachialis and brachioradialis muscles Eastern Virginia Medical School 1 Anatomy Guy Dissection Sheet 1/15/2012 Brachium and Cubital Fossa Pearls & Problems Don’t 1. Cut the biceps muscle just mobilize it Do 2. Follow the cords and tubes from known to unknown as you clean them Do 3. Remove the duplicated deep veins but save the unpaired superficial veins Do 4. -
Anatomical Overview
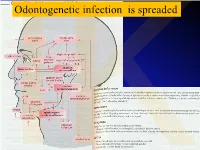
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

The Anatomy of Th-E Blood Vascular System of the Fox ,Squirrel
THE ANATOMY OF TH-E BLOOD VASCULAR SYSTEM OF THE FOX ,SQUIRREL. §CIURUS NlGER. .RUFIVENTEB (OEOEEROY) Thai: for the 009m of M. S. MICHIGAN STATE COLLEGE Thomas William Jenkins 1950 THulS' ifliillifllfllilllljllljIi\Ill\ljilllHliLlilHlLHl This is to certifg that the thesis entitled The Anatomy of the Blood Vascular System of the Fox Squirrel. Sciurus niger rufiventer (Geoffroy) presented by Thomas William Jenkins has been accepted towards fulfillment of the requirements for A degree in MEL Major professor Date May 23’ 19500 0-169 q/m Np” THE ANATOMY OF THE BLOOD VASCULAR SYSTEM OF THE FOX SQUIRREL, SCIURUS NIGER RUFIVENTER (GEOFFROY) By THOMAS WILLIAM JENKINS w L-Ooffi A THESIS Submitted to the School of Graduate Studies of Michigan State College of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Department of Zoology 1950 \ THESlSfi ACKNOWLEDGMENTS Grateful acknowledgment is made to the following persons of the Zoology Department: Dr. R. A. Fennell, under whose guidence this study was completed; Mr. P. A. Caraway, for his invaluable assistance in photography; Dr. D. W. Hayne and Mr. Poff, for their assistance in trapping; Dr. K. A. Stiles and Dr. R. H. Manville, for their helpful suggestions on various occasions; Mrs. Bernadette Henderson (Miss Mac), for her pleasant words of encouragement and advice; Dr. H. R. Hunt, head of the Zoology Department, for approval of the research problem; and Mr. N. J. Mizeres, for critically reading the manuscript. Special thanks is given to my wife for her assistance with the drawings and constant encouragement throughout the many months of work. -

Variant Origins of Arteries in the Carotid Triangle - a Case Report
Case Report 281 Variant Origins of Arteries in the Carotid Triangle - A Case Report B. V. Murlimanju, MD; Latha V. Prabhu, MS; Mangala M. Pai, MD; Dhanya Jayaprakash, MBBS; Vasudha V. Saralaya, MS The left superior laryngeal artery was observed arising from the external carotid artery instead of the superior thyroid artery in the cadaver of an approximately 70 year-old Asian man. In addition, on the same side, the superior thyroid artery arose from the common carotid artery 2 cm before the bifurcation instead of its usual origin from the external carotid artery. From the external carotid artery, the lingual and facial arteries arose from the com- mon linguofacial trunk. The nerves in the carotid triangle were normal in course. No varia- tions were observed on the right side carotid system. The multiple variations in this case have not been previously described. The embryogenesis of this combination of variations is not clear, but the anatomic consequences may have important clinical implications. As angiography has gained popularity in diagnostic approaches in recent years, it is essential to be aware of these variations so that they are not overlooked in differential diagnoses. (Chang Gung Med J 2012;35:281-4) Key words: artery, superior laryngeal, superior thyroid, common carotid, external carotid, vari- ant origin natomical variations in the carotid triangle in the STA from the left CCA is reported here. In the Athe neck are important, especially during surgi- literature, a few variations in origin have been cal and radiological intervention in the region. reported for both arteries,(1-3) but the combination of Normally, the superior laryngeal artery (SLA) is a variations reported in this case has not been previ- branch of the superior thyroid artery (STA). -

Arteries and Veins) of the Gastrointestinal System (Oesophagus to Anus)
2021 First Sitting Paper 1 Question 07 2021-1-07 Outline the anatomy of the blood supply (arteries and veins) of the gastrointestinal system (oesophagus to anus) Portal circulatory system + arterial blood flow into liver 1100ml of portal blood + 400ml from hepatic artery = 1500ml (30% CO) Oxygen consumption – 20-35% of total body needs Arterial Supply Abdominal Aorta • It begins at the aortic hiatus of the diaphragm, anterior to the lower border of vertebra T7. • It descends to the level of vertebra L4 it is slightly to the left of midline. • The terminal branches of the abdominal aorta are the two common iliac arteries. Branches of Abdominal Aorta Visceral Branches Parietal Branches Celiac. Inferior Phrenics. Superior Mesenteric. Lumbars Inferior Mesenteric. Middle Sacral. Middle Suprarenals. Renals. Internal Spermatics. Gonadal Anterior Branches of The Abdominal Aorta • Celiac Artery. Superior Mesenteric Artery. Inferior Mesenteric Artery. • The three anterior branches supply the gastrointestinal viscera. Basic Concept • Fore Gut - Coeliac Trunk • Mid Gut - Superior Mesenteric Artery • Hind Gut - Inferior Mesenteric Artery Celiac Trunk • It arises from the abdominal aorta immediately below the aortic hiatus of the diaphragm anterior to the upper part of vertebra LI. • It divides into the: left gastric artery, splenic artery, common hepatic artery. o Left gastric artery o Splenic artery ▪ Short gastric vessels ▪ Lt. gastroepiploic artery o Common hepatic artery ▪ Hepatic artery proper JC 2019 2021 First Sitting Paper 1 Question 07 • Left hepatic artery • Right hepatic artery ▪ Gastroduodenal artery • Rt. Gastroepiploic (gastro-omental) artery • Sup pancreatoduodenal artery • Supraduodenal artery Oesophagus • Cervical oesophagus - branches from inferior thyroid artery • Thoracic oesophagus - branches from bronchial arteries and aorta • Abd. -

Elbow Checklist
Workbook Musculoskeletal Ultrasound September 26, 2013 Shoulder Checklist Long biceps tendon Patient position: Facing the examiner Shoulder in slight medial rotation; elbow in flexion and supination Plane/ region: Transverse (axial): from a) intraarticular portion to b) myotendinous junction (at level of the pectoralis major tendon). What you will see: Long head of the biceps tendon Supraspinatus tendon Transverse humeral ligament Subscapularis tendon Lesser tuberosity Greater tuberosity Short head of the biceps Long head of the biceps (musculotendinous junction) Humeral shaft Pectoralis major tendon Plane/ region: Logitudinal (sagittal): What you will see: Long head of biceps; fibrillar structure Lesser tuberosity Long head of the biceps tendon Notes: Subscapularis muscle and tendon Patient position: Facing the examiner Shoulder in lateral rotation; elbow in flexion/ supination Plane/ region: longitudinal (axial): full vertical width of tendon. What you will see: Subscapularis muscle, tendon, and insertion Supraspinatus tendon Coracoid process Deltoid Greater tuberosity Lesser tuberosity Notes: Do passive medial/ lateral rotation while examining Plane/ region: Transverse (sagittal): What you will see: Lesser tuberosity Fascicles of subscapularis tendon Supraspinatus tendon Patient position: Lateral to examiner Shoulder in extension and medial rotation Hand on ipsilateral buttock Plane/ region: Longitudinal (oblique sagittal) Identify the intra-articular portion of biceps LH in the transverse plane; then -

The Square Flap Technique for Burn Contractures: Clinical Experience and Analysis of Length Gain
Annals of Burns and Fire Disasters - vol. XXXI - n. 4 - December 2018 THE SQUARE FLAP TECHNIQUE FOR BURN CONTRACTURES: CLINICAL EXPERIENCE AND ANALYSIS OF LENGTH GAIN DOUBLE LAMBEAU RHOMBOÏDE POUR BRIDE SÉQUELLAIRE DE BRÛ- LURE: EXPÉRIENCE PRATIQUE ET ANALYSE DE LA LONGUEUR GAGNÉE Hifny M.A. Department of Plastic Surgery, Faculty of Medicine, Qena University Hospital, South Valley University, Egypt SUMMARY. Post-burn contractures, affecting the joints especially, are demanding problems. Many surgical techniques have been designated for burn contracture release. The aim of this study is to investigate the efficiency of the square flap technique to release a post-burn scar contracture, and assess the post-operative length gain that can be achieved by simple mathematical calculation. In this study, sixteen patients with linear contracture bands were treated with the square flap tech- nique. The anatomical distribution of the contractures was: axilla, cubital fossa, flank, perineum and popliteal fossa. Scar maturity ranged from 4 months - 9 years. Square flap width and contracture band length before and immediately after surgery were recorded by simple mathematical calculation. Flap complication was assessed. Patient satisfaction was also assessed during the follow-up period. All square flaps were effective in lengthening the contracture bands. The length of the contracture that was released ranged from 2 to 6 cm. The gain in length provided with this technique ranged from 212 to 350%, average 247%, and adequate contracture release was achieved in all cases postoperatively. All square flaps healed uneventfully except for one (6%), which demonstrated limited epidermolysis that healed by secondary intention. The fol- low-up interval ranged from 6 months to 1.5 years. -

Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions
Int. J. Morphol., 34(3):1063-1068, 2016. Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions Topografía Infraclavicular de los Fascículos del Plexo Braquial en Diferentes Posiciones del Miembro Superior Daniel Alves dos Santos*; Amilton Iatecola*; Cesar Adriano Dias Vecina*; Eduardo Jose Caldeira**; Ricardo Noboro Isayama**; Erivelto Luis Chacon**; Marianna Carla Alves**; Evanisi Teresa Palomari***; Maria Jose Salete Viotto**** & Marcelo Rodrigues da Cunha*,** ALVES DOS SANTOS, D.; IATECOLA, A.; DIAS VECINA, C. A.; CALDEIRA, E. J.; NOBORO ISAYAMA, R.; CHACON, E. L.; ALVES, M. C.; PALOMARI, E. T.; SALETE VIOTTO, M. J. & RODRIGUES DA CUNHA, M. Infraclavicular topography of the brachial plexus fascicles in different upper limb positions. Int. J. Morphol., 34 (3):1063-1068, 2016. SUMMARY: Brachial plexus neuropathies are common complaints among patients seen at orthopedic clinics. The causes range from traumatic to occupational factors and symptoms include paresthesia, paresis, and functional disability of the upper limb. Treatment can be surgical or conservative, but detailed knowledge of the brachial plexus is required in both cases to avoid iatrogenic injuries and to facilitate anesthetic block, preventing possible vascular punctures. Therefore, the objective of this study was to evaluate the topography of the infraclavicular brachial plexus fascicles in different upper limb positions adopted during some clinical procedures. A formalin- preserved, adult, male cadaver was used. The infraclavicular and axillary regions were dissected and the distance of the brachial plexus fascicles from adjacent bone structures was measured. No anatomical variation in the formation of the brachial plexus was observed. The metric relationships between the brachial plexus and adjacent bone prominences differed depending on the degree of shoulder abduction.