The Weakness of Strong Policies and the Strength of Weak Policies: Law, Experimentalist Governance, and Supporting Coalitions in European Union Health Care Policy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Visser Chronicles
1 Animorphs Chronicles 3 Visser K.A. Applegate *Converted to EBook by asmodeus *edited by Dace k 2 Prologue “Honey?” No answer. My husband was watching a game on television. He was preoccupied. “Honey?” I repeated, adding more urgency to my tone of voice. He looked over. Smiled sheepishly. “What’s up?” “Marco’s fever is down. I think he’s basically over this thing. He’s asleep. Anyway, I was thinking of getting some fresh air.” He muted the television. “Good idea. It’s tough when they’re sick, huh? Kids. He’s okay, though, huh?” “It’s just a virus.” “Yeah, well, take some time, you’ve been carrying the load. And if you’re going to the store- “ “Actually, I think I’ll go down to the marina.” He laughed and shook his head. “Ever since you bought that boat… I think Marco has some competition as the favorite child in this household.” He frowned. “You’re not taking it out, are you? Looks kind of gloomy out.” I made a smile. “Just want to make sure it’s well secured, check the ropes and all.” He was back with the game. He winced at some error made by his preferred team. “Uh-huh. Okay.” I stepped back, turned, and walked down the hall. The door to Marco’s room was ajar. I paused to look inside. I almost couldn’t do otherwise because the other voice in my head, the beaten-down, repressed human voice, was alive and screaming and screaming at me, begging me, pleading <No! No! No!> Marco was still asleep. -

The Role of Picture Books in Developing an Empathic Response Towards Cultural Difference
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Queensland University of Technology ePrints Archive THE ROLE OF PICTURE BOOKS IN DEVELOPING AN EMPATHIC RESPONSE TOWARDS CULTURAL DIFFERENCE Kumarasinghe, Dissanayake Mudiyanselage MA (UQ), PGD (Peradeniya), BA (Peradeniya) Submitted in fulfilment of the requirements for the degree of Doctor of Philosophy (IF49) Office of Education Research Faculty of Education Queensland University of Technology 2016 The Role of Picture Books in Developing an Empathic Response towards Cultural Difference ii Keywords Australian children’s literature, picture books, Australian multicultural picture books, multiculturalism, Australian multiculturalism, cultural difference, cognitive narratology, empathy, narrative empathy, empathic unsettlement, semiotics, schema and scripts. The Role of Picture Books in Developing an Empathic Response towards Cultural Difference iii The Role of Picture Books in Developing an Empathic Response towards Cultural Difference iv Abstract This study investigates how empathic narrative techniques are used in a selection of contemporary Australian ‘multicultural’ picture books to position their readers to take up empathic responses towards cultural difference. Drawing examples from 17 migration-themed Australian picture books, it argues that picture books, through fictional manifestation of migrants’ experiences, encourage readers’ perceptive understanding of the plights of migrants and refugees, and thereby have the potential to nurture -
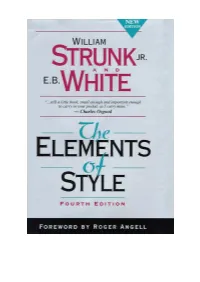
THE ELEMENTS of STYLE' (4Th Edition) First Published in 1935, Copyright © Oliver Strunk Last Revision: © William Strunk Jr
2 OLIVER STRUNK: 'THE ELEMENTS OF STYLE' (4th edition) First published in 1935, Copyright © Oliver Strunk Last Revision: © William Strunk Jr. and Edward A. Tenney, 2000 Earlier editions: © Macmillan Publishing Co., Inc., 1959, 1972 Copyright © 2000, 1979, ALLYN & BACON, 'A Pearson Education Company' Introduction - © E. B. White, 1979 & 'The New Yorker Magazine', 1957 Foreword by Roger Angell, Afterward by Charles Osgood, Glossary prepared by Robert DiYanni ISBN 0-205-30902-X (paperback), ISBN 0-205-31342-6 (casebound). ________ Machine-readable version and checking: O. Dag E-mail: [email protected] URL: http://orwell.ru/library/others/style/ Last modified on April, 2003. 3 The Elements of Style Oliver Strunk Contents FOREWORD ix INTRODUCTION xiii I. ELEMENTARY RULES OF USAGE 1 1. Form the possessive singular of nouns by adding 's. 1 2. In a series of three or more terms with a single conjunction, use a comma after each term except the last. 2 3. Enclose parenthetic expressions between commas. 2 4. Place a comma before a conjunction introducing an independent clause. 5 5. Do not join independent clauses with a comma. 5 6. Do not break sentences in two. 7 7. Use a colon after an independent clause to introduce a list of particulars, an appositive, an amplification, or an illustrative quotation. 7 8. Use a dash to set off an abrupt break or interruption and to announce a long appositive or summary. 9 9. The number of the subject determines the number of the verb. 9 10. Use the proper case of pronoun. 11 11. A participial phrase at the beginning of a sentence must refer to the grammatical subject. -

© Osprey Publishing • ORC WARFARE Chris Pramas
© Osprey Publishing • www.ospreypublishing.com ORC WARFARE Chris Pramas © Osprey Publishing • www.ospreypublishing.com INTRODUCTION To use the word orc 100 years ago was to invite confusion. There were malicious faeries and spirits from folklore and mythology to be sure, but nothing quite like the orc. It began, as many fantasy staples did, with The Lord of the Rings. J. R. R. Tolkien set the template of the orc in modern fantasy. In his tales orcs are twisted, evil creatures – the foot soldiers of dark lords like Morgoth and Sauron. Their numbers seem endless, but they can be cowardly when confronted or when their leaders are slain. From Tolkien, orcs spread to the role playing game Dungeons & Dragons, where they became pig-faced beast-men. And from thousands of readers and thousands of gamers, orcs spread to countless fantasy worlds. Now orcs are a go-to ingredient of modern fantasy, along with elves and dwarves. They are in books, games, and hugely popular movies. If you say the word orc today, many people will nod along. Yes, orcs, of course. They have become part of our culture. It is therefore not as strange as it might appear that Osprey, a publisher known for its extensive line of historical and military books, would commission a book about orcs. Why not take orcs, the scourge of a thousand worlds, and give them a military and cultural analysis? Why not take a fantasy race and give it the Osprey treatment? Orc Warfare, the book you hold in your hands, attempts to do just that. -

Uganda Wildlife Assessment PDFX
UGANDA WILDLIFE TRAFFICKING REPORT ASSESSMENT APRIL 2018 Alessandra Rossi TRAFFIC REPORT TRAFFIC is a leading non-governmental organisation working globally on trade in wild animals and plants in the context of both biodiversity conservation and sustainable development. Reproduction of material appearing in this report requires written permission from the publisher. The designations of geographical entities in this publication, and the presentation of the material, do not imply the expression of any opinion whatsoever on the part of TRAFFIC or its supporting organisations con cern ing the legal status of any country, territory, or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Published by: TRAFFIC International David Attenborough Building, Pembroke Street, Cambridge CB2 3QZ, UK © TRAFFIC 2018. Copyright of material published in this report is vested in TRAFFIC. ISBN no: UK Registered Charity No. 1076722 Suggested citation: Rossi, A. (2018). Uganda Wildlife Trafficking Assessment. TRAFFIC International, Cambridge, United Kingdom. Front cover photographs and credit: Mountain gorilla Gorilla beringei beringei © Richard Barrett / WWF-UK Tree pangolin Manis tricuspis © John E. Newby / WWF Lion Panthera leo © Shutterstock / Mogens Trolle / WWF-Sweden Leopard Panthera pardus © WWF-US / Jeff Muller Grey Crowned-Crane Balearica regulorum © Martin Harvey / WWF Johnston's three-horned chameleon Trioceros johnstoni © Jgdb500 / Wikipedia Shoebill Balaeniceps rex © Christiaan van der Hoeven / WWF-Netherlands African Elephant Loxodonta africana © WWF / Carlos Drews Head of a hippopotamus Hippopotamus amphibius © Howard Buffett / WWF-US Design by: Hallie Sacks This report was made possible with support from the American people delivered through the U.S. Agency for International Development (USAID). The contents are the responsibility of the authors and do not necessarily reflect the opinion of USAID or the U.S. -

Experimental and Quasi-Experimental Designs for Research
CHAPTER 5 Experimental and Quasi-Experimental Designs for Research l DONALD T. CAMPBELL Northwestern University JULIAN C. STANLEY Johns Hopkins University In this chapter we shall examine the validity (1960), Ferguson (1959), Johnson (1949), of 16 experimental designs against 12 com Johnson and Jackson (1959), Lindquist mon threats to valid inference. By experi (1953), McNemar (1962), and Winer ment we refer to that portion of research in (1962). (Also see Stanley, 19S7b.) which variables are manipulated and their effects upon other variables observed. It is well to distinguish the particular role of this PROBLEM AND chapter. It is not a chapter on experimental BACKGROUND design in the Fisher (1925, 1935) tradition, in which an experimenter having complete McCall as a Model mastery can schedule treatments and meas~ In 1923, W. A. McCall published a book urements for optimal statistical efficiency, entitled How to Experiment in Education. with complexity of design emerging only The present chapter aspires to achieve an up from that goal of efficiency. Insofar as the to-date representation of the interests and designs discussed in the present chapter be considerations of that book, and for this rea come complex, it is because of the intransi son will begin with an appreciation of it. gency of the environment: because, that is, In his preface McCall said: "There afe ex of the experimenter's lack of complete con cellent books and courses of instruction deal trol. While contact is made with the Fisher ing with the statistical manipulation of ex; tradition at several points, the exposition of perimental data, but there is little help to be that tradition is appropriately left to full found on the methods of securing adequate length presentations, such as the books by and proper data to which to apply statis Brownlee (1960), Cox (1958), Edwards tical procedure." This sentence remains true enough today to serve as the leitmotif of 1 The preparation of this chapter bas been supported this presentation also. -

The Roots to Peace in the Democratic Republic of Congo: Conservation As a Platform for Green Development
The roots to peace in the Democratic Republic of Congo: conservation as a platform for green development RICHARD MILBURN The Democratic Republic of Congo (DRC) is endowed with a wealth of natural resources, and the presence of high-value minerals such as coltan and diamonds is well known. The country is also endowed with a wealth of biodiversity, although the value of this is often overlooked. The DRC ranks fifth in terms of the most biodiverse countries in the world; it is home to a plethora of endemic species of both flora and fauna and contains the second largest rainforest in the world, smaller only than the Amazon.1 This range of flora and fauna has suffered enormously from the effects of armed conflict in the country over the past two decades, and many wildlife populations have been decimated. In spite of destruction through conflict, key populations and ecosystems still remain and they are crucial for the country’s development and the world’s fight against climate change. The DRC’s conflict is complex and poorly understood. It has exacted an enor- mous toll of human suffering in the country, where over five million people have died.2 It is therefore of the utmost importance to identify contributory factors to the conflict and methods to help end it; and to find ways to promote development to lift the people out of poverty and enable them to move to sustainable economic growth. This article examines the role biodiversity can play in this process. The combination of a wealth of biodiversity, the poverty of the majority of the population,3 and almost two decades of inter- and intrastate armed conflict (which continues to this day) make the country an excellent case-study through which to examine the interaction of biodiversity, armed conflict and development. -

Critical Thinking
Critical Thinking Mark Storey Bellevue College Copyright (c) 2013 Mark Storey Permission is granted to copy, distribute and/or modify this document under the terms of the GNU Free Documentation License, Version 1.3 or any later version published by the Free Software Foundation; with no Invariant Sections, no Front-Cover Texts, and no Back-Cover Texts. A copy of the license is found at http://www.gnu.org/copyleft/fdl.txt. 1 Contents Part 1 Chapter 1: Thinking Critically about the Logic of Arguments .. 3 Chapter 2: Deduction and Induction ………… ………………. 10 Chapter 3: Evaluating Deductive Arguments ……………...…. 16 Chapter 4: Evaluating Inductive Arguments …………..……… 24 Chapter 5: Deductive Soundness and Inductive Cogency ….…. 29 Chapter 6: The Counterexample Method ……………………... 33 Part 2 Chapter 7: Fallacies ………………….………….……………. 43 Chapter 8: Arguments from Analogy ………………………… 75 Part 3 Chapter 9: Categorical Patterns….…….………….…………… 86 Chapter 10: Propositional Patterns……..….…………...……… 116 Part 4 Chapter 11: Causal Arguments....……..………….………....…. 143 Chapter 12: Hypotheses.….………………………………….… 159 Chapter 13: Definitions and Analyses...…………………...…... 179 Chapter 14: Probability………………………………….………199 2 Chapter 1: Thinking Critically about the Logic of Arguments Logic and critical thinking together make up the systematic study of reasoning, and reasoning is what we do when we draw a conclusion on the basis of other claims. In other words, reasoning is used when you infer one claim on the basis of another. For example, if you see a great deal of snow falling from the sky outside your bedroom window one morning, you can reasonably conclude that it’s probably cold outside. Or, if you see a man smiling broadly, you can reasonably conclude that he is at least somewhat happy. -

Private Armies in the Early Korean Military Tradition (850-1598)
Penn History Review Volume 19 Issue 1 Fall 2011 Article 4 September 2012 Private Armies in the Early Korean Military Tradition (850-1598) Samuel Bieler University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/phr Recommended Citation Bieler, Samuel (2012) "Private Armies in the Early Korean Military Tradition (850-1598)," Penn History Review: Vol. 19 : Iss. 1 , Article 4. Available at: https://repository.upenn.edu/phr/vol19/iss1/4 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/phr/vol19/iss1/4 For more information, please contact [email protected]. Early Korean Armies Private Armies in the Early Korean Military Tradition (850-1598) Samuel Bieler From 850 to 1598, private armies were a critical feature of Korean history. They buttressed the military government of the Ch’oe in the late 1100s, usurped the Koryo Dynasty to make way for the rise of the Chosen in 1392, and fought the Japanese invasion forces of Toyotomi Hideyoshi during the Imjin War (1592-1598). They came from every facet of Korean society: peasant resistance forces, retainers of noble houses, and even contingents of Buddhist monks. Yet there has not been a great deal of analysis of the conditions that gave rise to private armies, nor whether in each conflict there were unique or similar conditions that lent themselves to the formation of private military forces in Korea during the different periods. Because these armies were not a constant feature of Korean history, the question of why certain eras witnessed the rise of private armies, while others did not, requires a closer examination. -

Book Chapter Reference
Book Chapter Trickster Narratives of the New World: Erdrich, Dorris, Columbus MADSEN, Deborah Lea Abstract The trickster figure, the shape-shifting, healing culture-hero Nanabozho, is central to Anishinaabe culture and the writings of contemporary writers of Anishinaabe descent, such as Louise Erdrich and Gerald Vizenor. In the introduction to Narrative Chance (1989), for example, Vizenor writes: "The trickster is a communal sign in a comic narrative; the comic holotrope (the whole figuration) is a consonance in tribal discourse. Silence and separation, not monologues in social science methodologies, are the antitheses of trickster discourse" (emphasis in original, 1989, 9). Others, like the Anishinaabe scholar Lawrence W. Gross, place the trickster directly at the heart of efforts to ensure tribal cultural survival. In this essay, I want to analyze the role of trickster discourses in response to the impact of colonization in Louise Erdrich's fiction, with a particular focus on the novel she co-authored with Michael Dorris, The Crown of Columbus (1991) and their subsequent writing for young adults, specifically the children's narratives dealing with the period of first contact with Europeans, such as Dorris's Morning Girl [...] Reference MADSEN, Deborah Lea. Trickster Narratives of the New World: Erdrich, Dorris, Columbus. In: Sahawney, B. Studies in the Literary Achievement of Louise Erdrich, Native American Writer. Lewiston : Edwin Mellen Press, 2009. Available at: http://archive-ouverte.unige.ch/unige:87784 Disclaimer: layout of this document may differ from the published version. 1 / 1 1 Published in Studies in the Literary Achievement of Louise Erdrich, Native American Writer: Fifteen Critical Essays, ed. -

The Novel-Machine Kendrick, Walter
The Novel-Machine Kendrick, Walter Published by Johns Hopkins University Press Kendrick, Walter. The Novel-Machine: The Theory and Fiction of Anthony Trollope. Johns Hopkins University Press, 1980. Project MUSE. doi:10.1353/book.68476. https://muse.jhu.edu/. For additional information about this book https://muse.jhu.edu/book/68476 [ Access provided at 29 Sep 2021 12:38 GMT with no institutional affiliation ] This work is licensed under a Creative Commons Attribution 4.0 International License. HOPKINS OPEN PUBLISHING ENCORE EDITIONS Walter M. Kendrick The Novel-Machine The Theory and Fiction of Anthony Trollope Open access edition supported by the National Endowment for the Humanities / Andrew W. Mellon Foundation Humanities Open Book Program. © 2019 Johns Hopkins University Press Published 2019 Johns Hopkins University Press 2715 North Charles Street Baltimore, Maryland 21218-4363 www.press.jhu.edu The text of this book is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License: https://creativecommons.org/licenses/by-nc-nd/4.0/. CC BY-NC-ND ISBN-13: 978-1-4214-3402-5 (open access) ISBN-10: 1-4214-3402-4 (open access) ISBN-13: 978-1-4214-3400-1 (pbk. : alk. paper) ISBN-10: 1-4214-3400-8 (pbk. : alk. paper) ISBN-13: 978-1-4214-3401-8 (electronic) ISBN-10: 1-4214-3401-6 (electronic) This page supersedes the copyright page included in the original publication of this work. THE NOVEL-MACHINE ��� The Novel-Machine The Theory and Fiction of Anthony Trollope Walter M. Kendrick The Johns Hopkins University Press Baltimore and London This book was brought to publication with the generous assistance of the Andrew W. -

Zola's Theory and Practice in the Genealogical Novel
Zola's theory and practice in the genealogical novel Item Type text; Thesis-Reproduction (electronic) Authors Wright, Grace, 1901- Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 09/10/2021 21:03:44 Link to Item http://hdl.handle.net/10150/553467 ZOLA'S THEORY AND PRACTICE IN THE GENEALOGICAL NOVEL , - -^ " " . ••• > •• - •; *.• .* '■ -«■ -• -r *. ■'» r * * < > Grace Wright fv - ..- - .• A TTieala submitted to the faculty of the .Bep&rtii^nt of English - / . v ' ■■■■:' ia partial fulfillment of -: ’ ' - - - - - : ~ \ : , the requirements for the degree of ;i m a t e r of Arts in the Graduate College University of Arizona 1 9 3 9 Approved! A 0 , M 3 1 Auvleer $ b$ tatmtOAas o t a raoaBY ?’ajos «R m K JAOItX5U.X31QED ***,0 A * .. ajiA lc •333X/0O odd r*i s a o 1o vdls ievittU Q A 0 £ W 1 ' / > ;■ r tuyj; 2- TABLE OF CONTENTS Chapter Page I. INTRODUCTION 1 II. PREPARING FOR THE EXPERIMENT 12 1. The Method 2. The Defining of the Purpose 3. The Selection of the Material III. FORMATION OF THE TWO BRANCHES 21 1. Inherited Characteristics 2. Differences IV. THE GROUP EXPERIMENT 33 1. Subjecti The Family 2. Environmental Changes The Coup d*Etat 3. Reactions V. INDIVIDUAL EXPERIMENTS WITH THE THIRD GENERATION 1. Eugbne 2. Aristide and Sidonie 3. Marthe and Francois 4.