Antibacterial Property and Biocompatibility of Silver, Copper, and Zinc in Titanium Dioxide Layers Incorporated by One-Step Micro-Arc Oxidation: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatise on Combined Metalworking Techniques: Forged Elements and Chased Raised Shapes Bonnie Gallagher
Rochester Institute of Technology RIT Scholar Works Theses Thesis/Dissertation Collections 1972 Treatise on combined metalworking techniques: forged elements and chased raised shapes Bonnie Gallagher Follow this and additional works at: http://scholarworks.rit.edu/theses Recommended Citation Gallagher, Bonnie, "Treatise on combined metalworking techniques: forged elements and chased raised shapes" (1972). Thesis. Rochester Institute of Technology. Accessed from This Thesis is brought to you for free and open access by the Thesis/Dissertation Collections at RIT Scholar Works. It has been accepted for inclusion in Theses by an authorized administrator of RIT Scholar Works. For more information, please contact [email protected]. TREATISE ON COMBINED METALWORKING TECHNIQUES i FORGED ELEMENTS AND CHASED RAISED SHAPES TREATISE ON. COMBINED METALWORKING TECHNIQUES t FORGED ELEMENTS AND CHASED RAISED SHAPES BONNIE JEANNE GALLAGHER CANDIDATE FOR THE MASTER OF FINE ARTS IN THE COLLEGE OF FINE AND APPLIED ARTS OF THE ROCHESTER INSTITUTE OF TECHNOLOGY AUGUST ( 1972 ADVISOR: HANS CHRISTENSEN t " ^ <bV DEDICATION FORM MUST GIVE FORTH THE SPIRIT FORM IS THE MANNER IN WHICH THE SPIRIT IS EXPRESSED ELIEL SAARINAN IN MEMORY OF MY FATHER, WHO LONGED FOR HIS CHILDREN TO HAVE THE OPPORTUNITY TO HAVE THE EDUCATION HE NEVER HAD THE FORTUNE TO OBTAIN. vi PREFACE Although the processes of raising, forging, and chasing of metal have been covered in most technical books, to date there is no major source which deals with the functional and aesthetic requirements -

Repoussé Work for Amateurs
rf Bi oN? ^ ^ iTION av op OCT i 3 f943 2 MAY 8 1933 DEC 3 1938 MAY 6 id i 28 dec j o m? Digitized by the Internet Archive in 2011 with funding from Boston Public Library http://www.archive.org/details/repoussworkforamOOhasl GROUP OF LEAVES. Repousse Work for Amateurs. : REPOUSSE WORK FOR AMATEURS: BEING THE ART OF ORNAMENTING THIN METAL WITH RAISED FIGURES. tfjLd*- 6 By L. L. HASLOPE. ILLUSTRATED. LONDON L. UPCOTT GILL, 170, STRAND, W.C, 1887. PRINTED BY A. BRADLEY, 170, STRAND, LONDON. 3W PREFACE. " JjJjtfN these days, when of making books there is no end," ^*^ and every description of work, whether professional or amateur, has a literature of its own, it is strange that scarcely anything should have been written on the fascinating arts of Chasing and Repousse Work. It is true that a few articles have appeared in various periodicals on the subject, but with scarcely an exception they treated only of Working on Wood, and the directions given were generally crude and imperfect. This is the more surprising when we consider how fashionable Repousse Work has become of late years, both here and in America; indeed, in the latter country, "Do you pound brass ? " is said to be a very common question. I have written the following pages in the hope that they might, in some measure, supply a want, and prove of service to my brother amateurs. It has been hinted to me that some of my chapters are rather "advanced;" in other words, that I have gone farther than amateurs are likely to follow me. -

Silver Cas # 7440-22-4
SILVER CAS # 7440-22-4 Agency for Toxic Substances and Disease Registry ToxFAQs July 1999 This fact sheet answers the most frequently asked health questions (FAQs) about silver. For more information, call the ATSDR Information Center at 1-888-422-8737. This fact sheet is one in a series of summaries about hazardous substances and their health effects. It’s important you understand this information because this substance may harm you. The effects of exposure to any hazardous substance depend on the dose, the duration, how you are exposed, personal traits and habits, and whether other chemicals are present. HIGHLIGHTS: Silver is an element found naturally in the environment. At very high levels, it may cause argyria, a blue-gray discoloration of the skin and other organs. This chemical has been found in at least 27 of the 1,177 National Priorities List sites identified by the Environmental Protection Agency (EPA). What is silver? o It may be released into water from photographic process ing. (Pronounced s≥l vír) o Rain may wash silver out of soil into the groundwater. Silver is a naturally occurring element. It is found in the o Silver does not appear to concentrate to a significant environment combined with other elements such as sulfide, extent in aquatic animals. chloride, and nitrate. Pure silver is “silver” colored, but silver nitrate and silver chloride are powdery white and silver sul fide and silver oxide are dark-gray to black. Silver is often How might I be exposed to silver? found as a by-product during the retrieval of copper, lead, o Breathing low levels in air. -

The Use of Titanium in Dentistry
Cells and Materials Volume 5 Number 2 Article 9 1995 The Use of Titanium in Dentistry Toru Okabe Baylor College of Dentistry, Dallas Hakon Hero Scandinavian Institute of Dental Materials, Haslum Follow this and additional works at: https://digitalcommons.usu.edu/cellsandmaterials Part of the Dentistry Commons Recommended Citation Okabe, Toru and Hero, Hakon (1995) "The Use of Titanium in Dentistry," Cells and Materials: Vol. 5 : No. 2 , Article 9. Available at: https://digitalcommons.usu.edu/cellsandmaterials/vol5/iss2/9 This Article is brought to you for free and open access by the Western Dairy Center at DigitalCommons@USU. It has been accepted for inclusion in Cells and Materials by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. Cells and Materials, Vol. 5, No. 2, 1995 (Pages 211-230) 1051-6794/95$5 0 00 + 0 25 Scanning Microscopy International, Chicago (AMF O'Hare), IL 60666 USA THE USE OF TITANIUM IN DENTISTRY Toru Okabe• and HAkon Hem1 Baylor College of Dentistry, Dallas, TX, USA 1Scandinavian Institute of Dental Materials (NIOM), Haslum, Norway (Received for publication August 8, 1994 and in revised form September 6, 1995) Abstract Introduction The aerospace, energy, and chemical industries have Compared to the metals and alloys commonly used benefitted from favorable applications of titanium and for many years for various industrial applications, tita titanium alloys since the 1950's. Only about 15 years nium is a rather "new" metal. Before the success of the ago, researchers began investigating titanium as a mate Kroll process in 1938, no commercially feasible way to rial with the potential for various uses in the dental field, produce pure titanium had been found. -

Metals and Metal Products Tariff Schedules of the United States
251 SCHEDULE 6. - METALS AND METAL PRODUCTS TARIFF SCHEDULES OF THE UNITED STATES SCHEDULE 6. - METALS AND METAL PRODUCTS 252 Part 1 - Metal-Bearing Ores and Other Metal-Bearing Schedule 6 headnotes: Materials 1, This schedule does not cover — Part 2 Metals, Their Alloys, and Their Basic Shapes and Forms (II chemical elements (except thorium and uranium) and isotopes which are usefully radioactive (see A. Precious Metals part I3B of schedule 4); B. Iron or Steel (II) the alkali metals. I.e., cesium, lithium, potas C. Copper sium, rubidium, and sodium (see part 2A of sched D. Aluminum ule 4); or E. Nickel (lii) certain articles and parts thereof, of metal, F. Tin provided for in schedule 7 and elsewhere. G. Lead 2. For the purposes of the tariff schedules, unless the H. Zinc context requires otherwise — J. Beryllium, Columbium, Germanium, Hafnium, (a) the term "precious metal" embraces gold, silver, Indium, Magnesium, Molybdenum, Rhenium, platinum and other metals of the platinum group (iridium, Tantalum, Titanium, Tungsten, Uranium, osmium, palladium, rhodium, and ruthenium), and precious- and Zirconium metaI a Iloys; K, Other Base Metals (b) the term "base metal" embraces aluminum, antimony, arsenic, barium, beryllium, bismuth, boron, cadmium, calcium, chromium, cobalt, columbium, copper, gallium, germanium, Part 3 Metal Products hafnium, indium, iron, lead, magnesium, manganese, mercury, A. Metallic Containers molybdenum, nickel, rhenium, the rare-earth metals (Including B. Wire Cordage; Wire Screen, Netting and scandium and yttrium), selenium, silicon, strontium, tantalum, Fencing; Bale Ties tellurium, thallium, thorium, tin, titanium, tungsten, urani C. Metal Leaf and FoU; Metallics um, vanadium, zinc, and zirconium, and base-metal alloys; D, Nails, Screws, Bolts, and Other Fasteners; (c) the term "meta I" embraces precious metals, base Locks, Builders' Hardware; Furniture, metals, and their alloys; and Luggage, and Saddlery Hardware (d) in determining which of two or more equally specific provisions for articles "of iron or steel", "of copper", E. -
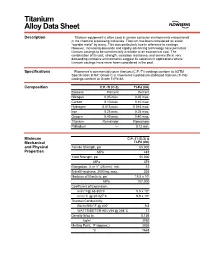
Titanium Alloy Data Sheet
M Titanium Alloy Data Sheet Description Titanium equipment is often used in severe corrosive environments encountered in the chemical processing industries. Titanium has been considered an exotic “wonder metal” by many. This was particularly true in reference to castings. However, increasing demands and rapidly advancing technology have permitted titanium castings to be commercially available at an economical cost. The combination of its cost, strength, corrosion resistance, and service life in very demanding corrosive environments suggest its selection in applications where titanium castings have never been considered in the past. Specifications Flowserve’s commercially pure titanium (C.P.-Ti) castings conform to ASTM Specification B367, Grade C-3. Flowserve’s palladium stabilized titanium (Ti-Pd) castings conform to Grade Ti-Pd 8A. Composition C.P.-Ti (C-3) Ti-Pd (8A) Element Percent Percent Nitrogen 0.05 max. 0.05 max. Carbon 0.10 max. 0.10 max. Hydrogen 0.015 max. 0.015 max. Iron 0.25 max. 0.25 max. Oxygen 0.40 max. 0.40 max. Titanium Remainder Remainder Palladium –– 0.12 min. Minimum C.P.-Ti (C-3) & Mechanical Ti-Pd (8A) and Physical Tensile Strength, psi 65,000 Properties MPa 448 Yield Strength, psi 55,000 MPa 379 Elongation, % in 1" (25 mm), min. 12 Brinell Hardness, 3000 kg, max. 235 Modulus of Elasticity, psi 15.5 x 106 MPa 107,000 Coefficient of Expansion, in/in/°F@ 68-800°F 5.5 x 10-6 m/m/°C @ 20-427°C 9.9 x 10-6 Thermal Conductivity, Btu/hr/ft/ft2/°F @ 400° 9.8 WATTS/METER-KELVIN @ 204°C 17 Density lb/cu in 0.136 kg/m3 3760 Melting Point, °F (approx.) 3035 °C 1668 Titanium Alloy Data Sheet (continued) Corrosion The outstanding mechanical and physical properties of titanium, combined with its Resistance unexpected corrosion resistance in many environments, makes it an excellent choice for particularly aggressive environments like wet chlorine, chlorine dioxide, sodium and calcium hypochlorite, chlorinated brines, chloride salt solutions, nitric acid, chromic acid, and hydrobromic acid. -

Rhodium Products
Rhodium products Rhodium is one of the of six elements in the platinum group, which consists of platinum, palladium, rhodium, osmium, iridium and ruthenium. Often found with deposits of platinum and commonly obtained from the mining and refining of platinum, it is considered to be the rarest and most valuable precious metal, more valuable than gold or silver. Rhodium is a silver-white metallic element with high melting and boiling points. It is highly reflective and resistant to corrosion and oxidation, which is why it is also classified as a noble metal. It was discovered in 1803 by English chemist William Hyde Wollaston shortly after his discovery of palladium. Wollaston extracted rhodium from a piece of platinum ore that he had obtained from South America. Rhodium was named for the rose-red color of its salts, after the Greek word “rhodon” which means rose. Rarely used by itself, rhodium metal is almost always used as an alloy. We offer a broad, diverse catalog of rhodium products which are also available in bulk quantities and pack sizes that can be customized to your requirements. Application highlights: The Alfa Aesar™ portfolio of rhodium products can be used in a wide range of applications, from chemistry research to manufacturing and industry, from emission control and electrical applications to jewelry. Rhodium in chemistry Rhodium is used in research and industrial laboratories primarily as a catalyst. It is preferable to the other platinum group catalysts in the reduction of nitrogen oxides to nitrogen and oxygen. Rhodium is also used to catalyze the reduction of benzene to cyclohexane as well as the addition of hydrosilanes to double bonds, an important step in the manufacture of certain silicone rubbers. -

Invictus Catalog Lowres.Pdf
At Invictus Body Jewelry we believe that professional piercers and body modifi cation artists desire high quality, implant grade jewelry at a reasonable price. To accomplish this, we designed and developed Invictus Body Jewelry to supply implant grade titanium jewelry to professional piercers all over the world. Invictus Body Jewelry is manufactured out of Ti 6Al-4V ELI ASTM F-136 implant grade titanium. All of our jewelry is internally threaded and adheres to industry standard thread patterns. At Invictus Body Jewelry we strive to provide the professional piercer with safe, customizable, and affordable implant grade jewelry. 2 www.invictusbodyjewelry.com Invictus Body Jewelry is manufactured only using implant grade materials - Ti 6Al-4V ELI ASTM-F136. All Invictus Body Jewelry products are internally threaded for professional piercers and their clients. Invictus Body Jewelry uses industry standard thread patterns. We use M1.2 threading on our 14ga and M0.9 threading on our 16ga & 18ga. We believe in providing quality piercing products at reasonable prices to our customers. We fulfi ll orders within 24 to 48 hours from being entered into the system. Invictus Body Jewelry is only available to wholesale customers. Only piercing shops and retailers may purchase our products, not the general public. 203.803.1129 3 HORSESHOES & CURVES TIHI (Internally Threaded Titanium Horseshoes) TICI (Internally Threaded Titanium Curves) CodeSizeDiameter Ends Code Size Diameter Ends TIHI601 16g 1/4” 3mm TIHI411 14g 5/16” 4mm TIHI611 16g 5/16” 3mm TIHI421 -

1 an Investigation of the Mechanical and Physical Properties of Copper
An Investigation of the Mechanical and Physical Properties of Copper-Silver Alloys and the Use of These Alloys in Pre-Columbian America by Shannon L. Taylor Submitted to the Department of Materials Science and Engineering in Partial Fulfillment of the Requirements for the Degree of Bachelor of Science at the Massachusetts Institute of Technology June 2013 © Massachusetts Institute of Technology. All rights reserved. Signature of Author: ____________________________________________________________ Department of Materials Science and Engineering May 3, 2013 Certified by: ___________________________________________________________________ Heather Lechtman Professor of Archaeology and Ancient Technology Thesis Supervisor Accepted by: __________________________________________________________________ Jeffrey Grossman Carl Richard Soderberg Associate Professor of Power Engineering Chair, Undergraduate Committee 1 An Investigation of the Mechanical and Physical Properties of Copper-Silver Alloys and the Use of These Alloys in Pre-Columbian America by Shannon L. Taylor Submitted to the Department of Materials Science and Engineering on May 3, 2013 in Partial Fulfillment of the Requirements for the Degree of Bachelor of Science in Archaeology and Materials ABSTRACT In both the Andean zone of South America and in Mesoamerica, copper-silver alloys were important in the production of thin, silver-colored sheet metal artifacts. This thesis examines the mechanical and physical properties of the copper-silver alloy system that are important to understanding why copper-silver alloys became central to the metallurgies that developed among prehistoric societies of the Andean zone and Western Mexico. These properties include their range of malleability, the microstructures behind their toughness, and the recrystallization and annealing behaviors that led to their development of silver-enriched surfaces. To determine these properties, a series of cold rolling, cold hammering, and annealing experiments were performed on five Cu-Ag alloys and pure copper. -

Effects of Surface Treatments on Stainless Steel 316 Exposed to Potable Water Containing Silver Disinfectant
49th International Conference on Environmental Systems ICES-2019-273 7-11 July 2019, Boston, Massachusetts Effects of Surface Treatments on Stainless Steel 316 Exposed to Potable Water Containing Silver Disinfectant Wenyan Li1, Jerry W. Buhrow2, Angie M. Diaz3, Tesia D. Irwin4, and Luz M. Calle5 NASA, Kennedy Space Center, FL, 32899 Michael R. Callahan 6 NASA Johnson Space Center, Houston, TX, 77058 Silver has been selected as the forward disinfectant candidate for potable water systems in future space exploration missions. To develop a reliable antibacterial system that requires minimal maintenance, it is necessary to address relevant challenges to preclude problems for future missions. One such challenge is silver depletion in potable water systems. When in contact with various materials, silver ions can be easily reduced to silver metal or form insoluble compounds. The same chemical properties that make ionic silver a powerful antimicrobial agent also result in its quick inactivation or depletion in various environments. Different metal surface treatments, such as thermal oxidation and electropolishing, have been investigated for their effectiveness in reducing silver disinfectant depletion in potable water. However, their effects on the metal surface microstructure and chemical resistance have not often been included in the studies. This paper reports the effects of surface treatments on stainless steel 316 (SS316) exposed to potable water containing silver ion as a disinfectant. Early experimental results showed that thermal oxidation, when compared with electropolishing, resulted in a thicker oxide layer but compromised the corrosion resistance of SS316. Nomenclature AgF = silver fluoride DI = deionized I2 = iodine ISS = International Space Station KSC = Kennedy Space Center NASA = National Aeronautics and Space Administration SEM = scanning electron microscopy SS = stainless steel S/V = surface to volume XPS = X-ray photon spectroscopy I. -

THE USE of MIXED MEDIA in the PRODUCTION of METAL ART by Mensah, Emmanuel (B.A. Industrial Art, Metals)
THE USE OF MIXED MEDIA IN THE PRODUCTION OF METAL ART By Mensah, Emmanuel (B.A. Industrial Art, Metals) A Thesis submitted to the School of Graduate Studies, Kwame Nkrumah University of Science and Technology In partial fulfillment of the requirements for the degree of MASTER OF ARTS (ART EDUCATION) Faculty of Art, College of Art and Social Sciences March 2011 © 2011, Department of General Art Studies DECLARATION I hereby declare that this submission is my own work toward the M.A Art Education degree and that, to the best of my knowledge, it contains no materials previously published by another person or material which has been accepted for the award of any other degree of the university, except where due acknowledgement has been made in the text. ……………………………….. ……………………………….. ………………………….. Student’s name & ID Signature Date Certified by ……………………………….. ……………………………….. ………………………….. Supervisor’s Name Signature Date Certified by ……………………………….. ……………………………….. ………………………….. Head of Department’s Name Signature Date ii ABSTRACT The focus of this study was to explore and incorporate various artistic and non artistic media into the production of metal art. The researcher was particularly interested in integrating more non metallic materials that are not traditional to the production of metal art in the decoration, finishing and the protective coating of metal art works. Basic hand forming techniques including raising, chasing and repoussé, piercing and soldering were employed in the execution of the works. Other techniques such as painting, dyeing and macramé were also used. Non metallic media that were used in the production of the works included leather, nail polish, acrylic paint, epoxy, formica glue, graphite, eye pencil, lagging, foam, wood, shoe polish, shoe lace, eggshell paper, spray paint, cotton cords and correction fluid. -
Understanding the Astrophysical Origin of Silver, Palladium and Other Neutron-Capture Elements
Understanding the astrophysical origin of silver, palladium and other neutron-capture elements Camilla Juul Hansen M¨unchen 2010 Understanding the astrophysical origin of silver, palladium and other neutron-capture elements Camilla Juul Hansen Dissertation an der Fakult¨at f¨ur Physik der Ludwig–Maximilians–Universit¨at M¨unchen vorgelegt von Camilla Juul Hansen aus Lillehammer, Norwegen M¨unchen, den 20/12/2010 Erstgutachter: Achim Weiss Zweitgutachter: Joseph Mohr Tag der m¨undlichen Pr¨ufung: 22 M¨arz 2011 Contents 1 Introduction 1 1.1 Evolutionoftheformationprocesses . ..... 2 1.2 Neutron-capture processes: The historical perspective............ 5 1.3 Features and description of the neutron-capture processes.......... 7 1.4 Whatisknownfromobservations? . .. 9 1.5 Why study palladium and silver? . .. 15 1.6 Abiggerpicture................................. 16 2 Data - Sample and Data Reduction 19 2.1 Compositionofthesample . 19 2.1.1 Samplebiases .............................. 21 2.2 Datareduction ................................. 22 2.2.1 Fromrawtoreducedspectra. 22 2.2.2 IRAF versus UVES pipeline . 25 2.3 Merging ..................................... 26 2.3.1 Radialvelocityshift .......................... 27 3 Stellar Parameters 29 3.1 Methods for determining stellar parameters . ........ 29 3.2 Temperature................................... 30 3.2.1 Comparingtemperaturescales . 32 3.3 Gravity ..................................... 34 3.4 Metallicity.................................... 35 3.5 Microturbulence velocity, ξ ..........................