An Update on Local Anesthetics in Dentistry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dental Management of Patients with Inherited Bleeding Disorders: a Multidisciplinary Approach
Dental management of patients with inherited bleeding disorders: a multidisciplinary approach Hassan Abed, BDS, MSc ¢ Abdalrahman Ainousa, BDS, MSc Bleeding disorders can be inherited or acquired and leeding disorders can result from inherited genetic demonstrate different levels of severity. Dentists may be defects or be acquired due to use of anticoagulant med- called on to treat patients who have bleeding disor- ications or medical conditions such as liver dysfunc- ders such as hemophilia A and von Willebrand disease B 1-3 tion, chronic kidney disease, and autoimmune disease. During (vWD). Dental extraction in any patient with clotting blood vessel injury, hemostasis relies on interactions between factor defects can result in a delayed bleeding episode. the vascular vessel wall and activated platelets as well as clot- 4 Local hemostatic measures provide effective results in ting factors. Any marked defect at one of these stages results a majority of cases but are insufficient in patients with in bleeding disorders. Vascular wall defects, platelet defects, severe hemophilia A and vWD. Therefore, consultation or deficiency of clotting factors can affect the severity level of 5 with the patient’s hematologist is required to ensure bleeding episodes. Thus, patients may have mild, moderate, or preoperative prophylactic coverage. Dental care provid- severe episodes of bleeding. ers have to be aware of any signs of bleeding disorders and refer patients for further medical investigations. This Sources of inherited bleeding disorders article aims to provide dental care providers with the Vascular wall defects knowledge to manage patients with inherited bleeding A patient’s bleeding disorder may be unrecognized, and bleeding disorders, especially hemophilia A and vWD. -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -
Mepivacaine Hydrochloride Injection
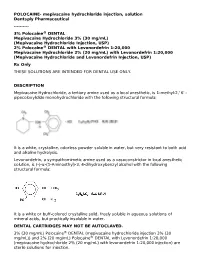
POLOCAINE- mepivacaine hydrochloride injection, solution Dentsply Pharmaceutical ---------- 3% Polocaine® DENTAL Mepivacaine Hydrochloride 3% (30 mg/mL) (Mepivacaine Hydrochloride Injection, USP) 2% Polocaine® DENTAL with Levonordefrin 1:20,000 Mepivacaine Hydrochloride 2% (20 mg/mL) with Levonordefrin 1:20,000 (Mepivacaine Hydrochloride and Levonordefrin Injection, USP) Rx Only THESE SOLUTIONS ARE INTENDED FOR DENTAL USE ONLY. DESCRIPTION Mepivacaine Hydrochloride, a tertiary amine used as a local anesthetic, is 1-methyl-2,' 6' - pipecoloxylidide monohydrochloride with the following structural formula: It is a white, crystalline, odorless powder soluble in water, but very resistant to both acid and alkaline hydrolysis. Levonordefrin, a sympathomimetic amine used as a vasoconstrictor in local anesthetic solution, is (-)-α-(1-Aminoethyl)-3, 4-dihydroxybenzyl alcohol with the following structural formula: It is a white or buff-colored crystalline solid, freely soluble in aqueous solutions of mineral acids, but practically insoluble in water. DENTAL CARTRIDGES MAY NOT BE AUTOCLAVED. 3% (30 mg/mL) Polocaine® DENTAL (mepivacaine hydrochloride injection 3% (30 mg/mL)) and 2% (20 mg/mL) Polocaine® DENTAL with Levonordefrin 1:20,000 (mepivacaine hydrochloride 2% (20 mg/mL) with levonordefrin 1:20,000 injection) are sterile solutions for injection. sterile solutions for injection. COMPOSITION: CARTRIDGE Each mL contains: 2% 3% Mepivacaine Hydrochloride 20 mg 30 mg Levonordefrin 0.05 mg - Sodium Chloride 4 mg 6 mg Potassium metabisulfite 1.2 mg - Edetate disodium 0.25 mg - Sodium Hydroxide q.s. ad pH; Hydrochloric 0.5 mg - Acid Water For Injection, qs. ad. 1 mL 1 mL The pH of the 2% cartridge solution is adjusted between 3.3 and 5.5 with NaOH. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

Hygroscopicity of Pharmaceutical Crystals
HYGROSCOPICITY OF PHARMACEUTICAL CRYSTALS A DISSERTATION SUBMITTED TO THE FACULTY OF GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY DABING CHEN IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY RAJ SURYANARAYANAN (ADVISER) JANUARY, 2009 © Dabing Chen, January / 2009 ACKNOWLEDGEMENTS I am very grateful to my thesis advisor, Prof. Raj Suryanarayanan, for his constant guidance, support, and encouragement throughout my research. Without his help, the completion of this thesis would be impossible. His friendship and advices are precious to my professional and personal growth and will help me overcome many difficulties in my future career. I would like to take the opportunity to thank Prof. David J.W. Grant, who was my advisor during the first three years in graduate school and led me into the research area of physical pharmacy. It was my great honor to have worked for him, and he will always live as a role model in my life. Many thanks to Dr. Zheng Jane Li at Boehringer Ingelheim Pharmaceuticals (BI) for her invaluable advice as an industrial mentor and also for agreeing to serve on my committee. I sincerely appreciate her helpful discussions, revision of the manuscripts, and supervision of my research. I also want to thank her for providing me the internship opportunity at BI. I thank Dr. Timothy S. Wiedmann and Dr. Theodore P. Labuza for serving on my committee and for critically reviewing my thesis. I also want to thank Dr. Timothy S. Wiedmann for allowing me the use of the HPLC instruments in his lab and also for his advice as the Director of Graduate Studies. -

Local Anesthetic Half Life (In Hours) Lidocaine 1.6 Mepivacaine 1.9 Bupivacaine 353.5 Prilocaine 1.6 Articaine 0.5
Local Anesthetics • The first local anesthetics History were cocaine and procaine (Novacain) developed in ltlate 1800’s • They were called “esters” because of their chemical composition • Esters had a slow onset and short half life so they did not last long History • Derivatives of esters called “amides” were developed in the 1930’s • Amides had a faster onset and a longer half life so they lasted longer • AidAmides quiklickly repldlaced esters • In dentistry today, esters are only found in topical anesthetics Generic Local Anesthetics • There are five amide anesthetics used in dentistry today. Their generic names are; – lidocaine – mepivocaine – bupivacaine – prilocaine – artica ine • Each is known by at least one brand name Brand Names • lidocaine : Xylocaine, Lignospan, Alphacaine, Octocaine • mepivocaine: Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest • prilocaine : Citanest, Citanest Forte • bibupivaca ine: MiMarcaine • articaine: Septocaine, Zorcaine About Local Anesthetic (LA) • Local anesthetic (LA) works by binding with sodium channels in neurons preventing depolarization • LA is inactivated at the injection site when it is absorbed into the blood stream and redistributed throughout the body • If enough LA is absorbed, sodium channels in other parts of the body will be blocked, causing systemic side effects About LA • A clinical effect of LAs is dilation blood vessels, speeding up absorption and distribution • To counteract this dilation so anesthesia is prolonged, , a vasoconstrictor is often added to LAs • However, vasoconstrictors have side effects also Metabolism and Excretion • Most amide LAs are metabolized (inactivated) by the liver and excreted by the kidneys. • Prilocaine is partially metabolized by the lungs • Articaine is partially metabolized by enzymes in the bloo d as well as the liver. -

Efficacy of 2% Lidocaine and 4% Articaine in Mandibular Molars with Different Pulp Diagnoses in the Mandibular Technique1
Efficacy of 2% lidocaine and 4% articaine in mandibular molars with different pulp diagnoses in the mandibular technique1 Eficacia de la lidocaína al 2% y la articaína al 4% en molares mandibulares con diferentes diagnósticos pulpares en la técnica mandibular1 Adel Martínez Martínez2, Evelyn Freyle Granados3, Natalia Senior Carmona3 1 Paper submitted in partial fulfillment of the requirements for the degree of Endodontist 2 Assistant Professor, GITOUC Group, School of Dentistry, Universidad de Cartagena 3 DDS, Specialist in Endodontics, Postgraduate program in Endodontics, School of Dentistry, Universidad de Cartagena ABSTRACT Introduction: the inferior alveolar dental nerve block is the method most commonly used by endodontists to achieve local anesthesia during treatments. This study compared the efficacy of two anesthetic solutions: 2% lidocaine with 1:80,000 epinephrine and 4% articaine with 1:100,000 epinephrine in patients with different ARTICLES ORIGINAL pulp diagnoses requiring endodontic treatment. Method: an interventional, randomized clinical trial. The sample included 36 patients who were treated at the postgraduate endodontics service at the Universidad de Cartagena in the year 2016. Descriptive statistics and the Chi2 test were used for data analysis, using a limit of 0.05. Results: articaine showed a greater anesthetic effect in vestibular mucosa (88.9%) and tip of tongue (55.6%), compared with lidocaine. The rates of anesthetic success in the lidocaine and articaine groups were 5.6% and 22.2% respectively, but this difference was not statistically significant (p = 0.633). In teeth with normal pulp, the efficacy was 27.3%, and this value considerably decreased in teeth with asymptomatic and symptomatic irreversible pulpitis, with percentages of 5.8% and 12.5% respectively, although this difference was not statistically significant (p = 0.276). -

Comparative Evaluation of Lignocaine, Articaine and Ropivacaine for Proximal Paravertebral Anaesthesia in Cattle S.D
International Journal of Science, Environment ISSN 2278-3687 (O) and Technology, Vol. 8, No 3, 2019, 674 – 679 2277-663X (P) COMPARATIVE EVALUATION OF LIGNOCAINE, ARTICAINE AND ROPIVACAINE FOR PROXIMAL PARAVERTEBRAL ANAESTHESIA IN CATTLE S.D. Chepte1, M.G. Thorat2*, S.P. Waghmare3, M.V. Ingawale4, S.P. Mehesare5 M.V. Joshi5 and F.A. Fani6 1PhD Scholar, 2Professor and Head, 3Hospital Superintendent, 4Assistant Professor and 5Rtd Professor and 6Hospital Registrar Department of Surgery and Radiology Post Graduate Institute of Veterinary and Animal Sciences, MAFSU Akola (M.S.) E-mail: [email protected] (*Corresponding Author) Abstract: Present study was conducted on 18 clinical case of cattle presented with various gastro-intestinal affections to TVCC, PGIVAS, Akola subjected for laparotomy surgical procedure. All clinical cases were randomly divided into three equal group (n=6) and proximal paravertebral nerve block was performed by using Lignocaine, Articaine and Ropivacaine. Comparative anaesthetic assessment of onset of action and duration of anaesthesia along with clinicophysiological parameters were evaluated. Keywords: Lignocaine, Articaine, Ropivacaine, Cattle, Paravertebral. INTRODUCTION Thoracolumbar paravertebral block is performed to anesthetize the surgical site for a flank laparotomy. This technique is preferable to infiltration anesthetic techniques because of the smaller volume of anesthetic agent required, production of a more extensive anesthesia of the abdominal wall and reduced postoperative swelling and hematoma (Rostami & Vesal 2011). In ruminants, flank region is the most common site for laparotomy; caesarian section, rumenotomy, intestinal obstruction, volvulus, ruminal fistula, foreign body syndrome and hernia etc. (Lee, 2006; Kumar, 2003). Paravertebral nerve block results effective analgesia in all layers of the abdominal wall while the tissue infiltration, inverted L block may not produce analgesia of all muscle layers as well as peritoneum specially in fat animals (Sloss and Dufty, 1977). -

Anesthesia for Dental Treatment? Anesthesia Is Used to Help Manage Pain During Surgical Or Dental Procedures and Is an Integral Part of Dental Care
Anesthesia for Dental Treatment bcbsfepdental.com Learn more about reasons for use, types, and side effects of anesthesia Why Anesthesia for Dental Treatment? Anesthesia is used to help manage pain during surgical or dental procedures and is an integral part of dental care. Most of us are familiar with Novocain or lidocaine – a local anesthetic used to numb a treatment area – but did you know there are other reasons a dentist might recommend a different type of anesthesia? Dentists will determine which type of anesthesia is appropriate based on: • The complexity of the procedure (how invasive or the length of time to complete procedure) • The age of the patient and level of patient cooperation (small children, special needs, dementia/Alzheimer’s) Risks of Anesthesia • Patient medical history (allergies, special needs, Though complications from dental Parkinson’s) anesthesia are rare, there are some risks involved, including: • Patient mental health history (phobias, anxiety) • Allergic reactions Types of Anesthesia • Low blood pressure • Heart attack/failure Anesthesia options are broken into three categories: • Stroke Local Anesthesia – the most commonly used anesthetic, • Breathing failure local anesthesia is used to numb a specific area of the • Death mouth and are applied topically or by injection. Both the If you are planning dental treatment pre-injection numbing gel the dentist uses (topical using anesthesia, discuss any anesthetic) and the Novocain/lidocaine shot itself are concerns with your dentist. different examples of local anesthetics. Local anesthesia is used for minor dental procedures like fillings, extractions, root canal treatments, crown placement, and deep cleanings. The numbing sensation can last for hours, but leaves the patient conscious. -

Dental Anesthesia Division & the Dental Anesthesia Residency
Dental Anesthesia Division & the Dental Anesthesia Residency Program The Division of Dental Anesthesia is responsible for providing anesthesia to pediatric and adult patients who require dental rehabilitation, dental alveolar surgery, treatment for facial trauma and treatment for orthognathic surgery. A major responsibility for this division is providing care for pre-cooperative children and children and adults with special needs. The Division of Dental Anesthesia has three members: Dr. Martin Boorin, Dr. Ralph Epstein & Dr. Robert Reiner. Ralph Epstein, DDS Program Director The Division of Dental Anesthesia is responsible for a 3-year accredited dental Chief of anesthesia residency program which accepts 4 residents per year. Following Dental Anesthesia completion of the residency program these dentist anesthesiologists provide anesthesia for patients receiving dental and oral surgical care in multiple venues, i.e., office-based, ambulatory surgical centers, and hospitals. In addition, many of our graduates join the faculty of dental schools to provide didactic and clinical education to pre-doctoral students and post- doctoral residents in multiple specialties. Our graduates have accepted positions in states throughout this country and in Canada. During their training, the dental anesthesia residents are responsible for providing anesthesia care for all types of medical procedures. They are scheduled in a similar way to the physician anesthesia residents except they are not scheduled in the cardiac or obstetric rotations. A major part of the clinical portion of the anesthesia residency program is spent with Dr. Boorin and Dr. Epstein in dental and oral surgery offices providing the full spectrum of anesthesia care in an office-based venue. -

F 009 035 Benzocaine 20%, Lidocaine Hydrochoride 7
MEDISCA® NETWORK INC. TECHNICAL SUPPORT SERVICES FORMULATION CHEMISTRY DEPARTMENT TOLL-FREE: 866-333-7811 TELEPHONE: 514-905-5096 FAX: 514-905-5097 [email protected] 1/4/2021; Page 1 Suggested Benzocaine 20%, Lidocaine Hydrochloride 7%, Tetracaine Hydrochloride 7% FIN F 009 035 Formula Topical Gel (Suspension, 30 g) SUGGESTED FORMULATION Lot Expiry Ingredient Listing Qty. Unit NDC # Supplier Number Date Benzocaine, USP 6.000 g Lidocaine Hydrochloride, USP TBD Tetracaine Hydrochloride, USP 2.100 g Polysorbate 80, NF 0.5 mL Ethoxy Diglycol, NF 0.5 mL Medisca VersaPro™ Anhydrous Base 1.50 g Medisca VersaPro™ Anhydrous Base TBD MEDISCA® NETWORK INC. TECHNICAL SUPPORT SERVICES FORMULATION CHEMISTRY DEPARTMENT TOLL-FREE: 866-333-7811 TELEPHONE: 514-905-5096 FAX: 514-905-5097 [email protected] 1/4/2021; Page 2 Suggested Benzocaine 20%, Lidocaine Hydrochloride 7%, Tetracaine Hydrochloride 7% FIN F 009 035 Formula Topical Gel (Suspension, 30 g) SPECIAL PREPARATORY CONSIDERATIONS Ingredient-Specific Information Benzocaine, Tetracaine Hydrochloride, Polysorbate Light Sensitive (protect from light whenever possible): 80 Tetracaine Hydrochloride, Polysorbate 80, Ethoxy Hygroscopic (protect from moisture whenever possible): Diglycol Oxygen Sensitive (protect from air whenever possible): Polysorbate 80 Narrow Therapeutic Index Lidocaine Hydrochloride Suggested Preparatory Guidelines ■ Non-Sterile Preparation □ Sterile Preparation Processing Error / To account for processing error considerations during preparation, it is suggested to Testing Considerations: measure an additional 12 to 15% of the required quantities of ingredients. Special Instruction: This formula may contain one or more Active Pharmaceutical Ingredients (APIs) that may be classified as hazardous, please refer & verify the current NIOSH list of Antineoplastic and Other Hazardous Drugs in Healthcare Settings. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group.