Titanium Alloys for Dental Implants: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Presence of ROS in Inflammatory Environment of Peri-Implantitis Tissue
Journal of Clinical Medicine Article Presence of ROS in Inflammatory Environment of Peri-Implantitis Tissue: In Vitro and In Vivo Human Evidence 1, 2, 2, 3 4 Eitan Mijiritsky y, Letizia Ferroni y, Chiara Gardin y, Oren Peleg , Alper Gultekin , Alper Saglanmak 4, Lucia Gemma Delogu 5, Dinko Mitrecic 6, Adriano Piattelli 7, 8, 2,9, , Marco Tatullo z and Barbara Zavan * z 1 Head and Neck Maxillofacial Surgery, Department of Otoryngology, Tel-Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel-Aviv University, Weizmann street 6, 6423906 Tel-Aviv, Israel; [email protected] 2 Maria Cecilia Hospital, GVM Care & Research, Cotignola, 48033 Ravenna, Italy; [email protected] (L.F.); [email protected] (C.G.) 3 Department of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel-Aviv Sourasky Medical Center, Sackler School of Medicine, Tel Aviv University, 701990 Tel-Aviv, Israel; [email protected] 4 Istanbul University, Faculty of Dentistry, Department of Oral Implantology, 34093 Istanbul, Turkey; [email protected] (A.G.); [email protected] (A.S.) 5 University of Padova, DpT Biomedical Sciences, 35133 Padova, Italy; [email protected] 6 School of Medicine, Croatian Institute for Brain Research, University of Zagreb, Šalata 12, 10 000 Zagreb, Croatia; [email protected] 7 Department of Medical, Oral, and Biotechnological Sciences, University of Chieti-Pescara, via dei Vestini 31, 66100 Chieti, Italy; [email protected] 8 Marrelli Health-Tecnologica Research Institute, Biomedical Section, Street E. Fermi, 88900 Crotone, Italy; [email protected] 9 Department of Medical Sciences, University of Ferrara, via Fossato di Mortara 70, 44123 Ferara, Italy * Correspondence: [email protected] Co-first author. -
Overview of Biomaterials and Their Use in Medical Devices
© 2003 ASM International. All Rights Reserved. www.asminternational.org Handbook of Materials for Medical Devices (#06974G) CHAPTER 1 Overview of Biomaterials and Their Use in Medical Devices A BIOMATERIAL, as defined in this hand- shapes, have relatively low cost, and be readily book, is any synthetic material that is used to available. replace or restore function to a body tissue and Figure 1 lists the various material require- is continuously or intermittently in contact with ments that must be met for successful total joint body fluids (Ref 1). This definition is somewhat replacement. The ideal material or material restrictive, because it excludes materials used combination should exhibit the following prop- for devices such as surgical or dental instru- erties: ments. Although these instruments are exposed A biocompatible chemical composition to to body fluids, they do not replace or augment • avoid adverse tissue reactions the function of human tissue. It should be noted, Excellent resistance to degradation (e.g., cor- however, that materials for surgical instru- • rosion resistance for metals or resistance to ments, particularly stainless steels, are reviewed biological degradation in polymers) briefly in Chapter 3, “Metallic Materials,” in Acceptable strength to sustain cyclic loading this handbook. Similarly, stainless steels and • endured by the joint shape memory alloys used for dental/endodon- A low modulus to minimize bone resorption tic instruments are discussed in Chapter 10, • High wear resistance to minimize wear- “Biomaterials for Dental Applications.” • debris generation Also excluded from the aforementioned defi- nition are materials that are used for external prostheses, such as artificial limbs or devices Uses for Biomaterials (Ref 3) such as hearing aids. -

Repoussé Work for Amateurs
rf Bi oN? ^ ^ iTION av op OCT i 3 f943 2 MAY 8 1933 DEC 3 1938 MAY 6 id i 28 dec j o m? Digitized by the Internet Archive in 2011 with funding from Boston Public Library http://www.archive.org/details/repoussworkforamOOhasl GROUP OF LEAVES. Repousse Work for Amateurs. : REPOUSSE WORK FOR AMATEURS: BEING THE ART OF ORNAMENTING THIN METAL WITH RAISED FIGURES. tfjLd*- 6 By L. L. HASLOPE. ILLUSTRATED. LONDON L. UPCOTT GILL, 170, STRAND, W.C, 1887. PRINTED BY A. BRADLEY, 170, STRAND, LONDON. 3W PREFACE. " JjJjtfN these days, when of making books there is no end," ^*^ and every description of work, whether professional or amateur, has a literature of its own, it is strange that scarcely anything should have been written on the fascinating arts of Chasing and Repousse Work. It is true that a few articles have appeared in various periodicals on the subject, but with scarcely an exception they treated only of Working on Wood, and the directions given were generally crude and imperfect. This is the more surprising when we consider how fashionable Repousse Work has become of late years, both here and in America; indeed, in the latter country, "Do you pound brass ? " is said to be a very common question. I have written the following pages in the hope that they might, in some measure, supply a want, and prove of service to my brother amateurs. It has been hinted to me that some of my chapters are rather "advanced;" in other words, that I have gone farther than amateurs are likely to follow me. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

The Use of Titanium in Dentistry
Cells and Materials Volume 5 Number 2 Article 9 1995 The Use of Titanium in Dentistry Toru Okabe Baylor College of Dentistry, Dallas Hakon Hero Scandinavian Institute of Dental Materials, Haslum Follow this and additional works at: https://digitalcommons.usu.edu/cellsandmaterials Part of the Dentistry Commons Recommended Citation Okabe, Toru and Hero, Hakon (1995) "The Use of Titanium in Dentistry," Cells and Materials: Vol. 5 : No. 2 , Article 9. Available at: https://digitalcommons.usu.edu/cellsandmaterials/vol5/iss2/9 This Article is brought to you for free and open access by the Western Dairy Center at DigitalCommons@USU. It has been accepted for inclusion in Cells and Materials by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. Cells and Materials, Vol. 5, No. 2, 1995 (Pages 211-230) 1051-6794/95$5 0 00 + 0 25 Scanning Microscopy International, Chicago (AMF O'Hare), IL 60666 USA THE USE OF TITANIUM IN DENTISTRY Toru Okabe• and HAkon Hem1 Baylor College of Dentistry, Dallas, TX, USA 1Scandinavian Institute of Dental Materials (NIOM), Haslum, Norway (Received for publication August 8, 1994 and in revised form September 6, 1995) Abstract Introduction The aerospace, energy, and chemical industries have Compared to the metals and alloys commonly used benefitted from favorable applications of titanium and for many years for various industrial applications, tita titanium alloys since the 1950's. Only about 15 years nium is a rather "new" metal. Before the success of the ago, researchers began investigating titanium as a mate Kroll process in 1938, no commercially feasible way to rial with the potential for various uses in the dental field, produce pure titanium had been found. -
Cobalt Chrome Alloy Strength Without Size… Achieving Rigid Fixation Without the Bulk
Cobalt Chrome Alloy Strength Without Size… Achieving Rigid Fixation Without the Bulk • Cobalt Chrome Alloy Rod, 5.5mm Diameter • Polaris™ Deformity System • Trivium™ Derotation System Customizable Spinal Deformity Correction The Polaris™ Deformity System is available in Titanium and Stainless Steel in both 5.5mm and 6.35mm diameter rods. We now offer three tensile strengths of Cobalt Chrome Alloy in 5.5mm diameter rods. Our rod options offer you the ability to customize deformity correction based on curve type, curve stiffness and rigidity, and desired curve correction. Polaris™ Cobalt Chrome Alloy and Stainless Steel rods are Titanium rods are offered in three grades. offered in three tensile strengths. Cobalt Chrome Alloy Stainless Steel Titanium • Available in 5.5mm • Available in 5.5mm • Available in 5.5mm and 6.35mm and 6.35mm • Imaging advantages due • Offered in Titanium alloy and Commercially Pure Titanium to its use with titanium • Retains the initial bend screws and hooks and provides rigid fixation • Less exertion required for bending • Maintaining high strength • Imaging advantages without compromising profile Low Standard CP Ti 5.5mm and Ti Alloy 5.5mm 6.35mm High Ti Alloy 6.35mm Material Comparison Characteristics Cobalt Chrome Alloy Stainless Steel Titanium Stiffness High High Low Strength High High Medium Corrosion Resistance Medium Low High Notch Sensitivity Medium Low High Imaging Compatibility Medium Low High Cobalt Chrome Alloy for Spinal Deformity Correction The Polaris™ Deformity System offers a 5.5mm diameter Cobalt Chrome Alloy (CoCrMo) rod, which is offered in three tensile strengths for use with Polaris™ Titanium Implants. CoCrMo has a history of use in various orthopedic implants, and provides rigid fixation while maintaining imaging capability. -

Metals and Metal Products Tariff Schedules of the United States
251 SCHEDULE 6. - METALS AND METAL PRODUCTS TARIFF SCHEDULES OF THE UNITED STATES SCHEDULE 6. - METALS AND METAL PRODUCTS 252 Part 1 - Metal-Bearing Ores and Other Metal-Bearing Schedule 6 headnotes: Materials 1, This schedule does not cover — Part 2 Metals, Their Alloys, and Their Basic Shapes and Forms (II chemical elements (except thorium and uranium) and isotopes which are usefully radioactive (see A. Precious Metals part I3B of schedule 4); B. Iron or Steel (II) the alkali metals. I.e., cesium, lithium, potas C. Copper sium, rubidium, and sodium (see part 2A of sched D. Aluminum ule 4); or E. Nickel (lii) certain articles and parts thereof, of metal, F. Tin provided for in schedule 7 and elsewhere. G. Lead 2. For the purposes of the tariff schedules, unless the H. Zinc context requires otherwise — J. Beryllium, Columbium, Germanium, Hafnium, (a) the term "precious metal" embraces gold, silver, Indium, Magnesium, Molybdenum, Rhenium, platinum and other metals of the platinum group (iridium, Tantalum, Titanium, Tungsten, Uranium, osmium, palladium, rhodium, and ruthenium), and precious- and Zirconium metaI a Iloys; K, Other Base Metals (b) the term "base metal" embraces aluminum, antimony, arsenic, barium, beryllium, bismuth, boron, cadmium, calcium, chromium, cobalt, columbium, copper, gallium, germanium, Part 3 Metal Products hafnium, indium, iron, lead, magnesium, manganese, mercury, A. Metallic Containers molybdenum, nickel, rhenium, the rare-earth metals (Including B. Wire Cordage; Wire Screen, Netting and scandium and yttrium), selenium, silicon, strontium, tantalum, Fencing; Bale Ties tellurium, thallium, thorium, tin, titanium, tungsten, urani C. Metal Leaf and FoU; Metallics um, vanadium, zinc, and zirconium, and base-metal alloys; D, Nails, Screws, Bolts, and Other Fasteners; (c) the term "meta I" embraces precious metals, base Locks, Builders' Hardware; Furniture, metals, and their alloys; and Luggage, and Saddlery Hardware (d) in determining which of two or more equally specific provisions for articles "of iron or steel", "of copper", E. -
MEMS Technology for Physiologically Integrated Devices
A BioMEMS Review: MEMS Technology for Physiologically Integrated Devices AMY C. RICHARDS GRAYSON, REBECCA S. SHAWGO, AUDREY M. JOHNSON, NOLAN T. FLYNN, YAWEN LI, MICHAEL J. CIMA, AND ROBERT LANGER Invited Paper MEMS devices are manufactured using similar microfabrica- I. INTRODUCTION tion techniques as those used to create integrated circuits. They often, however, have moving components that allow physical Microelectromechanical systems (MEMS) devices are or analytical functions to be performed by the device. Although manufactured using similar microfabrication techniques as MEMS can be aseptically fabricated and hermetically sealed, those used to create integrated circuits. They often have biocompatibility of the component materials is a key issue for moving components that allow a physical or analytical MEMS used in vivo. Interest in MEMS for biological applications function to be performed by the device in addition to (BioMEMS) is growing rapidly, with opportunities in areas such as biosensors, pacemakers, immunoisolation capsules, and drug their electrical functions. Microfabrication of silicon-based delivery. The key to many of these applications lies in the lever- structures is usually achieved by repeating sequences of aging of features unique to MEMS (for example, analyte sensitivity, photolithography, etching, and deposition steps in order to electrical responsiveness, temporal control, and feature sizes produce the desired configuration of features, such as traces similar to cells and organelles) for maximum impact. In this paper, (thin metal wires), vias (interlayer connections), reservoirs, we focus on how the biological integration of MEMS and other valves, or membranes, in a layer-by-layer fashion. The implantable devices can be improved through the application of microfabrication technology and concepts. -

Antibacterial Property and Biocompatibility of Silver, Copper, and Zinc in Titanium Dioxide Layers Incorporated by One-Step Micro-Arc Oxidation: a Review
antibiotics Review Antibacterial Property and Biocompatibility of Silver, Copper, and Zinc in Titanium Dioxide Layers Incorporated by One-Step Micro-Arc Oxidation: A Review Masaya Shimabukuro Department of Biomaterials, Faculty of Dental Science, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan; [email protected]; Tel.: +81-92-642-6346 Received: 3 October 2020; Accepted: 19 October 2020; Published: 20 October 2020 Abstract: Titanium (Ti) and its alloys are commonly used in medical devices. However, biomaterial-associated infections such as peri-implantitis and prosthetic joint infections are devastating and threatening complications for patients, dentists, and orthopedists and are easily developed on titanium surfaces. Therefore, this review focuses on the formation of biofilms on implant surfaces, which is the main cause of infections, and one-step micro-arc oxidation (MAO) as a coating technology that can be expected to prevent infections due to the implant. Many researchers have provided sufficient data to prove the efficacy of MAO for preventing the initial stages of biofilm formation on implant surfaces. Silver (Ag), copper (Cu), and zinc (Zn) are well used and are incorporated into the Ti surface by MAO. In this review, the antibacterial properties, cytotoxicity, and durability of these elements on the Ti surface incorporated by one-step MAO will be summarized. This review is aimed at enhancing the importance of the quantitative control of Ag, Cu, and Zn for their use in implant surfaces and the significance of the biodegradation behavior of these elements for the development of antibacterial properties. Keywords: titanium; biofilm; infection; micro-arc oxidation; silver; copper; zinc; antibacterial properties; coating; implant 1. -
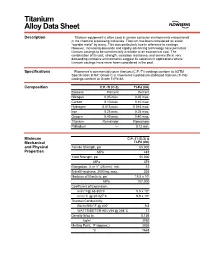
Titanium Alloy Data Sheet
M Titanium Alloy Data Sheet Description Titanium equipment is often used in severe corrosive environments encountered in the chemical processing industries. Titanium has been considered an exotic “wonder metal” by many. This was particularly true in reference to castings. However, increasing demands and rapidly advancing technology have permitted titanium castings to be commercially available at an economical cost. The combination of its cost, strength, corrosion resistance, and service life in very demanding corrosive environments suggest its selection in applications where titanium castings have never been considered in the past. Specifications Flowserve’s commercially pure titanium (C.P.-Ti) castings conform to ASTM Specification B367, Grade C-3. Flowserve’s palladium stabilized titanium (Ti-Pd) castings conform to Grade Ti-Pd 8A. Composition C.P.-Ti (C-3) Ti-Pd (8A) Element Percent Percent Nitrogen 0.05 max. 0.05 max. Carbon 0.10 max. 0.10 max. Hydrogen 0.015 max. 0.015 max. Iron 0.25 max. 0.25 max. Oxygen 0.40 max. 0.40 max. Titanium Remainder Remainder Palladium –– 0.12 min. Minimum C.P.-Ti (C-3) & Mechanical Ti-Pd (8A) and Physical Tensile Strength, psi 65,000 Properties MPa 448 Yield Strength, psi 55,000 MPa 379 Elongation, % in 1" (25 mm), min. 12 Brinell Hardness, 3000 kg, max. 235 Modulus of Elasticity, psi 15.5 x 106 MPa 107,000 Coefficient of Expansion, in/in/°F@ 68-800°F 5.5 x 10-6 m/m/°C @ 20-427°C 9.9 x 10-6 Thermal Conductivity, Btu/hr/ft/ft2/°F @ 400° 9.8 WATTS/METER-KELVIN @ 204°C 17 Density lb/cu in 0.136 kg/m3 3760 Melting Point, °F (approx.) 3035 °C 1668 Titanium Alloy Data Sheet (continued) Corrosion The outstanding mechanical and physical properties of titanium, combined with its Resistance unexpected corrosion resistance in many environments, makes it an excellent choice for particularly aggressive environments like wet chlorine, chlorine dioxide, sodium and calcium hypochlorite, chlorinated brines, chloride salt solutions, nitric acid, chromic acid, and hydrobromic acid. -

Biocompatibility of Polyimides: a Mini-Review
materials Review Biocompatibility of Polyimides: A Mini-Review Catalin P. Constantin 1 , Magdalena Aflori 1 , Radu F. Damian 2 and Radu D. Rusu 1,* 1 “Petru Poni” Institute of Macromolecular Chemistry, Romanian Academy, Aleea Grigore Ghica Voda 41A, Iasi-700487, Romania; [email protected] (C.P.C.); mafl[email protected] (M.A.) 2 SC Intelectro Iasi SRL, Str. Iancu Bacalu, nr.3, Iasi-700029, Romania; [email protected] * Correspondence: [email protected]; Tel.: +40-232-217454 Received: 14 August 2019; Accepted: 25 September 2019; Published: 27 September 2019 Abstract: Polyimides (PIs) represent a benchmark for high-performance polymers on the basis of a remarkable collection of valuable traits and accessible production pathways and therefore have incited serious attention from the ever-demanding medical field. Their characteristics make them suitable for service in hostile environments and purification or sterilization by robust methods, as requested by most biomedical applications. Even if PIs are generally regarded as “biocompatible”, proper analysis and understanding of their biocompatibility and safe use in biological systems deeply needed. This mini-review is designed to encompass some of the most robust available research on the biocompatibility of various commercial or noncommercial PIs and to comprehend their potential in the biomedical area. Therefore, it considers (i) the newest concepts in the field, (ii) the chemical, (iii) physical, or (iv) manufacturing elements of PIs that could affect the subsequent biocompatibility, and, last but not least, (v) in vitro and in vivo biocompatibility assessment and (vi) reachable clinical trials involving defined polyimide structures. The main conclusion is that various PIs have the capacity to accommodate in vivo conditions in which they are able to function for a long time and can be judiciously certified as biocompatible. -

A Mini-Review of Dental Implant Biomaterials
Mini Review Modifying an Implant: A Mini-review of Dental Implant Biomaterials Oliver K. Semisch-Dieter1, Andy H. Choi1, Besim Ben-Nissan1 and Martin P. Stewart1,* Abstract 1School of Life Sciences, Faculty of Science, University Dental implants have been used as far back as 2000BC, and since then have developed into highly sophisti- of Technology Sydney, Ultimo, cated solutions for tooth replacement. It is becoming increasingly important for the materials used in dental implants to exhibit and maintain favorable long-term mechanical, biological and more recently, aesthetic NSW, Australia properties. This review aims to assess the biomaterials used in modern dental implants, introducing their properties, and concentrating on modifications to improve these biomaterials. Focus is drawn to the promi- nent biomaterials, titanium (Ti) and zirconia due to their prevalence in implant dentistry. Additionally, novel coatings and materials with potential use as viable improvements or alternatives are reviewed. An effective *Correspondence to: dental biomaterial should osseointegrate, maintain structural integrity, resist corrosion and infection, and not Martin P. Stewart cause systemic toxicity or cytotoxicity. Current materials such as bioactive glass offer protection against bio- E-mail: martin.stewart@uts. film formation, and when combined with a titanium–zirconium (TiZr) alloy, provide a reliable combination edu.au of properties to represent a competitive alternative. Further long-term clinical studies are needed to inform the development of next-generation materials. Received: September 7 2020 Revised: December 7 2020 Keywords Accepted: January 4 2021 Biocompatibility, biomaterials, dental implant, titanium, zirconia. Published Online: March 19 2021 Significance Statement Available at: Biomaterials have become essential for modern implants.