Combined Versus Sequential Injection of Mepivacaine and Ropivacaine for Supraclavicular Nerve Blocks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mepivacaine Hydrochloride Injection
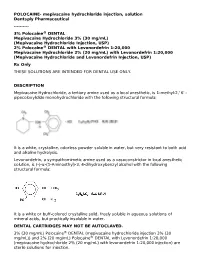
POLOCAINE- mepivacaine hydrochloride injection, solution Dentsply Pharmaceutical ---------- 3% Polocaine® DENTAL Mepivacaine Hydrochloride 3% (30 mg/mL) (Mepivacaine Hydrochloride Injection, USP) 2% Polocaine® DENTAL with Levonordefrin 1:20,000 Mepivacaine Hydrochloride 2% (20 mg/mL) with Levonordefrin 1:20,000 (Mepivacaine Hydrochloride and Levonordefrin Injection, USP) Rx Only THESE SOLUTIONS ARE INTENDED FOR DENTAL USE ONLY. DESCRIPTION Mepivacaine Hydrochloride, a tertiary amine used as a local anesthetic, is 1-methyl-2,' 6' - pipecoloxylidide monohydrochloride with the following structural formula: It is a white, crystalline, odorless powder soluble in water, but very resistant to both acid and alkaline hydrolysis. Levonordefrin, a sympathomimetic amine used as a vasoconstrictor in local anesthetic solution, is (-)-α-(1-Aminoethyl)-3, 4-dihydroxybenzyl alcohol with the following structural formula: It is a white or buff-colored crystalline solid, freely soluble in aqueous solutions of mineral acids, but practically insoluble in water. DENTAL CARTRIDGES MAY NOT BE AUTOCLAVED. 3% (30 mg/mL) Polocaine® DENTAL (mepivacaine hydrochloride injection 3% (30 mg/mL)) and 2% (20 mg/mL) Polocaine® DENTAL with Levonordefrin 1:20,000 (mepivacaine hydrochloride 2% (20 mg/mL) with levonordefrin 1:20,000 injection) are sterile solutions for injection. sterile solutions for injection. COMPOSITION: CARTRIDGE Each mL contains: 2% 3% Mepivacaine Hydrochloride 20 mg 30 mg Levonordefrin 0.05 mg - Sodium Chloride 4 mg 6 mg Potassium metabisulfite 1.2 mg - Edetate disodium 0.25 mg - Sodium Hydroxide q.s. ad pH; Hydrochloric 0.5 mg - Acid Water For Injection, qs. ad. 1 mL 1 mL The pH of the 2% cartridge solution is adjusted between 3.3 and 5.5 with NaOH. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

Local Anesthetic Half Life (In Hours) Lidocaine 1.6 Mepivacaine 1.9 Bupivacaine 353.5 Prilocaine 1.6 Articaine 0.5
Local Anesthetics • The first local anesthetics History were cocaine and procaine (Novacain) developed in ltlate 1800’s • They were called “esters” because of their chemical composition • Esters had a slow onset and short half life so they did not last long History • Derivatives of esters called “amides” were developed in the 1930’s • Amides had a faster onset and a longer half life so they lasted longer • AidAmides quiklickly repldlaced esters • In dentistry today, esters are only found in topical anesthetics Generic Local Anesthetics • There are five amide anesthetics used in dentistry today. Their generic names are; – lidocaine – mepivocaine – bupivacaine – prilocaine – artica ine • Each is known by at least one brand name Brand Names • lidocaine : Xylocaine, Lignospan, Alphacaine, Octocaine • mepivocaine: Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest • prilocaine : Citanest, Citanest Forte • bibupivaca ine: MiMarcaine • articaine: Septocaine, Zorcaine About Local Anesthetic (LA) • Local anesthetic (LA) works by binding with sodium channels in neurons preventing depolarization • LA is inactivated at the injection site when it is absorbed into the blood stream and redistributed throughout the body • If enough LA is absorbed, sodium channels in other parts of the body will be blocked, causing systemic side effects About LA • A clinical effect of LAs is dilation blood vessels, speeding up absorption and distribution • To counteract this dilation so anesthesia is prolonged, , a vasoconstrictor is often added to LAs • However, vasoconstrictors have side effects also Metabolism and Excretion • Most amide LAs are metabolized (inactivated) by the liver and excreted by the kidneys. • Prilocaine is partially metabolized by the lungs • Articaine is partially metabolized by enzymes in the bloo d as well as the liver. -

Meta-Xylene: Identification of a New Antigenic Entity in Hypersensitivity
Clinical Communications Meta-xylene: identification of a new Our patient is a 53-year-old male who presented in 2003 with antigenic entity in hypersensitivity contact dermatitis after the use of lidocaine and disinfection with reactions to local anesthetics chlorhexidine. In 2006, an extensive skin testing by patch, prick, Kuntheavy Ing Lorenzini, PhDa, intradermal sampling, and graded challenge was performed as b c followed. The patch tests were performed with the thin layer Fabienne Gay-Crosier Chabry, MD , Claude Piguet, PhD , rapid use epicutaneous test, using the caine mix (benzocaine, a and Jules Desmeules, MD tetracaine, and cinchocaine), the paraben mix (methyl, ethyl, propyl, butyl, and benzylparaben), and the Balsam of Peru. The Clinical Implications caine and paraben mix were positive, and the patch test was possibly positive for Balsam of Peru. The prick test performed The authors report a patient who presented delayed with preservative-free lidocaine 20 mg/mL (Lidocaïne HCl hypersensitivity reactions to several local anesthetics, all “Bichsel” 2%, Grosse Apotheke Dr. G. Bichsel, Switzerland) was containing a meta-xylene entity, but not to articaine, negative. The intradermal test, performed with lidocaine 20 mg/ which is a thiophene derivative. Meta-xylene could be the mL containing methylparaben (Xylocain 2%, AstraZeneca, immunogenic epitope. Switzerland) with 1/10 and 1/100 dilutions, was negative. The subcutaneous challenge test was performed with 10 mg of preservative-free lidocaine 20 mg/mL (Lidocaïne HCl “Bichsel” TO THE EDITOR: 2%, Grosse Apotheke Dr. G. Bichsel) and lidocaine 20 mg/mL containing methylparaben (Lidocaïne Streuli 2%, Streuli, Hypersensitivity reactions to local anesthetics (LAs) are rare and Switzerland), both of which were positive and had the appear- represent less than 1% of all adverse reactions to LAs. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice. -

Prescribing Information Carbocaine 1%
Prescribing Information Carbocaine 1% 10 mg/mL, Mepivacaine Hydrochloride Injection, USP Carbocaine 2% 20 mg/mL, Mepivacaine Hydrochloride Injection, USP Local Anesthetic Pfizer Canada Inc. DATE OF REVISION: 17300 Trans-Canada Highway August 2, 2017 Kirkland, Québec NTF: February 14, 2018 H9J 2M5 Control Number: (204807) 1 Prescribing Information Carbocaine 1% 10 mg/mL, Mepivacaine Hydrochloride Injection, USP Carbocaine 2% 20 mg/mL, Mepivacaine Hydrochloride Injection, USP Local Anesthetic Pharmacology: Mepivacaine stabilizes the neuronal membrane and prevents the initiation and transmission of nerve impulses, thereby effecting local anesthesia. Its pharmacological properties are somewhat similar to those of lidocaine, which it resembles chemically. Its action is more rapid in onset and somewhat more prolonged than that of lidocaine. It has been employed for all types of infiltration and regional nerve block anesthesia. Onset of anesthesia is rapid, the time of onset for sensory block ranging from about 3 to 20 minutes depending upon such factors as the anesthetic technique, the type of block, the concentration of the solution and the individual patient. The degree of motor blockade produced is dependent on the concentration of the solution. The 1% concentration will block sensory and sympathetic conduction without loss of motor function and will be effective in small superficial nerve blocks. The 2% concentration of mepivacaine will produce complete sensory and motor block of any nerve group. The duration of anesthesia also varies depending upon the technique and type of block, the concentration and the individual. Mepivacaine will normally provide anesthesia which is adequate for 2 to 2½ hours of surgery. It has been reported that vasoconstrictors do not significantly prolong anesthesia with mepivacaine, but epinephrine (1:200 000) may be added to the mepivacaine solution to promote local hemostasis and to delay systemic absorption of the anesthetic. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

A Brief History Behind the Most Used Local Anesthetics
Tetrahedron xxx (xxxx) xxx Contents lists available at ScienceDirect Tetrahedron journal homepage: www.elsevier.com/locate/tet Tetrahedron report XXX A brief history behind the most used local anesthetics * Marco M. Bezerra, Raquel A.C. Leao,~ Leandro S.M. Miranda, Rodrigo O.M.A. de Souza Biocatalysis and Organic Synthesis Group, Chemistry Institute, Federal University of Rio de Janeiro, 21941-909, Brazil article info abstract Article history: The chemistry behind the discovery of local anesthetics is a beautiful way of understanding the devel- Received 13 April 2020 opment and improvement of medicinal/organic chemistry protocols towards the synthesis of biologically Received in revised form active molecules. Here in we present a brief history based on the chemistry development of the most 16 September 2020 used local anesthetics trying to draw a line between the first achievements obtained by the use of Accepted 18 September 2020 cocaine until the synthesis of the mepivacaine analogs nowadays. Available online xxx © 2020 Elsevier Ltd. All rights reserved. Keywords: Anesthetics Medicinal chemistry Organic synthesis Mepivacaíne Contents 1. Introduction . ............................. 00 1.1. Pain and anesthesia . ............................................... 00 1.2. Ancient techniques to achieve anesthesia . ............................... 00 1.3. The objective of this work . .......................................... 00 2. Cocaine .............................................................................................. ............................ -

Lidocaine: a Local Anesthetic, Its Adverse Effects and Management
medicina Review Lidocaine: A Local Anesthetic, Its Adverse Effects and Management Entaz Bahar and Hyonok Yoon * Research Institute of Pharmaceutical Sciences, College of Pharmacy, Gyeongsang National University, Jinju 52828, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-55-772-2422 Abstract: The most widely used medications in dentistry are local anesthetics (LA), especially lidocaine, and the number of recorded adverse allergic responses, particularly of hazardous responses, is quite low. However, allergic reactions can range from moderate to life-threatening, requiring rapid diagnosis and treatment. This article serves as a review to provide information on LA, their adverse reactions, causes, and management. Keywords: local anesthetics; lidocaine; adverse allergic responses 1. Introduction A local anesthetic (LA) is a medicine that is used to numb a small part of the body temporarily before performing a minor surgery like skin biopsy. Before a dental operation, such as tooth extraction, LA may be given to the patient. LA do not cause humans to fall asleep, unlike general anesthesia. They are usually distinguished by their chemical structure, specifically the linkage between the compound’s common components, such as Citation: Bahar, E.; Yoon, H. amide and esters [1]. The vast majority of the regularly used dental LA are amides, for Lidocaine: A Local Anesthetic, Its example, lidocaine, mepivacaine, bupivacaine, etidocaine, prilocaine, and articaine [2]. The Adverse Effects and Management. maximum recommended dose of LA may vary based on the nation, gender, age, weight, Medicina 2021, 57, 782. https:// and medical condition of the patient. The gathering of information from several sources, doi.org/10.3390/medicina57080782 Table1 shows the acceptable maximum doses of LA with or without vasoconstrictor [ 3–5]. -

Prescription Medications, Drugs, Herbs & Chemicals Associated With
Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form, or by any means, without the prior written permission of the American Tinnitus Association. ©2013 American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association This document is to be utilized as a conversation tool with your health care provider and is by no means a “complete” listing. Anyone reading this list of ototoxic drugs is strongly advised NOT to discontinue taking any prescribed medication without first contacting the prescribing physician. Just because a drug is listed does not mean that you will automatically get tinnitus, or exacerbate exisiting tinnitus, if you take it. A few will, but many will not. Whether or not you eperience tinnitus after taking one of the listed drugs or herbals, or after being exposed to one of the listed chemicals, depends on many factors ‐ such as your own body chemistry, your sensitivity to drugs, the dose you take, or the length of time you take the drug. It is important to note that there may be drugs NOT listed here that could still cause tinnitus. Although this list is one of the most complete listings of drugs associated with tinnitus, no list of this kind can ever be totally complete – therefore use it as a guide and resource, but do not take it as the final word. The drug brand name is italicized and is followed by the generic drug name in bold. -

Interventions for Relieving Pain Associated with Panretinal
Eye (2006) 20, 712–719 & 2006 Nature Publishing Group All rights reserved 0950-222X/06 $30.00 www.nature.com/eye 1 2 1 1 CLINICAL STUDY Interventions W-C Wu , K-H Hsu , T-L Chen , Y-S Hwang , K-K Lin1, L-M Li1, C-P Shih2 and C-C Lai1 for relieving pain associated with panretinal photocoagulation: a prospective randomized trial Abstract mefenamic acid, and acetaminophen (either alone or in combination with each other) are Purpose To evaluate the efficacy of pain relief not effective in preventing PRP treatment- by oral diazepam, acetaminophen, mefenamic associated pain. Intramuscular injection of 1Department of acid, intramuscular ketorolac tromethamine, ketorolac tromethamine is also not effective in Ophthalmology, Chang and peribulbar anaesthesia in panretinal reducing PRP-associated pain. Gung Memorial Hospital, photocoagulation (PRP). Eye (2006) 20, 712–719. doi:10.1038/sj.eye.6701989; Taoyuan, Taiwan Methods A total of 220 patients with published online 8 July 2005 proliferative diabetic retinopathy requiring 2The Department of Business Administration, PRP treatment were enrolled in this study. Keywords: peribulbar anesthesia; pain; Chang Gung University, Before laser treatment, the patients were panretinal photocoagulation Taoyuan, Taiwan allocated randomly to one of eight groups: group 1: diazepam (n ¼ 22), group 2: Introduction Correspondence: C-C Lai, acetaminophen (n ¼ 21), group 3: mefenamic Department of acid (n ¼ 21), group 4: diazepam and Panretinal photocoagulation (PRP) is an Ophthalmology, Chang Gung Memorial Hospital, acetaminophen (n ¼ 22), group 5: diazepam effective treatment in reducing severe visual 5 Fu-Hsin St, Kwei-Shan, and mefenamic acid (n ¼ 22), group 6: loss in patients with proliferative diabetic 333, Taoyuan, peribulbar anaesthesia with lidocaine (n ¼ 23), retinopathy (PDR). -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P)